Abstract
Objective
The objective was to evaluate cerebral hemodynamics in young children with acute subdural hematoma (SDH) and the impact of surgical treatment using transcranial Doppler (TCD).
Design
The design was a prospective study of infants with SDH requiring surgical evacuation.
Setting
The setting was the neuro intensive care unit of a university hospital.
Interventions
Indications for surgical evacuation were based upon clinical and radiological arguments. Surgery included emergency needle aspiration followed by external or/and internal shunting as required. A TCD evaluation was performed before needle aspiration, and after each surgical drainage procedure. It included a pressure provocation test to assess cerebral compliance. Preoperative and postoperative middle cerebral artery (MCA) velocities, Gosling pulsatility (PI) and Pourcelot resistivity (RI) indexes and compliance were compared with Student’s t-test, or Fisher’s exact test as indicated.
Measurements and main results
Out of 26 infants, 23 (88%) had injuries that had possibly been inflicted, and 3 had accidental injuries. Initial TCD evaluation demonstrated intracranial hypertension with decreased diastolic velocity, increased PI and RI, and decreased compliance. Surgical evacuation resulted in statistically significant improvement in cerebral hemodynamics (diastolic velocity: 17.2±10 cm/s vs. 31.1±10 cm/s, p<0.0015, PI: 2.5±1.3 vs. 1.4±0.8, p<0.002, RI: 0.8±0.2 vs. 0.6±0.1, p<0.005) in all but 3 infants, who eventually died. Surgical drainage (primary shunting or external drainage) was needed in 23 infants and resulted in further improvement in cerebral hemodynamics. Finally, 73% of the infants made a good recovery.
Conclusions
Children with acute bilateral HSD have a high incidence of increased intracranial pressure as assessed by TCD. Surgical evacuation improves cerebral hemodynamics. TCD could be used for assessing the need for, and the efficiency of surgical drainage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute subdural hematoma (SDH) is one of the most frequent conditions in children with head injuries under 2 years of age [1]. It can be observed in as many as 46–70% of children with inflicted injuries [2–4]. It is a devastating lesion that carries a higher risk of posttraumatic seizures, developmental deficiency, and mortality than other lesions resulting from accidental brain injuries [1, 5, 6]. The questions of intracranial hypertension, and the need for surgical management of acute SDH, remain unresolved, since there are no studies directly measuring intracranial pressure (ICP) in children with acute SDH, and no clear evidence in the literature that early surgical evacuation could improve the outcome. Surgical indications vary widely from simple needle puncture to early subduroperitoneal shunting, and remain based upon a body of clinical and imaging arguments [7, 8]. Transcranial Doppler (TCD) is a non-invasive and easily reproducible examination that has already proved its usefulness for evaluating ICP and the efficiency of surgical procedures for intracranial hypertension from hydrocephalus [9–11]. We prospectively evaluated the contribution of TCD in evaluating the incidence of intracranial hypertension, and the efficiency of surgical evacuation on cerebral hemodynamics in infants with acute SDH.
Patients and methods
Children less than 2 years of age, with subdural bilateral collection more than 1 cm thick and spontaneous hyperdensity evidenced on admission CT scan examination were prospectively included in the study. All of them had detailed physical examination and complete evaluation including cerebral CT scan, complete skeletal survey, EEG recording, and fundoscopic examination within 6 h of admission. Initial critical care management included tracheal intubation with mechanical ventilation in children with a Glasgow coma score less than 8, and systematic seizures prevention with intravenous phenytoin (15 mg/kg IV bolus followed by 15 mg/kg/day IV infusion) and phenobarbital (loading dose: IV 15 mg/kg). A TCD examination was performed, upon admission, by a trained operator, including bilateral insonation of the M1 segment of the middle cerebral artery (MCA) through the temporal window as previously described [12]. A Doppler probe operating continuously at 2 MHz (Waki 1-TC, Atys Medical, France) was used for the purpose of the study. Systolic, diastolic, and mean velocities, pulsatility index (PI = systolic velocity − diastolic velocity/mean velocity), and resistivity index (RI = systolic velocity − diastolic velocity/systolic velocity) were recorded for each side. After standard examination, a cerebral compliance test was performed. It consisted of continuous Doppler recording during gentle compression of the anterior fontanel for 10 s, and then releasing compression. Compliance was considered as normal when compression decreased diastolic velocity without modifying systolic velocity, with a return to baseline within 5 s of pressure release. Compliance was considered as decreased when fontanel compression decreased both systolic and diastolic velocities with a return to baseline within 10 s of pressure release. Compliance was considered as abolished when systolic and diastolic velocities did not return to baseline after pressure release. Each child with a potentially non-accidental injury or with an history inconsistent with the severity of the brain lesion observed benefitted from a multidisciplinary medical and social inquiry.
Early surgical evacuation of SDH was considered by neurosurgeons in children with a Glasgow coma scale score of 12 or less. Indications were based upon the clinical observation of a bulging fontanel in a child with bilateral subdural collection more than 1 cm thick on the CT scan. Surgical treatment consisted of direct needle puncture as the first step, followed by either external subdural drainage or subduroperitoneal shunt implantation as required. A head CT scan was performed before and after surgical drainage procedures, but not after needle evacuation. A TCD evaluation was systematically performed immediately before each surgical evacuation and 1 h and 6 h after operation. Postoperative systolic, diastolic, and mean velocities, PI, RI, and compliance were compared with preoperative measurements. Each patient served as his own control. Results are presented as means ± standard deviations. Statistical analysis used paired Student’s t-test for comparison of means, and Fisher’s exact test for discrete variables. A p value of less than 0.05 was considered as significant.
Results
Over a 6-month period, 26 children with acute SDH requiring surgical evacuation were evaluated. Mean age was 4.8±2 months, and 68% were boys. Among them, 3 (11.5%) were in a road traffic accident as passengers of moving vehicles; the remaining 23 children had a described mechanism of injury inconsistent with the lesions observed. A cerebral CT scan evidenced a bilateral subdural collection more than 1 cm thick, with interhemispheric and convexity blood hyperdensity in all children. Subarachnoid or parenchymal hemorrhages were associated in 20% and 12% of the patients respectively. Cerebral edema was noted in 5 patients and brain ischemia in 4. Upon admission, 13 patients had a GCS score of 8 or less and requiring mechanical ventilation, 6 had early seizures, and 5 had early refractory status epilepticus requiring continuous barbiturate therapy. Six children (23%) developed further status epilepticus despite prophylactic treatment and required continuous barbiturate therapy. Fundoscopic examination was normal in 7 patients (3 with witnessed accidental injury) and depicted bilateral retinal hemorrhage in 19. Skeletal survey evidenced associated fractures in only 2 patients.
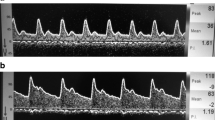
Preoperative TCD evaluation revealed decreased diastolic velocity in all but one child, with increased PI and RI (Table 1), and an abnormal cerebral compliance in 23 patients. The first surgical operation was a direct puncture through the fontanel in all cases. It resulted in immediate increased diastolic velocity (17.2±10 cm/s vs. 31.1±10 cm/s, p<0.0015) with concomitant decreased PI (2.5±1.3 vs. 1.4±0.8, p<0.002) and RI (0.8±0.2 vs. 0.6±0.1, p<0.005) in all the cases. Compliance was normalized in 11 children (42.5%), remained decreased in 11, and abolished in 4 (15%). Further surgical treatment was required based upon clinical and neuroimaging arguments in all infants. It consisted of primary subduroperitoneal shunting in 8 patients and external subdural drainage in 15 patients, with massive hemorrhage after needle puncture. Only 2 patients with external drainage did not require secondary internal shunting because of spontaneously self-limiting collection (Table 2). Definitive surgical treatment resulted in significantly increased diastolic velocity and decreased pulsatility index. Cerebral compliance was normalized in 20 patients, remained abolished despite surgical treatment in 3 patients, and decreased in 3 (Figs. 1, 2). Finally, 3 patients (11.5%) died, all of them had dramatically decreased diastolic velocity and abolished compliance at first examination, and needle evacuation and external drainage failed to restore cerebral compliance. On evaluation after 1 month, 4 patients (15.5%) had severe developmental disability and 19 (73%) had minor or no sequelae. Shunt removal was possible between 3 and 6 months after implantation in all the survivors.
Discussion
In 26 children less than 2 years of age with acute SDH, we were able to demonstrate that preoperative TCD examination evidenced severe intracranial hypertension with decreased diastolic velocity and increased resistivity and pulsatility indexes, and that surgical evacuation resulted in dramatic improvement in TCD values. Although definite arguments are lacking to ascertain that surgical evacuation was beneficial for the final outcome, variations of TCD velocities and indexes related to surgical treatment could reflect improvement in cerebral hemodynamic conditions.
Previous studies have reported that 24% of children less than 2 years of age with head injuries may have suffered from non-accidental trauma [3]. The most frequent brain lesions in these cases are subdural hematomas appearing as unilateral or bilateral high-density collections with a particular propensity for the interhemispheric fissure on cerebral CT scan [6]. Early diffuse hypodensity resulting from anoxo-ischemic encephalopathy can be found in shaking impact syndrome and reflect the severity of the injury [12]. This contrasts with accidental injuries where acute SDH are rare and almost always associated with diffuse cerebral edema and axonal injuries resulting in petechial intraparenchymal hemorrhages [2, 5]. When associated with inconsistent history of trauma, cutaneous marks or bruises, or metaphyseal fractures, acute HSD is almost pathognomonic of battered or shaken baby syndrome [13]. Retinal hemorrhage, although non-specific for inflicted injuries, is a rare finding in children with documented accidental head injury. It was not noted in the three patients in the present study who were in motor vehicle accidents. Seizures occur in 40–70% of children with acute SDH [5, 6, 13], and can result in intractable status epilepticus, despite systematic anticonvulsant therapy. Status epilepticus occurred in 11 out of our 26 patients (42%). This high incidence of seizures could reflect the severity of this kind of brain injury, which carries a high risk of mortality and poor outcome. Although there are no studies in the literature reporting the use of direct ICP measurement in these patients, the most frequently evocated cause of death is uncontrollable intracranial hypertension. Autopsy findings consistent with cortical and white-matter atrophy support the hypothesis that the combination of mechanical trauma, brain compression, hypoxia, and seizure activity overwhelms the compensatory mechanisms of the immature brain, resulting in intracranial hypertension and massive neuronal loss [13].
The means of and indications for surgical evacuation of acute SDH remain controversial. Needle aspiration through the fontanel is the simplest way to evacuate subdural blood [14]; however, it fails to solve the problem definitively in many cases [7]. Burr hole evacuation with or without external drainage implantation has been suggested [15]. In a retrospective study, Tolias et al. found that needle aspiration and burr hole evacuation had a higher incidence of infection than primary shunting and concluded that needle evacuation should be avoided in the absence of severe intracranial hypertension [7]. In a large series of infants benefitting from primary subduroperitoneal shunting, Vinchon et al. found that when subdural taps failed to control SDH, subduroperitoneal shunting was the best procedure, with a complication rate of 15% [8]. In our study, all the children had early needle evacuation, but required further treatment and final subduroperitoneal shunting was required in 21 out of 23 survivors. The thickness of the subdural collection seems to be an important argument for surgical evacuation, but to our knowledge there are no prospective randomized studies demonstrating the benefit to outcome of the surgical evacuation of large subdural collections. It seems logical to assume that a large bilateral SDH could contribute to increased intracranial ICP and brain compression. However, evaluation of increased ICP in young children relies mostly on clinical signs such as tension of the fontanel and neurological examination.
All our patients had a bulging fontanel, large bilateral hematoma, and clinical signs of increased ICP; 13 were comatose, and 11 had seizure activity. Indications for surgical drainage were independent of TCD findings and emergency needle aspiration was the first step. Initial TCD examination demonstrated decreased diastolic velocity and increased pulsatility and resistivity indexes in all but 1 child, and decreased cerebral compliance in 23. This may reflect a high incidence of severe intracranial hypertension and confirm retrospectively the need for surgical evacuation in these patients. TCD is a non-invasive, easily reproducible bedside tool that can be efficient in the diagnosis of intracranial hypertension. Insonation of the MCA through the temporal window is easy to perform and is an accurate indirect assessment of 95% of the cerebral blood flow. It is demonstrated that with increasing ICP and decreasing cerebral perfusion pressure, diastolic velocity is first affected, with preserved systolic velocity and a concomitant increase in the pulsatility and resistivity indexes [15]. TCD has been used in patients with possible intracranial hypertension of various origins to evaluate the influence of surgical treatment on cerebral hemodynamics. A pressure provocation during TCD examination in hydrocephalic infants with an opened fontanel has been previously used for determining the need for shunt implantation. Westra et al. in their study demonstrated that children with increased resistivity index and decreased compliance determined with pressure provocation benefitted more from shunting than the others [9]. These findings were corroborated by Jindal and Mahapatra, who found a positive correlation between variations of TCD and decreased ventricular size after shunt implantation [11]. In our patients, needle aspiration resulted in a significant and immediate increase in diastolic velocity and decreased pulsatility and resistivity indexes reflecting improvement in cerebral hemodynamics. Cerebral compliance remained absent in the three patients who eventually died, but improved in 42% of the cases. However, needle aspiration was not sufficient, and all infants required further surgical treatment because of persistent or growing subdural collection, and/or clinical signs of intracranial hypertension. TCD variations after surgical drainage demonstrated additional improvement in cerebral hemodynamics, with normalized diastolic velocity and indexes in all. Because of the design of the study, we could not correlate precisely the variations of TCD to the variations in size of the collection. However, we were able to demonstrate the positive impact of surgical evacuation on cerebral hemodynamics in these children with severe initial intracranial hypertension. Additionally, we could not demonstrate the precise positive impact of surgical evacuation on outcome. An interesting finding that needs further confirmation was that the children who died had evidence of severe intracranial hypertension on early TCD evaluation and did not demonstrate a dramatic improvement in cerebral hemodynamics after surgical evacuation.
Provided that these findings can be confirmed in a larger prospective study that is now in progress, we suggest that TCD could be used in the objective assessment of intracranial hypertension in infants with acute SDH. It may also be a valuable means of assessing the need for, and the efficiency, in terms of cerebral hemodynamics, of the surgical drainage of subdural collections.
References
Michaud LJ, Rivara FP, Gready S, Ready DT (1992) Predictors of survival and severity of disabilities after severe brain injury in children. Neurosurgery 31:254–264
Reece RM, Sege R (2000) Childhood head injuries: accidental or inflicted? Arch Pediatr Adolesc Med 154:11–15
Di Scala C, Sege R, Li G, Reece RM (2000) Child abuse and unintentional injuries: a 10-year retrospective. Arch Pediatr Adolesc Med 154:16–22
Dashti SR, Decker DD, Razzaq A, Cohen AR (1999) Current patterns of inflicted head injury in children. Pediatr Neurosurg 31:302–306
Ewing-Cobbs L, Kramer L, Prasad M et al (1998) Neuroimaging, physical and developmental findings after inflicted and noninflicted brain injury in young children. Pediatrics 102:300–307
Duhaime AC, Alario AJ, Lewander WJ et al (1992) Head injury in very young children: mechanisms, injury types and ophthalmologic findings in 100 hospitalized patients younger than 2 years of age. Pediatrics 90:179–185
Tolias C, Sgouros S, Walsh AR, Hockley AD (2001) Outcome of surgical treatment for subdural fluid collections in infants. Pediatr Neurosurg 34:280–284
Vinchon M, Noule N, Soto-Ares G, Dhellemmes P (2001) Subduroperitoneal drainage for subdural hematomas in infants: results in 244 cases. J Neurosurg 95:249–255
Westra SJ, Lazareff J, Curran JG, Sayre JW, Kawamoto H (1998) Transcranial Doppler ultrasonography to evaluate the need for cerebral fluid drainage in hydrocephalic children. J Ultrasound Med 17:561–569
Hanlo PW, Gooskens RHJM, Faber JAJ, Nijhuis IJM, Peters RJA, Van Huffelen AC, Tulleken CAF, Willemse J (1995) Value of transcranial Doppler indices in predicting raised ICP in infantile hydrocephalus. Childs Nerv Syst 11:595–603
Jindal A, Mahapatra AK (1998) Correlation of ventricular size and transcranial Doppler findings before and after ventricular peritoneal shunt in patients with hydrocephalus: prospective study of 35 patients. J Neurol Neurosurg Psychiatry 65:269–271
Byrd SE, Seibert JJ (1999) Transcranial Doppler imaging in pediatric abnormalities. Neuroimaging Clin N Am 9:17–40
Duhaime AC, Christian CW, Rorke LB, Zimmerman R (1998) Current concepts: nonaccidental head injury in infants—the shaken baby syndrome. N Engl J Med 338:1822–1829
MacDonald RL, Hoffman HJ, Kestle JR, Rutka JT, Weinstein G (1994) Needle aspiration of acute subdural hematomas in infancy. Pediatr Neurosurg 20:73–76
Gaskill SJ, Oakes WJ, Marlin AE (1991) Continuous external drainage in the treatment of subdural hematomas in infancy. Pediatr Neurosurg 92:121–123
Czonyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD (1998) Cerebral perfusion pressure in head injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg 88:802–808
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meyer, P.G., Ducrocq, S., Rackelbom, T. et al. Surgical evacuation of acute subdural hematoma improves cerebral hemodynamics in children: a transcranial Doppler evaluation. Childs Nerv Syst 21, 133–137 (2005). https://doi.org/10.1007/s00381-004-1016-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-004-1016-1