Abstract
Introduction
While raised intracranial pressure (ICP) is a well recognized complication affecting children with syndromic craniosynostosis, certain percentage of the patients with non-syndromic craniosynostosis may have some problems related to increased ICP, such as developmental delay or visual problem. However, it is still not clear how many percent of and/or which types of craniosynostosis patients suffer from those symptoms, especially in older patients.
Objective
The aim of this study was to examine the ICP of older children with mild form of craniosynostosis to determine if any of them should be surgically treated.
Materials and methods
We measured ICP before making the decision for surgical intervention.
Results
Twenty-five of thirty-six patients had raised ICP in our series.
Discussion
All of the 25 patients were treated surgically and followed-up after more than 1 year. All patients improved in some degree. Further investigations should be performed to determine what is the threshold for raised ICP in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the first description by Virchow [16] in 1851, caraniosynosotosis has been considered as a premature fusion of skull suture, which occur early in fetal development. Then it has been thought that early diagnosis may lead the early surgical intevention resulting in a good surgical outcome. However, recent investigations suggest that some of the patients with mild form of craniosynostosis may develop their symptoms relatively late. In this paper, we present our results of ICP measurement in mild form of carniosynostosis in older children. Twenty-five patients out of thrity-six had increased ICP. Based on these results, we performed cranial expansion in 25 patients who improved in some degree after surgery. While the younger patients tended to improve in speech, the older patients improved in behavior. Because in this series the definition of raised ICP may be high for toddlers, further investigation will be needed to determine the borderline between normal and increased ICP in children.
Materials and methods
Patients population
All patients in this study were referred to our institute by pediatric neurologists or local general pediatricians for evaluation. Most of the patients in this study were diagnosed with mild developmental delay and/or learning disability by their clinicians, initially. Inclusion criteria were as follows: there is a possibility of craniosynostosis, there is no possible cause of developmental delay other than craniosynostosis, recommended for further investigation by their pediatricians, full agreement for enrolling the children to this study by parents (mandatory). Exclusion criteria were as follows: obvious craniosynostosis (typical) cases that were not detected early for any reason, other cause of mental delay suspected or confirmed by their physicians, only one caretaker’s agreement for enrolling their child to this study. Thirty-six patients with mild form craniosynostosis were included in this study, and all patients were followed-up more than 1 year after surgery. If the ICP was high, we performed cranial expansion using either conventional technique or gradual distraction technique.
Intracranial pressure monitoring
We measured the intracranial pressure (ICP) via lumbar tap under general anesthesia (Tables 1 and 2) based on the parents’ preference as the first step. If the ICP via lumbar tap is high or the parents preferred this as a first step, we measured the ICP via epidural monitoring with a CodmanR pressure sensor (MicroSensor™, Johnson and Johnson, Raynham, MA, USA), which was attached to the CodmanR ICP Express™ (Johnson and Johnson, Raynham, MA, USA). If the epidural ICP, which measured continuously in the operative room at least 30 min under the general anesthesia, was high, the patients received cranial expansion at the same time. If the ICP measured in the operative room was not high enough, we measured the ICP for at least 3 days in the ward. Initially, we planned to monitor ICP continuously in the ward but it turned out to be impossible because of the hyper-activity of the patients. We then measured the ICP when the patients were well sleeping and also noted the eye movement and the posture of the patients. When the patients were sleeping on their back and there was no eye movement, we considered this as the quiet ICP. In case the ICP measurement was low, we sent the patients to a pediatric neurologist for further follow-up.
Definition of raised ICP
We obtained the permission from the ethic committee in our institute to perform the surgical intervention if the patients showed increased ICP, as high as mentioned in well-accepted papers. We considered the raised ICP if it was higher than 18 mmHg in systolic (and/or 15 mmHg in mean). It was considered borderline if it was between 14 and 18 mmHg in systolic pressure in this study.
Operative procedure
In cases of mild form of craniosynostosis such as mild metpic suture synostosis, mild bicoronal synostosis, and mild form of multiple sutures, involvement was treated with gradual distraction procedure. In case of mild form of sagittal synostosis, gradual distraction methods or conventional cranial expansion were selected. The reason why conventional cranial expansion was performed less frequently in this series was the possible reduction in the chances of blood transfusion in gradual distraction methods than in conventional methods; the purpose of these procedures in this series was normalizing the ICP with cranial expansion; there was no need to reshape the cranial vault in most cases.
Result
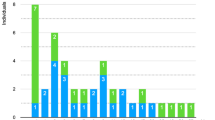
Twenty-five out of thirty-six cases had raised ICP; we performed cranial vault expansion as described above. We followed them at least more than a year either ourselves and/or pediatric neurologist or pediatric phychiatrist after cranial expansion. All patients improved in some degree. It is very interesting to note that even DQ (not performed systematically) showed almost no improvement in some cases, their behavior and/or verbal response to the parents and/or teachers in school improved dramatically. The younger patients showed the better outcome. There was a tendency that the younger patients showed the improvement in speech and older patients improved in behavior. In some cases, the craniogram and/or 3D-CT were not reliable enough to tell if patients have raised ICP before surgery. For example, while in some cases the craniogram showed fingerprinting and/or 3D-CT revealed the keel formation at the site of suture, the intracranial ICP was not high; in the others who showed no indication of raised ICP on either craniogram or 3D-CT had raised ICP.
Discussion
As we presented in the Asian Pacific Craniofacial Association Conference in 2002, we realized that some patients with craniosynostosis started to improve their behavior after surgical intervention even if they were older than 4 years old. After our own experience with several children with mild form of craniosynostosis in whom we found dramatic improvement after surgical intervention, the following question arose: how can such children be monitored so that they do not develop severe consequences of increase ICP? To answer this question, we performed serial ICP monitoring before making a decision to perform surgery. Shimoji et al. [14] also stated that some patients with mild form of craniosynostosis such as mild trigonocephaly rapidly improved in both or either motor and mental development after cranial expansion. In this paper, we describe the results of our investigation, which tried to understand if or in which patients we should perform surgical intervention for mild form of craniosynostosis. The questions to be answered are as follows: if we could predict raised ICP based upon the information from neuroradiological examination in those patients, is the ICP measurement via lumbar tap as reliable as continuous intracranial ICP measurement? How many of those patients have raised ICP? Is surgical intervention beneficial for those patients who are older than 2 or 3 year old?
Nonsyndromic caniosynostosis has been considered as a morphologic disorder. However, recent studies showed that it is not rare that affected children showed learning problem or mental retardation. Moreover, the brain dysfunction may become evident with time in patients with nonsyndromic craniosynostosis [3, 7, 8, 11, 13]. It is however unclear how nonsyndromic craniosynostosis affects brain function in older children. The long-term effects of nonsyndromic craniosynostosis on complex brain function is not clear because of the absence of outcome study [2]. In this investigation, we tried to obtain the following information: if there were any indication for surgery for the mild form of craniosynostosis, if any of those patients had raised ICP, and if the surgical intervension led to a better outcome in those older children with mild form of craniosynostosis. Our results in this paper showed that if the ICP was high, the surgical intervention should be done even if the patients were older than 4 or 5 years old. Before this study, we thought that if the children were old there would be no surgical indications even if the ICP were relatively high. We considered that the condition of untreated craniosynostosis in older children might be similar to those so-called arrested hydrocephalus in older children or adults. However, our results showed that normalized or decreased ICP with cranial expansion led to the improvement of the patients’ condition. Because we did not operate those children without raised ICP, it is not clear that raised ICP is the direct cause of damaged brain function in our cases.
ICP monitoring
The biggest problem in evaluating our results is the definition of normal ICP. Though the extensive works of measuring the ICP in the patients with craniosynostosis had been done, there was no well-accepted scale of normal ICP in children. Most accepted ICP value might be the statement of Minns [9]. The author stated normal ICP as 3.5 mmHg in neonates, 5.8 mmHg in infants, 6.4 mmHg in children, and 15.3 mmHg in adolescents and adults based on the review of previous papers. On the other hand, the other authors [5, 6, 10] stated that normal ICP in children older than 1 year of age should be considered as the same as adult patients in whom ICP is considered abnormal if it is higher than 15 mmHg.
We found that the ICP measurement via lumbar tap is not so reliable as the one measured via epidural; the epidural ICP measurement under general anesthesia was also less reliable in the continuous measurement in the ward.
ICP and radiological findings
Traditionally, we tend to think that it might be easy to tell which patients have increased ICP based on the findings of craniogram or 3D-CT. However, our results in this study showed that there was less correlation between neuroradiological findings and ICP than our initial thought. There are some possibilities to explain the gap between neuroradiological findings and ICP. For the patients with fingerprinting with normal ICP: Those patients might have raised ICP if we measured ICP when they were much younger. Long lasting raised ICP resulted in the less elastic brain, which showed normal ICP. Negative neuroradiological finding with high ICP: it is not statistical data but we assumed that the thickness of the skull in those patients might be the key. In some cases, we found the skull was very thick and hard for their age.
The reason of delayed diagnosis
In our series, the patients were not diagnosed before 2 years of age. According to their parents, there were no recognizable problems in their child’s development in the first year of age. Connolly et al. [4] presented a paper in which they observed two groups of patients with syndromic craniosynostosis. One group exhibited an unusual form of craniosynostosis, progressive postnatal craniosynostosis. In this group, they found that the patients in this group had normal skull shape and suture at birth. However, with time, they developed craniosynostosis. There is some possibility that the same phenomenon occurred in the simple form of craniosynostosis in our series. That may be a reason why the patients in our series were not diagnosed early.
Cognitive function and ICP
Increased ICP is an important factor for the development in craniosynostosis patients. The risk of increased ICP was dependent on the number of involved sutures. They demonstrated that 47% of the patients with multisuture involvement showed increase ICP, only 14% of the patients with single suture involvement showed increase ICP [12]. It has been reported previously that the increased ICP occurred in 13% of scaphocephaly [1].
Speltz et al. [15] reviewed 17 studies examining the neuropsychological status of children with simple form craniosynostosis. The majority of children in these studies demonstarated global developmental or IQ scores within normal range. However, 35–40% of the assessed cases demonstrated some types of adverse neurodevelopmental outcome such as a learning disability, language impairment, behavioral or cognitive abnormality [8]. There is little information that shows direct correlation between the state of ICP and mental development or cognitive function in mild nonsyndromic craniosynostosis. All patients in this paper improved after surgery in some degree either in behavior or speech, though there is no statistical improvement in DQ. Table 3 shows a part of letters from some parents and teachers of their school. There was a tendency that the younger patients, the better outcome. While the younger patients improved in speech, the older patients improved in behavior. A standardized, long-term, prospective study of cognitive, speech and behavioral functioning will be required to determine if the raised ICP in those children is the direct adverse effect to the developing brain.
References
Arnaud E, Renier D, Marchac D (1995) Prognosis for mental function in scaphocephaly. J Neurosurg 83:476–479
Becker DB, Petersen JD, Kane AA, Cradock MM, Pilgram TK, Marsh JL (2005) Speech, cognitive, and behavioral outcomes in nonsyndromic craniosynostosis. Plast Reconstr Surg 116:400–407
Bottero L, Lajeunie E, Arnaud E, Marchac D, Renier D (1998) Functional outcome after surgery for trigonocephaly. Plast Reconstr Surg 102:952–958 (discussion 959–960)
Connolly JP, Gruss J, Seto ML, Whelan MF, Ellenbogen R, Weiss A, Buchman SR, Cunningham ML (2004) Progressive postnatal craniosynostosis and increased intracranial pressure. Plast Reconstr Surg 113:1313–1323
Eide PK, Helseth E, Due-Tonnessen B, Lundar T (2001) Changes in intracranial pressure after calvarial expansion surgery in children with slit ventricle syndrome. Pediatr Neurosurg 35:195–204
Gambardella G, Zaccone C, Cardia E, Tomasello F (1993) Intracranial pressure monitoring in children: comparison of external ventricular device with the fiberoptic system. Childs Nerv Syst 9:470–473
Gripp KW, McDonald-McGinn DM, Gaudenz K, Whitaker LA, Bartlett SP, Glat PM, Cassileth LB, Mayro R, Zackai EH, Muenke M (1998) Identification of a genetic cause for isolated unilateral coronal synostosis: a unique mutation in the fibroblast growth factor receptor 3. J Pediatr 132:714–716
Kapp-Simon KA (1998) Mental development and learning disorders in children with single suture craniosynostosis. Cleft Palate Craniofac J 35:197–203
Minns RA (1984) Intracranial pressure monitoring. Arch Dis Child 59:486–488
Pople IK, Muhlbauer MS, Sanford RA, Kirk E (1995) Results and complications of intracranial pressure monitoring in 303 children. Pediatr Neurosurg 23:64–67
Renier D, El-Ghouzzi V, Bonaventure J, Le Merrer M, Lajeunie E (2000) Fibroblast growth factor receptor 3 mutation in nonsyndromic coronal synostosis: clinical spectrum, prevalence, and surgical outcome. J Neurosurg 92:631–636
Renier D, Sainte-Rose C, Marchac D. and Hirsch.JF (1982) Intracranial pressure in craniosynostosis. J Neurosurg 57:370–377
Sidoti EJ Jr, Marsh JL, Marty-Grames L, Noetzel MJ (1996) Long-term studies of metopic synostosis: frequency of cognitive impairment and behavioral disturbances. Plast Reconstr Surg 97:276–281
Shimoji T, Shimabukuro S, Sugama S, Ochiai Y (2002) Mild trigonocephaly with clinical symptoms:analysis of surgical results in 65 patients. Childs Nerv Syst 18: 215–224
Speltz ML, Kapp-Simon KA, Cunningham M, Marsh J, Dawson G (2004) Single-suture craniosynostosis: a review of neurobehavioral research and theory. J Pediatr Psychol 29:651–668
Virchow,R (1851) Uever den Cretinismus, namentlich in Franken, und uer pathologische Schadelformen. Verh Phys Med Ges Wurzburg 2:230
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inagaki, T., Kyutoku, S., Seno, T. et al. The intracranial pressure of the patients with mild form of craniosynostosis. Childs Nerv Syst 23, 1455–1459 (2007). https://doi.org/10.1007/s00381-007-0436-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-007-0436-0