Abstract
Object
The purpose of this study is to determine the epidemiology of tumors of the nervous system diagnosed according to the WHO 2000 classification in a single Brazilian institution.
Patients and method
One thousand one hundred ninety-five tumors in children between 0 and 21 years of age diagnosed between 1974 and 2003 were classified according the sex, topography, and age distribution.
Results
In all ages, males were slightly more affected. In the first 2 years, the prevalence for boys was higher (68.3%). In the whole series, 58.7% were supratentorial, 31.4% infratentorial, and 9.9% spinal (44% intra- and 56% extramedullary). Among these latter, ependymomas and schwannomas were the most frequent. In the cerebral compartment, pilocytic astrocytomas were the single most frequent tumors (18%), followed by diffuse astrocytomas (14%), medulloblastomas (11%), and craniopharyngiomas (11%). In the posterior fossa, there was an even distribution among medulloblastomas and pilocytic astrocytomas, but the former was much more frequent in the first 2 years of age. High-grade (III and IV) diffuse astrocytomas were slightly more frequent than low grades (II), and this difference becomes more evident as the child grows older. Due to the new development of the surgery of epilepsy, the frequency of neuronal and mixed neuronal–glial tumors is increasing (8%).
Conclusion
Classified according to the latest WHO classification, by a single neuropathologist in a single institution, this large series of pediatric neurological tumors may reflect fairly well their real incidence. Our results obtained in a developing country do not differ substantially from other similar series reported in the literature from the First World.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumors of the nervous system are the second commonest type of neoplasia of childhood after leukemia. The annual incidence varies between 1.7 and 4.1/100,000 children, and it seems that there is a slight increase in annual incidence for the last two decades [3, 5, 16]. In the USA, it is estimated that 2,200 children develop nervous system tumors each year [1]. Albeit the progress in early detection, surgical procedures, and therapeutic strategies, the overall prognosis of these tumors remains poor. In a recent study from the USA [2], only 33% of the patients were alive at follow-up 5 years after surgery. However, there are conspicuous differences as to prognosis among the nervous system neoplasms either according to the different histological types or their topography.
There are several reports regarding the epidemiology of tumors of the nervous system in children. However, most are based on population-based or institutional tumor registries [3, 7–9]. The major flaw of such studies concerns the fact that different classification schemes may have been adopted by the several institutions from which the data are taken. Also, two other issues concerning astrocytic tumors and medulloblastomas, which are the most frequent pediatric tumors, need to be clarified. In several reports, the former is taken as a whole, and medulloblastomas and primitive neuroectodermal tumors (PNETs) are considered the same type of neoplasm [14, 15, 17]. Actually, astrocytic tumors are a heterogeneous group of neoplasms with distinct biological behavior varying from grade I (pilocytic astrocytomas) to grade IV (glioblastoma multiforme) of malignancy. These different types of astrocytomas constitute distinct clinicopathological entities that must be individualized in the schemes dealing with these issues. As to the medulloblastoma/PNET issue, the current view of most neuropathologists including the WHO classification of tumors of the nervous system [4] considers these neoplasms as distinct entities whose propensity to occur in various sites within the neuroaxis, and the response to treatment is quite different. As with the astrocytic tumors, these neoplasms must appear under different headings in order to allow the actual detection of their incidence.
The present study is an epidemiological analysis of 1,195 consecutive tumors of the nervous system whose anatomopathological diagnosis was performed in a single institution by a single neuropathologist. It is worth mentioning that to our knowledge, this is the only study of this kind performed in a developing country so that it will be possible to compare the epidemiology of the pediatric tumors of the nervous system between different socioeconomic populations.
Patients and methods
One thousand one hundred ninety-five consecutive tumors of the nervous system in children from 0 to 21 years of age histologically diagnosed at the Division of Pathology of the Hospital das Clinicas of the São Paulo University School of Medicine between January 1974 and December 2003 were reviewed. In some cases, mainly in those whose diagnosis had been performed prior to the immunohistochemistry era, the initial diagnosis was remade with the utilization of this technique. Also, in 1998, a special cohort of tumors including embryonal and low-grade gliomas was reviewed in order to detect the recently recognized dysembryoplastic neuroepithelial tumor (DNT) [13]. The tumors were classified and graded according the WHO 2000 scheme [4]. Other recently described entities not yet contemplated in this classification were included.
Results
According to the gender, 54% of the tumors occurred in males and 46% in females. Of the tumors, 58.7% were situated in the supratentorial (ST) compartment, 31.4% in the infratentorial (IT), and 9.9% in spinal canal (SC). However, in the first 2 years of life (104 cases), 68.3% of the affected children were males. Fifty-eight cases (55.7%) were ST, 33 (31,8%) were IT, and 13 (12.5%) were spinal.
The histologic types of the spinal tumors are listed in Table 1. Of these, 44% were intramedullary (ependymoma being the most frequent tumor) and 56% were extramedullary, intra- or extradural. Peripheral nerve sheath tumors (mostly schwannomas) were by far the most frequent tumors of this region.
The histological types of the brain (intracranial) tumors are listed in Table 2. The topographic distribution plotted with the histological types were as follows: hemispheric=24.4% (diffuse astrocytomas=34.9%, ganglioglioma/gangliocytoma=16.7%, pilocytic astrocytoma=11.6%, DNT=5.4%, meningioma=6.6%, others=24.8%); lateral ventricles=7.8% (choroid plexus tumors=32.9%, ependymoma=23.2%, subependymal giant cell astrocytoma=14.6%, others=29.3%); basal ganglia/thalami=3.9% (diffuse astrocytomas=53.7%, pilocytic astrocytoma=22%, others=24.3%); selar=19% (craniopharyngioma=57.7%, pituitary adenoma=29.8%, germinoma=5.5%, others 6.9%); pineal region=3.3% (germinoma=25.7%, pineocytoma/pineoblastoma=20%, teratomas=14.3%, others=40%); hypothalamus/optic pathways=4.3% (pilocytic astrocytoma=89.1%, ganglionar hypothalamic hamartoma=10%); cerebellum/IV ventricle=30.9% (medulloblastoma=36.4%, pilocytic astrocytoma=31.5% ependymoma=17.4%, others=14.7%); brain stem=2.3% (diffuse astrocytomas=66.7%, pilocytic astrocytoma=16.7, others=16.6%); and base of the skull=4.1% (chordoma=18.6%, epidermoid cysts=7%, schwannoma=51.2%, others=23.3%).
According to their topography, the distribution of the main tumors was as follows: pilocytic astrocytoma (ST=41.8%, IT=51.9%, SC=6.3%), diffuse astrocytoma (ST=72%, IT=18.5%, SC=9.5%), ependymoma (ST=26.5%, IT=58.2%, SC=15.3%), ganglioglioma/gangliocytoma (ST=86%, IT=5.2%, SC=8.8%), choroid plexus tumors (ST=84.4%, IT=15.6%).
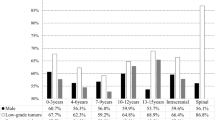
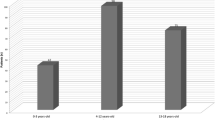
Figure 1 represents the distribution of the most frequent tumors through the patient’s ages. The distribution of the three types of diffuse astrocytomas, pilocytic astrocytoma, and ependymoma, as well as the cerebellar/IV ventricle tumors according to age, is shown in Figs. 2, 3, 4, 5.
Discussion
We think that our results reflect fairly well the incidence of tumors of the nervous system in childhood due to the fact that this study was performed through many years in a single institution with a homogeneous neuropathological approach. They do not differ substantially when compared with those of most series reported in the literature in which the methodology was similar to ours [11, 12].
In general, males are slightly more affected than females. However, in the first 2 years of life and between 2 and 5 years, respectively, about 68% and 60% of the cases occur in males.
It is commonly stated that in children, the tumors of the posterior fossa are more frequent than those arisen in the ST compartment. However, when reviews of population-based and institutional tumor registries are taken together [8, 9], it emerges that there is an even distribution among infra and ST tumors and, in some series, like ours, there is a predominance of the latter. This is particularly true when one considers the tumors in the first 2 years of life. At this period, 64% of the 91 intracranial tumors found in our series were situated in the ST compartment. However, the actual incidence of the tumors of the posterior fossa may be slightly higher than shown in our series because the majority of the brain stem tumors (glioma of the pons) are not biopsied. We estimate that these tumors represent 10 to 20% of those situated in the posterior fossa.
In the cerebellum, medulloblastomas and pilocytic astrocytomas are almost evenly distributed. However, in the first 2 years, the former is more frequent.
Pilocytic astrocytoma is the most frequent tumor of the nervous system in children performing almost one fifth of all neoplasms. More than half of them are cerebellar and they represent the vast majority of the tumors of the optic/hypothalamic region, almost one third of the cerebellar/IV ventricle, one fourth of the basal ganglia/thalamic, and 11% of the hemispheric tumors. Diffuse astrocytomas that are by far the most frequent tumor of the nervous system in adults represent almost 15% of all tumors in children. It is worth mentioning that high-grade tumors (grades III and IV) are as frequent as low-grade (grade II) tumors. Almost 90% of them are situated in the cerebral hemispheres or in the basal ganglia/thalamic region.
Due to the recent development of surgery of epilepsy techniques, neuronal and mixed neuronal–glial tumors perform a quite high percentage (8%) of the brain tumors in our series. The majority of these tumors are represented by gangliogliomas, gangliocytomas, and DNTs, which commonly lead to chronic intractable epilepsy.
Tumors recognized in the last quarter of the century are indeed very rare, DNT being the most frequent of them (n=14). The others included pleomorphic xanthoastrocytoma (n=6), atypical teratoid/rhabdoid tumor (n=3), desmoplastic infantile astrocytoma (n=3), and central neurocytoma (n=3). Cerebellar liponeurocytoma, choroid, and rhabdoid meningiomas have not been diagnosed. Other rare entities [6, 10] not yet contemplated in the WHO 2000 scheme are the ganglioneurocytoma, the ganglioneuroblastoma, and the papillary glioneuronal tumor. We found, respectively, 1, 3, and 0 cases of such tumors in our series.
We think that these data may reflect the real epidemiological status of pediatric brain tumors and that the incidence of these neoplasms in a developing country does not differ substantially from that found in first-world countries. This is another argument speaking against a possible role of environmental factors in the genesis of tumors of the nervous system.
References
Bleyer WA (1999) Epidemiologic impact of children with brain tumors. Childs Nerv Syst 15:758–763
Gurney G, Smith MA, Bunin GR (1999) CNS and miscellaneous intracranial and intraspinal neoplasms. National Cancer Institute SEER Pediatric monograph, pp 51–63
Kaatsch P, Rickert CH, Kuhl J, Schuz J, Michaelis J (2001) Population-based epidemiologic data on brain tumors in German children. Cancer 15:3155–3164
Kleihues P, Cavenee WK (2000) Tumours of the nervous system. World Health Organization classification of tumours. IARC Press, Lyon
Leviton A (1994) Principles of epidemiology. In: Cohen ME, Duffner PK (eds) Brain tumors in children, 2nd edn. Raven Press, New York, pp 27–49
McLendon RE, Provenzale J (2002) Glioneuronal tumors of the central nervous system. Brain Tumor Pathol 19:51–58
Miltenburg D, Louw DF, Sutherland GR (1996) Epidemiology of childhood brain tumors. Can J Neurol Sci 23:118–122
Nomura S, Nishizaki T, Yamashita K, Ito H (1998) Pediatric brain tumors in a 10-year period from 1986 to 1995 in Yamaguchi prefecture: epidemiology and comparison with adult brain tumors. Pediatr Neurosurg 28:130–134
Pollack IF (1994) Brain tumors in children. N Engl J Med 331:1500–1507
Prayson RA (2000) Papillary glioneuronal tumor. Arch Pathol Lab Med 124:1820–1823
Rickert CH, Probst-Cousin S, Gullotta F (1997) Primary intracranial neoplasms of infancy and early childhood. Childs Nerv Syst 13:507–513
Rickert CH, Paulus W (2001) Epidemiology of central nervous system tumors in childhood and adolescence based on the new WHO classification. Childs Nerv Syst 17:503–511
Rosemberg S, Vieira GS (1988) Tumor neuro-epitelial disembrioplástico. Um estudo epidemiológico de uma única instituição. Arq Neuro-Psiquiatr 56:232–236
Siffert J, Greenleaf M, Mannis R, Allen J (1999) Pediatric brain tumors. Child Adolesc Psychiatr Clin N Am 8:879–903
Sklar CA (2002) Childhood brain tumors. J Pediatr Endocrinol Metab 2:669–673
Smith MA, Freidlin B, Ries LA, Simon R (2000) Increased incidence rates but no space-time clustering of childhood astrocytoma in Sweden, 1973–1992: a population-base study of pediatric brain tumors. Cancer 15:1492–1493
Staneczec W, Janisch W (1994) Epidemiology of primary tumors of the central nervous system in children and adolescents. A population based study. Pathologe 15:207–215
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosemberg, S., Fujiwara, D. Epidemiology of pediatric tumors of the nervous system according to the WHO 2000 classification: a report of 1,195 cases from a single institution. Childs Nerv Syst 21, 940–944 (2005). https://doi.org/10.1007/s00381-005-1181-x
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-005-1181-x