Abstract
Objective
In a developing country like India, tuberculosis is very common in spite of a mass vaccination programme. Meningitis, progressive arteritis, adhesive arachnoiditis and tuberculomas represent the wide spectrum of this potentially lethal disease. Hydrocephalus occurs in about one third of the patients with central nervous system tuberculosis. Majority of patients have large fourth ventricles with adhesive obstructions in the basal cerebrospinal fluid (CSF) cisterns. Aggressive CSF diversion does not always alter the course of the disease. Endoscopic procedures are rarely, if ever, successful. Ventriculo-peritoneal shunting is fraught with complications like high rate of infection and shunt tube blockage. So there is clearly a need to explore methods of CSF diversion.
Methods
In our series of 32 patients, we present the indications, prognostic indicators and types of shunt with the clinical outcome of childhood tuberculous meningitis.
Conclusions
Even though the results are far from satisfactory, early shunting still remains the best option to prevent long-term neurological sequelae.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis remains a deadly disease in the developing world and in conjunction with HIV infections, it is also spreading to other parts of the world. It has been declared as a public health emergency in 1993 by the World Health Organization (WHO). As per the WHO report in 2005, the incidence of tuberculosis in India is 168 per 100,000 population, the prevalence is 299 per 100,000 population and the mortality rate is 29 per 100,000 population. This is in spite of an effective chemotherapy regime in place. Multidrug-resistant tuberculosis is also increasingly being reported in the paediatric population. Among the lethal spectrum of complications in childhood tuberculosis, meningitis ranks first with a death rate of ten per 100,000 in children below 4 years of age [5]. Hydrocephalus is a sinister sequela of meningitis in this group. In this study, we retrospectively analysed data of 32 children with hydrocephalus due to tuberculous meningitis at the Park Children’s Centre in Calcutta between 2003 and 2006.
Pathophysiology
Tuberculous meningitis develops from secondary spread from an extracranial focus, most commonly pulmonary. The spread occurs commonly within a year of primary infection. The intracranial focus, the so-called Rich focus, is usually subependymal or subpial. The focus ruptures to form exudates which settle in the basal meninges, invoking a hypersensitive reaction to the mycobacterial antigen. Along with that, progressive arachnoiditis and small vessel arteritis occur. The thick exudates block the subarachnoid cerebrospinal fluid (CSF) spaces, aqueduct or fourth ventricular outlets to cause hydrocephalus. In two thirds of the cases, the hydrocephalus is communicating and in others it is non-communicating. Hydrocephalus has been reported in 83% of children with tuberculous meningitis [14]. Patients with tuberculous meningitis are staged according to the Palur grading [13] (Table 1). Of the various methods available for CSF diversion, ventriculo-peritoneal shunt has been the most commonly practiced. The indications and timing of shunting, however, differ in literature and no consensus of opinion exists.
Materials and methods
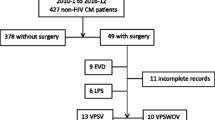
The study was a retrospective analysis of case records of children admitted in the departments of Neurosurgery and Pediatrics at the Park Children’s Centre, Calcutta, India. The period of study was 4 years (2003 to 2006). The select population was up to 12 years of age. The clinical profiles, operation records and follow-up data of 32 patients who underwent shunting following hydrocephalus for tuberculous meningitis were reviewed.
The diagnosis of tuberculous meningitis was established on the basis of clinical features of high fever, meningism, ocular abnormalities, positive history of tuberculosis and history of contact. The laboratory features were positive Mantoux test, lymphocytosis, hyperproteinemia and hypoglycoracchia. Computer tomography (CT) scan features considered suggestive of the pathology were enhancing basal cisterns suggestive of exudates.
The patients were graded according to the Palur grading. Only those in Palur grades II and III were included in the study.
All patients were started with anti-tuberculous chemotherapy regimen according to the Directly Observed Treatment, short course protocol followed in India. The drugs administered daily were isoniazid (20 mg/kg), rifampicin (20 mg/kg), pyrazinamide (40 mg/kg) and ethambutol (20 mg/kg). Specific side effects of the drugs were monitored regularly and dose adjustments made. Steroids were added routinely. The improvements of the patients were monitored clinically by improvement of CSF parameters and serial CT scans.
Only those patients with hydrocephalus either at the time of presentation or those who developed delayed features of hydrocephalus were included in this study. They were considered for ventriculo-peritoneal shunting if they were in Palur grade II or III. In grade I, neurological observation was done and in grade IV patients, only external ventricular drains were offered as first line therapy. They underwent a shunt if there was clinical deterioration with radiological documentation of increasing ventricular size. The CSF opening pressure was significantly high in 23 (71.9%) patients and normal in nine (28.1%) patients.
Ventriculo-peritoneal shunt was done using the Chhabra shunt system. The Chhabra shunt system used was a spring valve type of a differential pressure shunt [8]. There is a cylindrical side-walled slit valve that is housed in a stainless steel spring to protect the slit valve while maintaining the opening pressure. Medium- or low-pressure settings were used depending on the age of the child. Generally, low-pressure shunts were used if the age of the child was less than 1 year and medium-pressure shunts were used in older children.
Follow-up was done on an average of 6 months to 1 year on an inpatient and outpatient basis and the outcomes were assessed at the end of 6 months based on the Glasgow Outcome Scale (GOS). Other clinical and radiological parameters were also noted.
Results
There were 41 patients with tuberculous meningitis in grades II and III. Hydrocephalus was present in 37 of them (90.2%). Communicating hydrocephalus was found in 25 patients (78.1%) and 12 (21.9%) had non-communicating hydrocephalus. Thirty-two of them eventually underwent ventriculo-peritoneal shunts and their results will be further discussed.
The mean age of the patients was 6 years (range 1 month to 12 years). The majority age group was 3–7 years. There were 22 boys and ten girls. Twenty children (62.5%) were in Palur grade II and 12 (37.5%) were in grade III. The clinical features were depressed levels of consciousness in grade III patients, meningism in 27 (84.4%) and ocular motility disorders in 30 (93.8%). Papilledema was found in older children but since it was not recorded in neonates, the incidence is not included in the statistics. Motor weakness was found in 13 children (40.6%). Hydrocephalus was present in the CT scan at the time of referral in 26 patients (81.3%) and delayed progressive hydrocephalus was seen on serial scanning in six patients (18.7%). Thirteen patients (40.6%) had infarcts in CT scans, mostly (8 = 61.5%) single and in the rest there were multiple infarcts. Ventriculo-peritoneal shunting was done by both authors using the same type of shunt. Low-pressure shunts were used in six (18.8%) patients and in the rest (26, 81.2%) medium-pressure shunts were used. Shunt infection was found in five patients (15.6%) during the follow-up period. Shunt revisions due to blockade were observed in 14 (43.8%) patients. Multiple revisions were done in six (18.7%) patients. The Glasgow Outcome Score at 6 months (Table 2) showed good outcome in eight (25%) children, moderate disability (of cognition and ocular motility disorders) in 15 children (46.9%), severe disability in five (15.6%), vegetative state in one (3.2%) and death in three patients (9.3%). Patients in Palur grade II had comparatively better outcomes in each grade.
Discussion
Hydrocephalus following tuberculous meningitis is one of the common causes of neurosurgical referrals in the developing world where tuberculosis is rampant. Often one encounters a sick, irritable child with occasional extensor posturing and profound oculo-motor signs. The subarachnoid space is filled with tuberculous exudates precluding the possibility of a successful endoscopic third ventriculostomy. The only option is a ventriculo-peritoneal shunt whose efficacy seems doubtful in the face of high CSF protein. Even when the shunt works, the clinical outcome is unpredictable due to spreading vasculitis.
Hydrocephalus in tuberculous meningitis is a common complication and the incidence in literature ranges from 59% to 85% [7, 9]. Majority of the hydrocephalus (78.1% in our series) are communicating, indicating a subarachnoid block. Others with non-communicating variety, however, fare much worse [1]. Lampretch et al. [12] advocate that in cases with communicating hydrocephalus, shunting should be done in cases of failed medical management or progressive rise in intracranial tension. However, in that series, the communicating group fared much worse than the non-communicating group (18.5% death compared to 7.9%). Goel [10] and Arimoto et al. [2] had advocated monitoring of intracranial pressure and CSF TB PCR respectively before determining the optimal timing of shunting both of which, in our opinion, is impractical in our country. We believe that even in the communicating cases, early CSF diversion minimises intracranial damage, with better long-term clinical and cognitive outcome. Palur staging [13] offers some standard protocol for management of hydrocephalus and indeed it has been successfully proven in all series including ours that the overall outcome fares inversely with Palur clinical grading. The corollary is that the patients with radiological evidence of vasculitis in the form of infarcts do far worse. Shunting may alleviate part of their problem but the progressive arteritis and cranial nerve paresis makes the outcome dismal. All nine of our patients with GOS 1–3 had infarcts in their scans. Selection of shunt system is an issue in these trying conditions. The Chhabra shunt system with added manual compression of the chamber has been shown to drain proteinaceous debris and acts well in tuberculous meningitis [2]. We generally, however, avoid pumping of shunt valve as we fear the risk of migration and indrawing of chorid plexus in the tube. Nevertheless, high incidence of blockade is still seen commonly after 3–6 months requiring one or multiple revisions. The other limiting factor in these children is that the tuberculous peritonitis may hinder distal absorption. In that situation, ventriculo-atrial shunting is advocated by some [3] though it is proved to cause systemic dissemination of the disease. Endoscopic third ventriculostomy is a good option and the results are encouraging in early studies [11]. In our small experience of endoscopic procedures in acute cases, we had found the procedure to be hazardous as the floor is opaque, hard to perforate and there is increased vascularity of the floor of the third ventricle. The future is unpredictable as the distal subarachnoid space may be blocked. The incidence of shunt infection in our series is approximately the same as in other series [1, 4, 12]. Interestingly, the incidence of shunt infection in tuberculous meningitis is close to the incidence of shunt infections in other cases of hydrocephalus at our centre. We attribute this paradox to the rifampicin used in tuberculous meningitis patients which has reasonable anti-staphylococcal properties.
Our series present comparable presentations and results of treatment of hydrocephalus following tuberculous meningitis with results from the series of Yaramis and Chan [6, 15]. Retrospective analysis of the group who had dilated ventricular system but did not improve with shunt surgery suggests there exists a group of children who have dilated ventricular system but the CSF pressure is low (as documented at the time of surgery). None of the patients whose CSF pressure was low at the time of surgery improved after shunt surgery. Hence, we have modified our practice to perform ventricular drainage by external ventricular drain in all patients with hydrocephalus. We then go on to do the shunts in children who have clinical and radiological signs of improvement.
Conclusions
Hydrocephalus following tuberculous meningitis will continue to torment the neurosurgeon for a long time though epidemiological evidence points to plateauing in incidence of the disease. Ventriculo-peritoneal shunt will remain as the only armamentarium in the arsenal of the neurosurgeon for treating this disease even if it gets replaced by third ventriculostomy in treatment of other forms of hydrocephalus. Search for better shunts equipped to handle protein load is probably the only ray of hope.
References
Agrawal D, Gupta A, Mehta VS (2005) Role of shunt surgery in pediatric tubercular meningitis with hydrocephalus. Indian Pediatr 47:245–50
Arimoto A, Yoshioka H, Kihara M, Yagi T, Sawada T (1998) Tuberculous meningitis with hydrocephalus. Contribution of PCR assay of CSF before VP shunting. Childs Nerv Syst 14:623–626
Bhagwati SN (1971) Ventriculo-atrial shunting in tuberculous meningitis with hydrocephalus. J Neurosurg 35:309–313
Bullock MRR, Van Dellen JR (1982) The role of cerebrospinal fluid shunting in tubercular meningitis. Surg Neurol 18:274–277
Chakraborty AK (2000) Estimating mortality from tuberculous meningitis in a community: use of available epidemiological parameters in Indian context. Ind J Tub 47:9–13
Chan KH, Cheung RTF, Fong CY, Tsang KL, Mak W, Ho SI (2003) Clinical relevance of hydrocephalus as a presenting feature of tuberculous meningitis. K J Med 96:643–648
Clark WC, Metcalf JC, Muhlbauer MS et al (1986) Mycobacterium tuberculosis meningitis: a report of twelve cases and literature review. Neurosurgery 18:604–610
Czosnyka Z, Czosnyka M, Richard HK, Pickard JD (1998) Chhabra hydrocephalus shunt: lessons for gravitational valves. J Neurol Neurosurg Psychiatr 65:406–407
Gelabert M, Castro-Gago M (1988) Hydrocephalus and tuberculous meningitis in children. Childs Nerv Syst 4:268–270
Goel A (2004) Tuberculous meningitis and hydrocephalus. Neurol India 52(2):155
Jonathan A, Rajsekhar V (2005) Endoscopic third ventriculostomy for chronic hydrocephalus after tuberculous meningitis. Surgical Neurol 63:32–35
Lampretch D, Schoeman J, Donald P, Hartzenberg H (2001) Ventriculoperitoneal shunting in childhood tuberculous meningitis. Br J Neurosurg 15(2):119–125
Palur R, Rajsekhar V, Chandy M et al (1991) Shunt surgery for hydrocephalus in tuberculous meningitis: a long term follow-up study. J Neurosurg 74:64–69
Schoeman JF, Van Zyl LE, Laubscher JA, Donald PR (1995) Serial CT scanning in childhood tuberculous meningitis: prognostic factors in 198 cases. J Child Neurol 10:320–329
Yaramis A, Gurkan F, Elveli M, Soker M, Kenana H, Kirbas G et al (1998) Central nervous system tuberculosis in children: a review of 214 cases. Pediatrics 102(5):e49 PMID-9794979
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sil, K., Chatterjee, S. Shunting in tuberculous meningitis: a neurosurgeon’s nightmare. Childs Nerv Syst 24, 1029–1032 (2008). https://doi.org/10.1007/s00381-008-0620-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0620-x