Abstract
Non-invasive measurement of ICP (nICP) can be warranted in patients at risk for developing increased ICP during pneumoperitoneum (PP). Our aim was to assess available data on the application of nICP monitoring during these procedures and to present a patient assessed with an innovative combination of noninvasive tools. Literature review of nICP assessment during PP did not find any studies comparing different methods intraprocedurally and only few studies of any nICP monitoring were available: transcranial Doppler (TCD) studies used the pulsatility index (PI) as an estimator of ICP and failed to detect a significant ICP increase during PP, whereas two out of three optic nerve sheath diameter (ONSD) studies detected a statistically significant ICP increase. In the case study, we describe a 52 year old man with a high grade thalamic glioma who underwent urgent laparoscopic cholecystectomy. Considering the high intraoperative risk of developing intracranial hypertension, he was monitored through parallel ONSD ultrasound measurement and TCD derived formulae (flow velocity diastolic formula, FVdnICP, and PI). ONSD and FVdnICP methods indicated a significant ICP increase during PP, whereas PI was not significantly increased. Our experience, combined with the literature review, seems to suggest that PI might not detect ICP changes in this context, however we indicate a possible interest of nICP monitoring during PP by means of ONSD and of TCD derived FVdNICP, especially for patients at risk for increased ICP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The laparoscopic approach has become a common technique for many types of surgical procedures, including gynecology, general surgery, and urology.
During gas insufflation [pneumoperitoneum (PP)], increased intra-abdominal pressure (IAP) can cause decreased venous return, cardiac output and preload, and increased heart rate, mean arterial pressure, and systemic vascular resistance [1, 2]. Moreover, carbon dioxide (CO2) gas insufflation can cause hypercapnia and respiratory acidosis due to absorption of the gas across the peritoneal surface [2]. The effects on the respiratory and cardiovascular system are usually mild and well tolerated [3]; less documented are the effects on intracranial pressure (ICP).
However, in the last years, there is growing evidence that demonstrates a positive correlation between IAP and ICP in animal models [7] and in humans [8]. Moreover, some authors have documented severe neurological complications during laparoscopy [4–6]. These studies have attributed neurological deficits to cerebral ischemia and cerebral edema, related to increased ICP. In general, the effect of IAP on ICP cannot be easily determined intraoperatively, but some authors [3] have shown that during laparoscopic surgery the insufflation of the abdomen with CO2 can significantly increase ICP [8]. Neurosurgeons and anesthesiologists are reluctant in these situations to apply invasive techniques for ICP monitoring, such as intraventricular catheters or microtransducer devices, because of the possible complications, such as malpositioning, infection or haemorrage [1, 9] and, further, the current literature does not provide any indications for invasive ICP monitoring.
There is only a small study on nine patients where ICP was invasively measured during laparoscopic ventriculo-peritoneal shunt placement. Although no neurological complication was reported, the authors demonstrated that laparoscopy linearly increases ICP up to 25 mmHg [10].
Therefore, in particular for patients at risk of developing intracranial hypertension who undergo laparoscopic surgery, a non-invasive method to monitor ICP would be desirable.
We here report a clinical case of a 52 year-old man affected by a right sided high-grade thalamic glioma, who underwent an urgent laparoscopic cholecystectomy. Considering the high risk of developing intracranial hypertension during surgery, the patient was monitored intraoperatively through simultaneous optic nerve sheath diameter (ONSD) ultrasound measurements and transcranial Doppler (TCD).
2 Methods
2.1 Case report
Written informed consent was obtained from the patient before the procedure regarding anesthetic management, monitoring and data publishing.
TCD examination was performed by two expert operators (RC and DC) by the use of a 2 MHz probe of a TCD system (Doppler Box DWL Compumedics, Germany) which was used to insonate the middle cerebral artery via the trans-temporal approach. We recorded systolic and diastolic blood flow velocities. Pulsatility index (PI) was calculated according to the method of Gosling (PI = sFV − dFV/mFV), where sFV is the systolic flow velocity, dFV is the diastolic flow velocity divided by the mean flow velocity [11].
Non-invasive measurement of ICP (nICP) was calculated according to FVdnICP formula (nCPP = MAP × FVd/FVm + 14), where nCPP is the non invasive Cerebral Perfusion Pressure (nCPP) and MAP is the mean arterial blood pressure [12]. nICP was then estimated as the difference between MAP and nCPP (nICP = MAP − nCPP).
Ultrasound examination of the eyes was performed by two trained investigators (CR and DC) and according to previously described protocols [13–16].
The patient was placed in a supine position. A thick layer of gel was applied over the closed upper eyelid. The 7.5-MHz linear probe (Toshiba’s Xario™ 200, PLT-704SBT Transducer) was placed only on the gel in the temporal area of the eyelid, not on the eyelid itself, to prevent pressure being exerted on the eye. The placement of the probe was adjusted to give a suitable angle for displaying the entry of the optic nerve into the globe [17].
The two-dimensional mode was used, and ONSD was measured 3 mm behind the globe using an electronic caliper and an axis perpendicular to the optic nerve (Fig. 2). For each optic nerve two measurements were made, one in the sagittal plane and the other in the transverse plane by rotating the probe clockwise.
2.2 Literature review
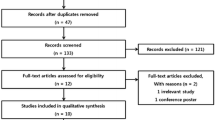
For the review of the literature, a comprehensive PubMed/MEDLINE search was performed for the period from 1st January 1990 to 1st January 2015 using as search strategy a combination of the key-words ‘videolaparoscopy’, ‘pneumoperitoneum’, intra-abdominal pressure’, and ‘ICP’, properly combined with Boolean operators and using Medical Subject-Headings (MeSH) terms where adequate. The used search string was: ((“pneumoperitoneum”[MeSH Terms] OR “pneumoperitoneum”[All Fields]) OR ((“videotape recording”[MeSH Terms] OR (“videotape”[All Fields] AND “recording”[All Fields]) OR “videotape recording”[All Fields] OR “video”[All Fields]) AND (“laparoscopy”[MeSH Terms] OR “laparoscopy”[All Fields])) OR (intra-abdominal[All Fields] AND (“pressure”[MeSH Terms] OR “pressure”[All Fields]))) AND (“intracranial pressure”[MeSH Terms] OR (“intracranial”[All Fields] AND “pressure”[All Fields]) OR “intracranial pressure”[All Fields]). A total of 111 results were obtained. Results were further screened, retaining only full length articles written in English, focusing on non invasive techniques for intraoperatively measuring and monitoring ICP, such as nICP, ONSD and TCD. Articles using animal models were excluded. Review articles were scanned for catching further potentially relevant manuscripts. Finally, fourteen published case reports and case series on intraoperative ICP monitoring on nICP as well as TCD and ONSD were considered relevant and selected for review and summarized in Tables 2 and 3, respectively. In particular, we found a total of four papers dealing with ONSD measurement during PP (one of these in pediatric patients). For TCD, we found two case reports (adult patients), six case studies for adult patients and two studies in pediatric patients.
2.3 Data collection
For each of these studies we collected data about general characteristics of the reported subjects or groups (age, gender, weight, height), type of procedure, duration of procedure and of PP, presence or absence of Trendelenburg positioning, anesthesiological and surgical parameters and characteristics: American Society of Anesthesia (ASA scale, end tidal CO2 intra-abdominal pressure, type of anaesthesia, fluids administration, influence of PP on mean arterial pressure (MAP)), on PaCO2 and on ONSD and TCD measures (mFV and PI).
2.4 Statistical analysis
Quantitative parameters were presented as mean, and standard deviation, median, whereas qualitative parameters as numbers.
3 Results
3.1 Case report
A 52 year-old man arrived by ambulance to the emergency ward due to persistent fever, intractable abdominal pain, nausea and vomiting. The initial examination evidenced tachycardia (pulse rate 130/min), fever (38.2 °C) and hypotension (97/56 mmHg). Palpation of the abdomen showed guarding and rebound tenderness, primarily in the right upper quadrant.
One year before the patient had been diagnosed of a multiform thalamic glioblastoma (Glioblastoma Multiforme, GBM) (Fig. 1). At that stage, a biopsy had confirmed the high-grade stage of the tumor, and the patient, due to the site of the lesion, was not considered suitable for any surgical procedure and was treated with palliative chemotherapy and radiotherapy. Eight months later, he had been admitted to the hospital with confusion and progressive neurological deterioration. A brain Magnetic Resonance Imaging (MRI) study showed tumor progression associated with perilesional edema, increased mass effect without signs of cerebral herniation (Fig. 1). Again, no surgical procedures were performed at that time and the patient was discharged to home, under medical treatment (Dexamethasone 2.5 mg, Citalopram 20 mg) with a Glasgow Coma Scale (GCS) of 14 (Eyes 4, Motor 6, Voice 4).
On admission at our hospital, the patient presented with an unchanged GCS of 14, with equal pupils and bilaterally preserved reflexes, normal power at the four limbs and negative Babinski sign. There was no record of excessive alcohol or other drug abuse. A blood test showed a high white blood cell count (17.6 × 109/L), hemoglobin of 148 g/L, hematocrit 42 %, and a very high C-reactive protein concentration (54 mg/L).
A chest X-ray showed clear lungs. Focused assessment with sonography (FAST) revealed a dilated common bile duct with signs of inflammation. Abdominal computed tomography (CT) confirmed a diagnosis of cholangitis and sepsis. Therefore, the patient was put forward for urgent laparoscopic cholecystectomy (Fig. 2).
Considering the emergency conditions of the procedure, brain imaging was not repeated before surgery.
Considering the high risk of developing intracranial hypertension during surgery, the patient was monitored intraoperatively through simultaneous ONSD ultrasound measurement and TCD.
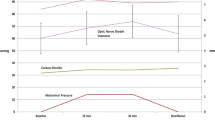
Intraoperative management After standard monitoring examinations as per our hospital protocols (pulse oxymetry, non-invasive blood pressure measurement, electrocardiography), anesthesia was induced with propofol 2 mg/kg and fentanyl (0.1 μg). After a successful tracheal intubation, the patient was mechanically ventilated with an oxygen/air mixture (FiO2: 0.5) and proper adjustments to maintain End Tidal CO2 (ETCO2) between 32 and 35 mmHg and to avoid hypercarbia. Anesthesia was maintained with a continuous infusion of propofol (Target Controlled Infusion mode, plasmatic concentration 2 μg/mL) and remifentanil (0.10–0.25 μg/kg/min). Cisatracurium (12 mg followed by repeated bolus doses of 2 mg) was used for intraoperative neuromuscular blockade. The patient was placed in supine position. TCD examination and ONSD measurements were performed preoperatively (baseline, T0), after insufflation of PP (T1) and after some minutes intraoperatively (T2) and after PP (T3). The results are shown in Table 1. IAP was kept between 10 and 14 mmHg during the procedure. The total duration of anesthesia was of 90 min. The total duration of PP was of 40 min.
During PP, PI and FVdICP increased compared to the baseline measurement, reaching a maximum value of 1.12 and 27 mmHg, respectively.
ONSD diameter increased as well, with a highest value of 7 mmHg after PP induction. During variations in blood flow velocities and ONSD, there were no associated variations in arterial pressure, airway pressure, SPO2 and ETCO2.
At the end of the surgical procedure, the patient smoothly emerged from anesthesia. He was extubated in the operating theater with no complications. His GCS was 12 after surgery (E3, V3, M6), he remained confused for about 1 h and he was treated for headache with paracetamol. No focal neurological deficits were observed. The patient’s recovery was uneventful and he was discharged to home on the following day.
3.2 Literature review
Patient and/or cohort characteristics are shown in Tables 1 and 2. For intraoperative ONSD assessment in PP surgeries, three adult studies and one study in pediatric patients were found. For TCD studies in PP context, besides two case reports, there were six studies in the adult and two in pediatric patients. The two case reports are already presented in Table 2. Case series on nICP either through ONSD or TCD during PP had the following characteristics: number of patients varied between 10 and 36. Studies are divided into pediatric and adult series and mean age varied in adult groups between 37.6 and 64.9 years. ASA score ranged between 1 and 2 in all the studies, but two with older patients (prostatectomies) also included ASA 3 scores. PP procedures included robotic assisted laparoscopic radical prostatectomy (RALRP), urological and gynecological procedures, anterior L5–S1 interbody fusion, video-laparo-cholecystectomies, herniorraphy, not specified laparoscopies, with obvious gender distributions. Mean duration of surgery, mentioned only in few studies, ranged from 68 min (videolaparocholecystectomy) to 373 min (RALRP), and mean PP duration lasted between 31 and 240 min. PP IAP varied between 10 and 12 mmHg and ventilation was adjusted to obtain end-tidal CO2 values that ranged from 30 to 40 mmHg. Trendelenburg position was used in almost all studies (9/11). A mixed anesthesia was used in all the studies using a mixture of opioid infusion (remifentanil, sulfentanil or fentanyl) and halogenate gases (isoflurane, sevoflurane and desflurane) with the addition of N2O in three studies. PP-related MAP increase was significant in five studies, whereas MAP decrease was observed in two studies and finally no statistically significant MAP changes were detected in three studies and one study did not mention MAP changes in relation to PP. Arterial partial CO2 pressure increased significantly in all studies, where information was available. According to these authors, OSND significantly increased during PP and Trendelenburg in 75 % of the studies. An increase in FVm was found in five out of eight studies. PI never significantly changed. Only two case reports were found, describing two patients with intracranial pathology (shunted hydrocephalus). In both cases, the authors did not observe any increase in PI nor in FVm during surgery [18], except when the abdominal pressure reached 30 mmHg or during instrument insertion [19].
4 Discussion
Laparoscopy has become the preferred method for surgical treatment of most intra-abdominal pathologies, because it is minimally invasive and because it reduces risks of secondary peritoneal adhesions. Intra-abdominal CO2 insufflation, however, is associated with an increase of ICP [20–22]. PP can cause compression of vena cava with a consequent increase and obstruction of cerebral venous outflow [20, 21]. Nausea, headache and other clinical symptoms that could be associated with increased ICP have been reported after laparoscopy [23].
Hypercarbia, as a consequence of CO2 absorption, is also a risk within laparoscopic procedures, especially in patients with intracranial diseases, as it causes dilatation of intracranial arteries and thus increases ICP [20, 24].
During laparoscopy sustained increases in ICP of more than 12 mmHg above the baseline in patients with ventriculo-peritoneal shunts have been reported [20].
Animal models showed that ICP increases significantly above 15 mmHg of IAP, reaching 150 % over control values with IAP above 16 mm Hg during Trendelenburg [21].
This preliminary evidence indicated that in patients at risk of developing an increased ICP as a result of head injury or of space occupying lesions, peritoneal insufflation could induce abrupt intracranial hypertension and should probably be used with special caution and close monitoring [25].
Invasive methods are still the gold standard in the measurement of ICP, but they are associated with major complications [1, 9, 26–28].
Several techniques have been proposed for the nICP [29–31]. Among these we selected PI and FVdICP obtained by TCD and the ONSD ultrasound.
TCD is a non-invasive method for the measurement of middle cerebral artery (MCA) blood flow velocity commonly used in standard care of neurocritical care patients. PI has been the most commonly used formula [32–37], but many studies have demonstrated that this measure cannot estimate ICP values with reliable precision [36–38].
Schmitd et al. [12] proposed a new method for estimation of CPP based on FVd and demonstrated that the absolute difference between real CPP and nCPP calculated with this new method was very small.
Effects of PP on TCD derived PI have been studied in adults and children (see Table 2) with discordant results as concerns the interaction between flow velocities (FV) and PP, some considering also the possible role of Trendelenburg position.
The two reports with TCD assessment during PP [18, 19] which were about two patients with intracranial disease, concluded that TCD, being a safe technique that can detect minimal variations of cerebral hemodynamics, could be a valid monitoring option for patients undergoing laparoscopic procedures with preexisting intracranial pathology.
Several studies on adults [24, 39–43] and children [44, 45] included a wider number of patients [24, 40] undergoing different laparoscopic procedures requiring [39–41, 43] or not [24, 39] Trendelenburg position and monitored with TCD. Among these studies TCD measurement methods, IAP parameters, ventilator settings (including ETCO2), patients number, characteristics and anesthesiological management are comparable. A mixed anesthesia with sevoflurane or isoflurane was used in all cases in a window of 0.5–1.5 mean alveolar concentration (MAC) [46] and it is well known that at these levels both isoflurane and sevoflurane do not induce any significant dose-related changes in blood flow velocities [47] nor changes in cerebral blood flow autoregulation [48].
Despite this, results concerning effects of PP on FV and PI are discordant: PCO2 tends always to increase after PP, but not all authors were able to observe a concomitant increase of FV [39, 40].
PI does not seem to be significantly influenced by PP and head down position in most of the described papers. Surprisingly, one study on a paediatric cohort, registered a decrease of PI during PP [44].
Thus the available literature seems not to clarify whether PI derived from TCD could be a reliable measure to monitor ICP patients during laparoscopy.
In our case report, PI reached a maximum value of 1.12 after PP induction, which was not associated with a significant ICP increase [32–37]. To our knowledge, FVdICP formula has never been used to assess nICP intraoperatively. In our case report, nICP obtained with this new method indicated an ICP of 26 mmHg during PP (with preoperative ICP values of 16 mmHg), which recovered after PP desufflation.
ONSD measures have shown to be well correlated to ICP [49, 50].
The optic nerve sheath is in continuity with the meninges of the central nervous system. During intracranial hypertension compensatory mechanisms such as intra-cerebral blood and cerebrospinal fluid (CSF) shifts occur. As CSF is incompressible, ICP is directly transmitted to the fluid in the optic nerve sheath, increasing its diameter. According to human studies, this phenomenon occurs within minutes of acute changes in ICP [14, 17, 51]. Cutoff values of 5.7 or 5.8 mm are used to predict elevated ICP (≥20 mmHg) [50, 52, 53]. ONSD is a safe, reproducible technique, and has a fast learning curve: novice sonologists need only 25 scans to obtain adequate results [49]. ONSD behavior during PP has been investigated only in three recent studies on adults [54–56], and one in children [46], where patients without intracranial pathologies underwent laparoscopy with prolonged PP and Trendelenburg positioning.
Despite similar general patient type, intra-procedural conditions (included type of anesthesia) among these ONSD studies, which are also well comparable to those in the TCD studies in adults, the conclusions were quite different: three out of four OSND studies [46, 55, 56] detected increased ICP (reaching values above 20 mmHg) during PP and in particular Trendelenburg; whereas in TCD studies PI did not detect significant ICP changes in similar conditions.
Moreover, we observed that in all the studies the PCO2 levels did not exceed the cut-off value for impaired autoregulation [57].
All the described studies involved patients not affected by intracranial pathology and show contrasting results, even though in those cases where an increased ICP was detected, no neurological sequels were observed. The currently available literature lacks contingency analyses which are necessary to be considered in future studies.
All in all, the present review indicates that ONSD might be sensitive to IAP variations, whereas TCD derived PI is not, though comparative studies are missing. In our case report, the patient was affected by a GBM with mass effect. In this patient, mean ONSD before PP was 5.5 mm, that is close to the threshold considered at risk of increased ICP (5.7–5.8 mm). After CO2 insufflation for PP, mean ONSD significantly increased up to 6.8 mm, that is associated to an ICP above 20 mmHg, which recovered to baseline diameter after PP desufflation. This can be explained by the fact that in the presence of space occupying lesions the compensation mechanisms that normally may attenuate intracranial effects induced by PP [58] are exhausted, as previously described [4].
On TCD measurements, PI values were always stable (in the range 0.91–1.1), whereas FVdICP measures reached a value of 26 mmHg of ICP after PP insufflation, decreasing at the end of the procedure (Table 3).
To our knowledge, a combination of ONSD measurements and TCD has never been applied intraoperatively. Moreover, FVdICP formula has never been used as intraoperative monitoring. The present case shows that nICP measured through FVd formula and ONSD provides concordant information. Many authors demonstrated that FVd formula and ONSD have a strong correlation with ICP invasively measured [12–18].
This can increase the likelihood that our intraoperative measures were reliable, even though not compared with an invasive gold standard. Moreover, the utility of PI is controversial [37].
In our reported case, nICP values were not followed by anaesthesiological countermeasures for two reasons: first of all, values peaked immediately after PP induction (T1) and tended to decrease after 30 min (T2); second, at this point the surgical procedure was successfully concluded and after PP desufflation (T3), ONSD and FVdICP values were perfectly normalized. The availability of nICP measure could allow to timely apply intraoperatively anaesthesiological measures in order to control ICP such as slight hyperventilation or osmotic therapy or even to suggest a switch to open surgery if ICP levels are persistently elevated. Certainly, a continuous form of intraoperative monitoring would even be preferable, since in TCD the isolated measurement is less reliable than the observation of trends and average values [32–34].
However, our findings should be interpreted with caution. The quality of published studies, the small samples investigated, some missing/not reported data, as well as their heterogeneity and occasional/anecdotal nature, hinder us to make general inferences. Therefore, larger randomized controlled trials are required to obtain sensitivity and specificity measures, and to avoid false reporting. Once that better contingency and outcome data become available, the possible routinary use of these non invasive ICP assessment methods might be considered on the basis of the collected scientific evidences.
5 Conclusions
Noninvasive ICP monitoring could be useful in situations at risk of intracranial hypertension, such as PP, especially where invasive ICP monitoring is not indicated or available.
TCD derived formulae, in particular FVd, and ONSD ultrasound are non-invasive, safe techniques, which correlate with ICP and may provide some useful information in patients with preexisting intracranial diseases undergoing laparoscopic procedures. Further, observational/contingency based trials and controlled studies aimed at comparing these methods with the invasive gold standard are necessary to validate this theory and are also necessary to appropriately interpret clinically related information.
Abbreviations
- CO2 :
-
Carbon dioxide
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- CVP:
-
central venous pressure
- dFV:
-
Diastolic flow velocity
- ETCO2 :
-
End tidal CO2
- FVdnICP:
-
Non invasive ICP estimated by diastolic flow velocity formula
- GBM:
-
multiform thalamic glioblastoma
- GCS:
-
Glasgow Coma Scale
- IAP:
-
Intraabdominal pressure
- ICP:
-
Intracranial pressure
- MAC:
-
Mean alveolar concentration
- MAP:
-
Mean arterial blood pressure
- mFV:
-
Mean flow velocity
- MRI:
-
Magnetic resonance imaging
- nCPP:
-
Non invasive CPP
- nICP:
-
Non invasive intracranial pressure
- ONSD:
-
Optic nerve sheet diameter
- PaCO2 :
-
Partial pressure CO2
- PI:
-
Pulsatility index
- PP:
-
Pneumoperitoneum
- RALRP:
-
Robotic assisted laparoscopic radical prostatectomy
- sFV:
-
Systolic flow velocity
- TCD:
-
Transcranial Doppler
- VPS:
-
Venticuloperitoneal shunt
References
Anderson RC, Kan P, Klimo P, Brockmeyer DL, Walker ML, Kestle JR. Complications of intracranial pressure monitoring in children with head trauma. J Neurosurg. 2004;101(1 Suppl):53–8. doi:10.3171/ped.2004.101.2.0053.
Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, Fuchs KH, Jacobi C, Jansen FW, Koivusalo AM, Lacy A, McMahon MJ, Millat B, Schwenk W. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16(7):1121–43. doi:10.1007/s00464-001-9166-7.
Kalmar AF, Foubert L, Hendrickx JF, Mottrie A, Absalom A, Mortier EP, Struys MM. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br J Anaesth. 2010;104(4):433–9. doi:10.1093/bja/aeq018.
Pandey R, Garg R, Darlong V, Punj J, Chandralekha Kumar A. Unpredicted neurological complications after robotic laparoscopic radical cystectomy and ileal conduit formation in steep trendelenburg position: two case reports. Acta Anaesthesiol Belg. 2010;61(3):163–6.
Danic MJ, Chow M, Alexander G, Bhandari A, Menon M, Brown M. Anesthesia considerations for robotic-assisted laparoscopic prostatectomy: a review of 1,500 cases. J Robot Surg. 2007;1(2):119–23. doi:10.1007/s11701-007-0024-z.
Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M, Guazzoni G, Guillonneau B, Menon M, Montorsi F, Patel V, Rassweiler J, Van Poppel H. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol. 2009;55(5):1037–63. doi:10.1016/j.eururo.2009.01.036.
Bloomfield GL, Ridings PC, Blocher CR, Marmarou A, Sugerman HJ. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. Crit Care Med. 1997;25(3):496–503.
Citerio G, Vascotto E, Villa F, Celotti S, Pesenti A. Induced abdominal compartment syndrome increases intracranial pressure in neurotrauma patients: a prospective study. Crit Care Med. 2001;29(7):1466–71.
Binz DD, Toussaint LG 3rd, Friedman JA. Hemorrhagic complications of ventriculostomy placement: a meta-analysis. Neurocrit Care. 2009;10(2):253–6. doi:10.1007/s12028-009-9193-0.
Kamine TH, Papavassiliou E, Schneider BE. Effect of abdominal insufflation for laparoscopy on intracranial pressure. JAMA Surg. 2014;149(4):380–2. doi:10.1001/jamasurg.2013.3024.
Gosling RG, King DH. Arterial assessment by Doppler-shift ultrasound. Proc R Soc Med. 1974;67(6 Pt 1):447–9.
Schmidt EA, Czosnyka M, Gooskens I, Piechnik SK, Matta BF, Whitfield PC, Pickard JD. Preliminary experience of the estimation of cerebral perfusion pressure using transcranial Doppler ultrasonography. J Neurol Neurosurg Psychiatry. 2001;70(2):198–204.
Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10(4):376–81.
Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatr Radiol. 1996;26(10):701–5.
Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol. 1996;26(10):706–10.
Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9(8):791–9.
Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87(1):34–40. doi:10.3171/jns.1997.87.1.0034.
Staikou C, Tsaroucha A, Mani A, Fassoulaki A. Transcranial Doppler monitoring of middle cerebral flow velocity in a patient with a ventriculoperitoneal shunt undergoing laparoscopy. J Clin Monit Comput. 2012;26(6):487–9. doi:10.1007/s10877-012-9380-y.
Ravaoherisoa J, Meyer P, Afriat R, Meyer Y, Sauvanet E, Tricot A, Carli P. Laparoscopic surgery in a patient with ventriculoperitoneal shunt: monitoring of shunt function with transcranial Doppler. Br J Anaesth. 2004;92(3):434–7. doi:10.1093/bja/aeh067.
Uzzo RG, Bilsky M, Mininberg DT, Poppas DP. Laparoscopic surgery in children with ventriculoperitoneal shunts: effect of pneumoperitoneum on intracranial pressure—preliminary experience. Urology. 1997;49(5):753–7. doi:10.1016/S0090-4295(97)00233-1.
Rosenthal RJ, Hiatt JR, Phillips EH, Hewitt W, Demetriou AA, Grode M. Intracranial pressure. Effects of pneumoperitoneum in a large-animal model. Surg Endosc. 1997;11(4):376–80.
Rosin D, Brasesco O, Varela J, Saber AA, You S, Rosenthal RJ, Cohn SM. Low-pressure laparoscopy may ameliorate intracranial hypertension and renal hypoperfusion. J Laparoendosc Adv Surg Tech A. 2002;12(1):15–9. doi:10.1089/109264202753486876.
Cooke SJ, Paterson-Brown S. Association between laparoscopic abdominal surgery and postoperative symptoms of raised intracranial pressure. Surg Endosc. 2001;15(7):723–5.
Fujii Y, Tanaka H, Tsuruoka S, Toyooka H, Amaha K. Middle cerebral arterial blood flow velocity increases during laparoscopic cholecystectomy. Anesth Analg. 1994;78(1):80–3.
Mobbs RJ, Yang MO. The dangers of diagnostic laparoscopy in the head injured patient. J Clin Neurosci. 2002;9(5):592–3.
Holloway KL, Barnes T, Choi S, Bullock R, Marshall LF, Eisenberg HM, Jane JA, Ward JD, Young HF, Marmarou A. Ventriculostomy infections: the effect of monitoring duration and catheter exchange in 584 patients. J Neurosurg. 1996;85(3):419–24. doi:10.3171/jns.1996.85.3.0419.
Hoefnagel D, Dammers R, Ter Laak-Poort MP, Avezaat CJ. Risk factors for infections related to external ventricular drainage. Acta Neurochir (Wien). 2008;150(3):209–14. doi:10.1007/s00701-007-1458-9 (discussion 214).
Bauer DF, Razdan SN, Bartolucci AA, Markert JM. Meta-analysis of hemorrhagic complications from ventriculostomy placement by neurosurgeons. Neurosurgery. 2011;69(2):255–60. doi:10.1227/NEU.0b013e31821a45ba.
Kirk T, Jones K, Miller S, Corbett J. Measurement of intraocular and intracranial pressure: is there a relationship? Ann Neurol. 2011;70(2):323–6. doi:10.1002/ana.22414.
Shimbles S, Dodd C, Banister K, Mendelow AD, Chambers IR. Clinical comparison of tympanic membrane displacement with invasive ICP measurements. Acta Neurochir Suppl. 2005;95:197–9.
Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2011;37(7):1059–68. doi:10.1007/s00134-011-2224-2.
Nadvi SS, Du Trevou MD, Van Dellen JR, Gouws E. The use of transcranial Doppler ultrasonography as a method of assessing intracranial pressure in hydrocephalic children. Br J Neurosurg. 1994;8(5):573–7.
Brandi G, Bechir M, Sailer S, Haberthur C, Stocker R, Stover JF. Transcranial color-coded duplex sonography allows to assess cerebral perfusion pressure noninvasively following severe traumatic brain injury. Acta Neurochir (Wien). 2010;152(6):965–72. doi:10.1007/s00701-010-0643-4.
Bellner J, Romner B, Reinstrup P, Kristiansson KA, Ryding E, Brandt L. Transcranial Doppler sonography pulsatility index (PI) reflects intracranial pressure (ICP). Surg Neurol. 2004;62(1):45–51. doi:10.1016/j.surneu.2003.12.007 (discussion 51).
Melo JR, Di Rocco F, Blanot S, Cuttaree H, Sainte-Rose C, Oliveira-Filho J, Zerah M, Meyer PG. Transcranial Doppler can predict intracranial hypertension in children with severe traumatic brain injuries. Childs Nerv Syst. 2011;27(6):979–84. doi:10.1007/s00381-010-1367-8.
de Riva N, Budohoski KP, Smielewski P, Kasprowicz M, Zweifel C, Steiner LA, Reinhard M, Fabregas N, Pickard JD, Czosnyka M. Transcranial Doppler pulsatility index: what it is and what it isn’t. Neurocrit Care. 2012;17(1):58–66. doi:10.1007/s12028-012-9672-6.
Zweifel C, Czosnyka M, Carrera E, de Riva N, Pickard JD, Smielewski P. Reliability of the blood flow velocity pulsatility index for assessment of intracranial and cerebral perfusion pressures in head-injured patients. Neurosurgery. 2012;71(4):853–61. doi:10.1227/NEU.0b013e3182675b42.
Czosnyka M, Richards HK, Whitehouse HE, Pickard JD. Relationship between transcranial Doppler-determined pulsatility index and cerebrovascular resistance: an experimental study. J Neurosurg. 1996;84(1):79–84. doi:10.3171/jns.1996.84.1.0079.
Colomina MJ, Godet C, Pellise F, Bago J, Villanueva C. Transcranial Doppler monitoring during laparoscopic anterior lumbar interbody fusion. Anesth Analg. 2003;97(6):1675–9.
Kalmar AF, Dewaele F, Foubert L, Hendrickx JF, Heeremans EH, Struys MM, Absalom A. Cerebral haemodynamic physiology during steep Trendelenburg position and CO2 pneumoperitoneum. Br J Anaesth. 2012;108(3):478–84. doi:10.1093/bja/aer448.
Abe K, Hashimoto N, Taniguchi A, Yoshiya I. Middle cerebral artery blood flow velocity during laparoscopic surgery in head-down position. Surg Laparosc Endosc. 1998;8(1):1–4.
De Cosmo G, Iannace E, Primieri P, Valente MR, Proietti R, Matteis M, Silvestrini M. Changes in cerebral hemodynamics during laparoscopic cholecystectomy. Neurol Res. 1999;21(7):658–60.
Kirkinen P, Hirvonen E, Kauko M, Purhonen S, Nuutinen L. Intracranial blood flow during laparoscopic hysterectomy. Acta Obstet Gynecol Scand. 1995;74(1):71–4.
Huettemann E, Terborg C, Sakka SG, Petrat G, Schier F, Reinhart K. Preserved CO2 reactivity and increase in middle cerebral arterial blood flow velocity during laparoscopic surgery in children. Anesth Analg. 2002;94(2):255–8 (table of contents).
Karsli C, El-Hout Y, Lorenzo AJ, Langer JC, Bagli DJ, Pippi Salle JL, Bissonette B, Farhat WA. Physiological changes in transperitoneal versus retroperitoneal laparoscopy in children: a prospective analysis. J Urol. 2011;186(4 Suppl):1649–52. doi:10.1016/j.juro.2011.03.069.
Min JY, Lee JR, Oh JT, Kim MS, Jun EK, An J. Ultrasonographic assessment of optic nerve sheath diameter during pediatric laparoscopy. Ultrasound Med Biol. 2015;. doi:10.1016/j.ultrasmedbio.2015.01.009.
Kuroda Y, Murakami M, Tsuruta J, Murakawa T, Sakabe T. Blood flow velocity of middle cerebral artery during prolonged anesthesia with halothane, isoflurane, and sevoflurane in humans. Anesthesiology. 1997;87(3):527–32.
Gupta S, Heath K, Matta BF. Effect of incremental doses of sevoflurane on cerebral pressure autoregulation in humans. Br J Anaesth. 1997;79(4):469–72.
Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49(4):508–14. doi:10.1016/j.annemergmed.2006.06.040.
Geeraerts T, Launey Y, Martin L, Pottecher J, Vigue B, Duranteau J, Benhamou D. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33(10):1704–11. doi:10.1007/s00134-007-0797-6.
Launey Y, Nesseler N, Le Maguet P, Malledant Y, Seguin P. Effect of osmotherapy on optic nerve sheath diameter in patients with increased intracranial pressure. J Neurotrauma. 2014;31(10):984–8. doi:10.1089/neu.2012.2829.
Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008;15(2):201–4. doi:10.1111/j.1553-2712.2007.00031.x.
Moretti R, Pizzi B. Ultrasonography of the optic nerve in neurocritically ill patients. Acta Anaesthesiol Scand. 2011;55(6):644–52. doi:10.1111/j.1399-6576.2011.02432.x.
Verdonck P, Kalmar AF, Suy K, Geeraerts T, Vercauteren M, Mottrie A, De Wolf AM, Hendrickx JF. Optic nerve sheath diameter remains constant during robot assisted laparoscopic radical prostatectomy. PLoS ONE. 2014;9(11):e111916. doi:10.1371/journal.pone.0111916.
Whiteley JR, Taylor J, Henry M, Epperson TI, Hand WR. Detection of elevated intracranial pressure in robot-assisted laparoscopic radical prostatectomy using ultrasonography of optic nerve sheath diameter. J Neurosurg Anesthesiol. 2015;27(2):155–9. doi:10.1097/ANA.0000000000000106.
Kim MS, Bai SJ, Lee JR, Choi YD, Kim YJ, Choi SH. Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep trendelenburg positioning proven by ultrasonographic measurement of optic nerve sheath diameter. J Endourol. 2014;28(7):801–6. doi:10.1089/end.2014.0019.
McCulloch TJ, Visco E, Lam AM. Graded hypercapnia and cerebral autoregulation during sevoflurane or propofol anesthesia. Anesthesiology. 2000;93(5):1205–9.
Eklund A, Smielewski P, Chambers I, Alperin N, Malm J, Czosnyka M, Marmarou A. Assessment of cerebrospinal fluid outflow resistance. Med Biol Eng Comput. 2007;45(8):719–35. doi:10.1007/s11517-007-0199-5.
Acknowledgments
D.C. and M.C. are partially supported by NIHR Brain Injury Healthcare Technology Co-operative, Cambridge, UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
S. Bacigaluppi and D. Cardim have equally contributed.
Rights and permissions
About this article
Cite this article
Robba, C., Bacigaluppi, S., Cardim, D. et al. Intraoperative non invasive intracranial pressure monitoring during pneumoperitoneum: a case report and a review of the published cases and case report series. J Clin Monit Comput 30, 527–538 (2016). https://doi.org/10.1007/s10877-015-9765-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9765-9