Abstract
Introduction
We report two cases of radiation-induced intracranial tumours after treatment for medulloblastoma presenting in children with nevoid basal cell carcinoma syndrome.
Discussion
These cases illustrate the need for judicious use of post-operative radiotherapy as secondary tumors are commonly reported. This is particularly important as the initial tumour in this cohort is of the ‘less aggressive’ desmoplastic subtype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nevoid basal cell carcinoma syndrome (NBCCS) is a syndrome inherited in an autosomal dominant fashion and is characterised by multiple jaw keratocysts and/or basal cell carcinomas that develop in the second and third decades of life, respectively [5]. Approximately 5% of the patients with NBCCS develop and require treatment for medulloblastomas [3]. We report radiation-induced tumours in two patients with NBCCS, who had medulloblastomas treated with surgery and radiotherapy. The implication for treatment in newly diagnosed patients and follow-up in treated patients is discussed.
Case histories
Patient 1
GC first presented, aged 15 months, with an enlarged head and a failure to thrive. Her early development (up to the age of 7 months) was normal, but since then, there had been no progress. On examination, she was noted to have a large head, bulging fontanelle and chronic papilloedema. She was admitted, and ventriculography revealed hydrocephalus as a result of a mass at the level of the fourth ventricle. She underwent a posterior fossa craniectomy and total excision of the mass. Histologically, the lesion was described as a cellular medulloblastoma with a lobular arrangement and glial differentiation. She recovered well from surgery and received cranio-spinal irradiation (30 Gy to the head and 45 Gy to the posterior fossa and spinal axis).
She was followed up as an outpatient and was diagnosed with Gorlin’s syndrome in 1991 aged 25 years. At this point, she was noted to have falcine calcification, bifid ribs, cleft palate, odontogenic keratocytes, multiple basal cell carcinoma and palmar pits. She had no evidence of intracranial pathology except falcine calcification, although she was noted to have marked learning difficulties. She exhibited a nonsense mutation (2842 A>T) in exon 16 of the PTCH gene on chromosome 9q22.3–q31, as did her father who also showed diagnostic features of NBCCS but was diagnosed after his daughter’s medulloblastoma diagnosis.
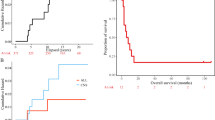
She represented to neurosurgery, age 38, 2 weeks after a fall. She was noted not to be using her right arm, and in retrospect, her carer reported that she had become more withdrawn over time. A CT scan performed to rule out any trauma-related pathology revealed space-occupying lesions consistent with multiple meningioma(s) (Fig. 1). Clinically, she had marked learning difficulties, with poor communication abilities and limited language. She had a thin scalp with multiple BCCs. She had a Glasgow Coma Score of 12 (E4, M5, V3). She had a mild right-sided weakness.
Patient 2
PC presented, aged 23 months, with a 3-week history of unsteadiness and falling. On examination, he was noted to have papilloedema and been markedly ataxic. A CT scan demonstrated hydrocephalus as a result of a posterior fossa tumour. He underwent excision of the posterior fossa mass, which histologically was described as a small, spindle, and polygonal celled medulloblastoma. He also received post-operative cranio-spinal radiotherapy. He was followed up and required excision of multiple scalp BCC 1991 and 1992. He was diagnosed as having the NBCCS on the basis of his medulloblastoma, palmar pits, calcified falx, multiple BCC and jaw keratocysts. After diagnosis of NBCCS in patient 2, it was possible to confirm the diagnosis in his asymptomatic mother. She had falx calcification, palmar pits, macrocephaly and BCCs, which she was unaware of, but were confirmed on histology. Patient 2 was lost to follow-up until he represented at 18 years after his initial consultation with a temporal lobe astrocytoma confirmed on biopsy (Fig. 2). Aside from learning problems, he was also small and had not entered puberty due to pituitary insufficiency. Despite molecular analysis of PTCH, no mutation was identified.
Discussion
We have presented two cases of post-radiation-induced tumours in patients with NBCCS after their initial intracranial surgery and cranio-spinal irradiation. These cases highlight a number of emerging issues that need to be considered in the management of patients with a medulloblastoma associated with NBCCS.
The main implications upon treatment and follow-up hinge around the atypical nature of medulloblastomas associated with NBCCS in that: (a) medulloblastomas as part of the NBCCS present at a median age of 2 years (compared to a peak incidence at 7 years for sporadic cases [1, 2] and (b) all of the 21 previously reported, histologically classified NBCCS-associated medulloblastomas were of the desmoplastic subtype [1]. This compares with the desmoplastic subtype making up about 20–34% of sporadic medulloblastomas [6]. Unfortunately, the tumours in this report were not histologically subtyped and only recorded as described above.
Implications
Diagnosis
NBCCS is diagnosed on the presence of two major and one minor, or one major and three minor criteria [5]. Presentation of a medulloblastoma aged below 2 years of age, particularly if it is of the desmoplastic subtype, should include examination and investigation of the criteria for diagnosis of NBCCS. Diagnosis at this age is hindered by the fact that many of the major diagnostic criteria do not present until the second decade of life [5]. However, NBCCS is an autosomal dominant disease, and therefore, a careful family history and examination of first-degree relatives may help to make an early diagnosis (both patients in this report had an affected parent). Molecular genetic studies may also be valuable in early diagnosis. In particular, PTCH gene mutations specifically have been associated with NBCCS. However, sequence analysis of exons 2–23 on chromosome 9 and mutation scanning of the PTCH coding region only detect mutations in 60–85% of patients with typical clinical findings of NBCCS; indeed, patient 2 with clear-cut NBCCS did not have a detectable mutation. This means that as yet, NBCCS cannot be excluded on the basis of negative molecular genetic testing [5]. The median reported time to diagnosis of NBCCS for patients who presented with a medulloblastoma is 5 years [1]. Whilst this may reflect the difficulty of early diagnosis, it probably also reflects the fact that the association of medulloblastoma presenting in children <3 years with NBCCS is still not recognised by many. Immediate or early recognition of whether an atypically presenting medulloblastoma heralds NBCCS may be important in guiding further therapy as discussed below.
Treatment
The overall outcome for treatment of medulloblastomas has improved such that the 5-year disease-free progression survival rate is about 70% [8]. Recent studies have identified age of presentation (children aged <3 years are twice as likely to progress over 5 years than those presenting with age >5 years), extent of disease and subtotal resection as important prognostic factors with contemporary therapy based on aggressive surgical removal followed by radiotherapy and chemotherapy [10, 14].
Cranio-spinal radiotherapy in particular is a highly effective therapy for both long-term survival and disease-free survival for medulloblastomas [8]. However, it is associated with significant morbidity particularly in children under 5 years of age, and complications include radiation-induced tumours, effects on pituitary function and/or neuropsychological disturbances as demonstrated by the above case studies [11]. These ‘toxic’ side effects of radiotherapy are increasingly recognised, and this has led to the treatment of medulloblastomas based on risk of recurrence (discussed above). In patients with ‘average’ risk, there is an increasing trend to treat with aggressive surgery, in combination with chemotherapy and reduced dose radiotherapy [8]. However, even reduced dose radiotherapy has been shown to have significant side effects [8, 11].
Adjuvant therapy with radiotherapy is of relevance in NBCCS for a number of reasons. Current opinion would dictate that all patients with medulloblastomas should receive adjuvant radiotherapy and chemotherapy to allow for optimal disease-free recurrence, although the timing of delivery of radiotherapy for patients <3 years old may be delayed due to the profound neuropsychological effects observed [8].
All the reported cases in the literature suggest that medulloblastomas associated with NBCCS are of the ‘desmoplastic’ variety [1]. These tumours are described to have a more ‘benign’ course despite presentation at an early age [7]. Furthermore, progression-free survival has been demonstrated in patients without radiotherapy. In a group of 11 patients diagnosed with a ‘nodular’ or ‘desmoplastic’ medulloblastoma with a median presentation age of 18 months and a median follow-up of 60 months, only three patients were treated with radiotherapy in addition to surgery and chemotherapy. Only 3/11 patients had a relapse, and all patients were alive at the median follow-up of 60 months (range 35–156 months) [7]. These data compare favourably to the overall median time to relapse of 9 months for medulloblastomas in patients aged 3 years after surgery and chemotherapy and suggest that NBCCS-associated medulloblastomas are of a more ‘benign’ nature [9]. This suggests that in a group of patients with ‘desmoplastic’ medulloblastomas, radiotherapy may be withheld.
Radiation-induced second malignancies are a significant risk to long-term survivors of childhood medulloblastomas. The relative risk of developing secondary malignancies is increased by 20 to 39-fold, with this risk being higher in those children who present before the age of 2 years as is common with NBCCS medulloblastomas [13]. The relative risk of intracranial radiation-induced neoplasms in NBCCS specifically has not been quantified. In the contemporary literature, we have observed that (including our report) 5/6 patients (7/8 including our report) with NBCCS-associated medulloblastoma developed a secondary intracranial tumour [1, 12, 13]. It is interesting to note that the only patient who did not develop secondary brain tumour was the one treated with surgery and chemotherapy alone and was in remission for 11 years. Radiation also has problems such that BCCs are almost certain to arise in the region of treatment of medulloblastoma and often do so when BCCs are treated. This is therefore a further reason why radiotherapy as treatment for BCC in NBCCS is not recommended [5]. Indeed, BCCs after cranio-spinal radiation may actually result in shortening of life span in addition to the adverse effects of multiple treatments on the quality of life [4].
Conclusion
Long-term survival is not an issue for patients with NBCCS. Given the problems of radiotherapy-associated secondary brain tumours, and that previous reports that suggested that this syndrome is associated with a less aggressive ‘desmoplastic’ tumour, we would advocate that early diagnosis of NBCCS should be sought and that radiotherapy should be deferred in those children presenting with desmoplastic medulloblastomas <3 years. Preferably, radiotherapy in a proven case of NBCCS should only be used as a second-line treatment if there is a failure to respond to chemotherapy or there is tumour recurrence.
References
Amlashi SF, Riffaud L, Brassier G, Morandi X (2003) Nevoid basal cell carcinoma syndrome: relation with desmoplastic medulloblastoma in infancy. A population-based study and review of the literature. Cancer 98:618–624
Cowan R, Hoban P, Kelsey A, Birch JN, Gattamaneni R, Evans DG (1997) The gene for the naevoid basal cell carcinoma syndrome acts as a tumour-suppressor gene in medulloblastoma. Br J Cancer 76:141–145
Evans DG, Farndon PA, Burnell LD, Gattamaneni R, and Birch JN (1991) The incidence of Gorlin syndrome in 173 consecutive cases of medulloblastoma. Br J Cancer 64:959–961
Evans DG, Birch JM, Orton C (1991) Brain tumours and the occurrence of severe invasive basal cell carcinomas in first degree relatives with Gorlin syndrome. Br J Neurosurg 5:643–646
Evans DG, Farndon, PA (2002) Nevoid Basal Cell Carcinoma Syndrome. http://www.genetests.org, 1-16. 6-10-0004. University of Washington, Seattle (Electronic Citation)
Gajjar A, Hernan R, Kocak M, Fuller C, Lee Y, McKinnon PJ et al (2004) Clinical, histopathologic, and molecular markers of prognosis: toward a new disease risk stratification system for medulloblastoma. J Clin Oncol 22:984–993
Giangaspero F, Perilongo G, Fondelli MP, Brisgiotti M, Carollo C, Burnelli R et al (1999) Medulloblastoma with extensive nodularity: a variant with favorable prognosis. J Neurosurg 91:971–977
Gilbertson RJ (2004) Medulloblastoma: signalling a change in treatment. Lancet Oncol 5:209–218
Heideman RL (2001) Overview of the treatment of infant central nervous system tumors: medulloblastoma as a model. J Pediatr Hematol Oncol 23:268–271
Kortmann RD, Kuhl J, Timmermann B, Mittler U, Urban C, Budach V et al (2000) Postoperative neoadjuvant chemotherapy before radiotherapy as compared to immediate radiotherapy followed by maintenance chemotherapy in the treatment of medulloblastoma in childhood: results of the German prospective randomized trial HIT ’91. Int J Radiat Oncol Biol Phys 46:269–279
Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE (2004) Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol 5:399–408
O’Malley S, Weitman D, Olding M et al (1997) Multiple neoplasms following craniospinal irradiation for medulloblastoma in a patient with nevoid basal cell carcinoma syndrome. Case report. J Neurosurg 86:286–288
Stavrou T, Bromley CM, Nicholson HS et al (2001) Prognostic factors and secondary malignancies in childhood medulloblastoma. J Pediatr Hematol Oncol 23:431–436
Zeltzer PM, Boyett JM, Finlay JL, Albright AL, Rorke LB, Milstein JM et al (1999) Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the Children’s Cancer Group 921 randomized phase III study. J Clin Oncol 17:832–845
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choudry, Q., Patel, H.C., Gurusinghe, N.T. et al. Radiation-induced brain tumours in nevoid basal cell carcinoma syndrome: implications for treatment and surveillance. Childs Nerv Syst 23, 133–136 (2007). https://doi.org/10.1007/s00381-006-0178-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-006-0178-4