Abstract
Object
The authors analyze the factors that predispose to persistent hydrocephalus in children with posterior fossa tumors and compare their results and treatment policy with those described in the literature, particularly with regard to the higher postoperative shunt insertion rates, which have led some authors to the routine use of preoperative third ventriculostomy.
Methods
The clinical records of 180 children treated for posterior fossa tumors in the Department of Pediatric Neurosurgery of the National Institute of Neurosurgery, Budapest, Hungary, between 1990 and 2000 were retrospectively reviewed.
Conclusions
The low postoperative shunt insertion rate in our series (15.5%) led us to believe that the routine use of preoperative third ventriculostomy is not entirely justified. Factors such as patient's age and tumor type, which showed a statistically significant association with the postoperative shunt requirement in our study, should be considered when the decision regarding treatment is made.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is well known that children with posterior fossa tumors are predisposed to hydrocephalus [19]. A proportion of the patients will require a CSF diversion procedure at some time during the course of their illness. However, the management of hydrocephalus in children with resectable posterior fossa tumors is controversial [20]. Some authors advocate preoperative shunts [1, 2, 14], but it is also reported that the insertion of a shunt in the presence of a posterior fossa neoplasm can lead to upward herniation and hemorrhage into the tumor [5, 11, 12], and to metastases in the peritoneal cavity [6]. Others recommend external ventricular drainage (EVD) [8, 11, 15, 17, 18].
In the last decade, neuroendoscopy became a routine surgical tool in the hands of pediatric neurosurgeons [7, 9]. A recent study by Sainte-Rose et al. reports the routine use of preoperative third ventriculostomy in patients with triventricular hydrocephalus due to space-occupying lesions of the posterior fossa [16].
In the Department of Pediatric Neurosurgery of the National Institute of Neurosurgery, Budapest, Hungary, we treat patients with posterior fossa tumors by carrying out early surgery, which means direct excision of the tumors, possibly followed by third ventriculostomy or VCSF shunt placement in cases of persistent hydrocephalus. Preoperatively we use dehydration without steroids and, if needed in an emergency, EVD.
In the present study we analyze the factors that predispose to persistent hydrocephalus and present our postoperative shunt insertion rate. We excluded those few patients who had undergone a CSF shunting procedure preoperatively.
Patients and methods
After excluding 6 shunted patients and 2 patients having undergone endoscopic third ventriculostomy preoperatively, we retrospectively reviewed the clinical records of 180 pediatric patients who were operated on because of resectable posterior fossa tumors in our department between January 1990 and December 2000. The ages ranged from 3 months to 16 years. The mean was 7.4 years and the median was 7 years. The majority of children were boys (57%) and all of the patients underwent preoperative CT and/or MRI. The radiological reports were reviewed. The extent of tumor removal was determined according to the operation notes and the postoperative imaging. The number and timing of EVD, ventriculo-peritoneal shunts and endoscopic third ventriculostomies were noted. We recorded all the postoperative complications that could be related to CSF circulation disorders. The duration of follow-up ranged from 1 to 12 years, with a mean of 6.5 years.
The ratios of children requiring postoperative shunts or endoscopic third ventriculostomies in different subgroups were compared using the Fisher's exact test. Relative risks (RR) and the corresponding 95% confidence intervals (CI) were also calculated. Statistical correction for multiple comparisons was not applied.
Results
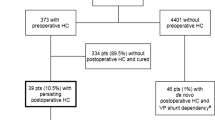
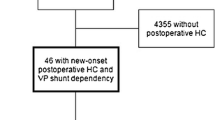
Hydrocephalus on admission CT and/or MR scan was documented in 137 patients (76%). In 129 patients (94% of hydrocephalus group) it was associated with the symptoms or clinical signs of raised ICP. Seven out of the 43 patients without preoperative hydrocephalus developed hydrocephalus postoperatively. Histologically, astrocytoma was the most common tumor (41%, n=74), followed by medulloblastoma (39%, n=71), ependymoma (11%, n=19) and others (8%, n=16).
Twelve shunts (6.7%) out of180 were inserted within the first 6 postoperative weeks after primary posterior fossa tumor surgery and there were 16 (8.9%) late shunt requirements (between 2 and 83 months). Eight of these 16 patients who had late shunt requirement underwent shunt insertion as a treatment for hydrocephalus due to local tumor recurrence. One of these 8 children was shunted without tumor resection due to non-resectable tumor recurrence, and 7 patients were reoperated for tumor resection. Shunting occurred before (2 patients) or after (5 patients) the resection. We noted 8 other late shunt requirements. Two of these children developed tumor recurrence some years after the late shunting procedure and were operated.
On these grounds we distinguish three categories of postoperative shunts:
-
1.
Direct primary postoperative shunts: 12 (6.7%)
-
2.
Shunts due to tumor recurrence: 8 (4.4%)
-
3.
Other late shunts: 8 (4.4%)
The 28 definitive postoperative CSF drainage procedures (15.5%), simply called shunts, comprised 26 VP shunts and 2 endoscopic third ventriculostomies (1 late). The low number of endoscopic procedures was connected with the instrumentation that was regularly available in only the last 2 years of the period examined.
Twenty-seven patients (27/180=14.9%) underwent EVD: 13 preoperatively (8.3%), 2 intraoperatively (1%), and 12 postoperatively (6.7%). Eleven out of the 27 had a postoperative shunt.
The definitive postoperative CSF drainage procedure (VP shunt or endoscopic third ventriculostomy) requirement was analyzed in the various groups of patients divided into different categories. This analysis was performed on direct primary postoperative shunts (1st category), shunts due to tumor recurrence (2nd category), and other late shunts (3rd category).
The mean age of patients requiring postoperative shunts was lower (5.3 years) than those who did not require shunt placement (7.9 years). In the primary postoperative shunt category the mean age was 5.6 years, in the tumor recurrence category 5.2 years, and in the case of other late shunts 5.3 years. Thirty-one percent of the children under 3 years of age required postoperative shunts vs. 12% of the children over 3 years of age, which is a statistically significant difference (p=0.0078, RR=2.68, CI: 1.38–5.20). The ratios were 14% vs. 5% for the 1st category (RR=2.96, CI: 1.00–8.77), 14% vs. 2% for the 2nd category (RR=6.90 CI: 1.73–27.53), and 3% vs. 5% for the 3rd category (RR=0.59, CI: 0.08–4.66).
With regard to the tumor type, it was apparent that the incidence of shunt insertions was found to be the highest in children with ependymomas (37%, n=7), followed by those in the mixed group (25%, n=4), which included 1 choroid plexus papilloma, 1 choroid plexus carcinoma, 1 glioblastoma, and 1 teratoma, those with medulloblastomas (17%, n=12), and the lowest was in patients with astrocytomas (7%, n=5). The rates were significantly different between these groups (p=0.007). In the case of primary postoperative shunts the shunt insertion rate was also highest in the group with ependymomas (11%), followed by medulloblastomas (8%), and astrocytomas (3%). In the tumor recurrence category the rate was 26% for ependymomas, 3% for medulloblastomas, and 1% for astrocytomas. The tendency was similar among the patients below 3 years of age. The histopathological diagnosis of the patients in the "other late shunts" category is demonstrated in Table 1.
Twenty-one (15.3%) of the children who showed hydrocephalus on their admission CT scan underwent postoperative shunting, while 7 (16%) of the patients without preoperative hydrocephalus required a shunt postoperatively (p=1.0000, RR=0.94, CI: 0.43–2.06). However, if we consider primary shunts only, we find a closely significant relationship: 8.7% (n=12) and 0%, respectively (p=0.072). But 100% of the patients in the primary shunt group had hydrocephalus on their admission CT, as did 63% (n=5) in the recurrence group and 50% (n=4) in the other late shunt group.
The group without preoperative hydrocephalus consisted of 43 patients and 4 of them were less than 3 years old. Histologically, 44% had astrocytomas, 32% had medulloblastomas, 19% had other types of tumor, and 5% had ependymomas. There were 3 patients with meningitis. Seven children (16%) were shunted, 3 of whom had medulloblastomas, 1 had an astrocytoma, 1 had a glioblastoma, 1 had an ependymoma, and 1 had a plexus carcinoma. The ages of these shunted patients ranged from 1 to 12 years, and there were 3 patients (7%) below 3 years. One of the children who had meningitis was shunted, and he was 1 year old.
One hundred and fifty-four patients (85%) had tumors that involved the midline structures, and 16% of them required shunts (n=24: 11 primary (7%), 7 due to recurrence, 6 other late shunts) (RR=1.01, CI:0.38–2.68). In the primary shunt group the tumor involved the midline in 92% of the patients (n=11) vs. 8% (n=1) in whom the midline was not involved. The shunt rate was 75% (n=6) vs. 25% (n=2) in the recurrence shunt group and 88% (n=7) vs. 12% (n=1) in the group with other late shunts. Eleven patients had tumors that exclusively involved the cerebellar hemisphere, and none of them required postoperative shunt insertion. Sixty-four percent (n=7) of these patients had pilocytic astrocytomas, and the remaining 36% (n=4) had medulloblastomas. The observed differences between different localizations of tumors in patients requiring shunts were not statistically significant.
According to the extent of tumor excision, we found that the shunt requirement was higher when a partial excision was achieved (18%, i.e., 8% primary, 5% recurrence, 5% others), than in cases of macroscopically complete excision (14%: i.e., 6% primary, 4% recurrence, 4% others). The difference was not significant (p=0.41, RR=0.76, CI: 0.39–1.50). There was a bigger difference between the shunt requirements with regard to the extent of tumor excision in patients with astrocytomas (children with complete tumor removal had 4.3% shunt insertion rate compared with 11% following partial removal) (RR=0.38, CI: 0.07–2.15).
Thirteen patients (7%) who developed postoperative CSF leak through the wound had a shunt insertion rate of 31% (n=4, p>5%, RR=2.14, CI: 0.87–5.24). In this group there were no primary shunts, but there were 2 shunts due to recurrence, and 2 other late shunts.
We noted 13 children (7%) who had postoperative pseudomeningoceles with a shunt insertion rate of 23% (n=3, i.e., 3 primary shunts; p>5%, RR=1.52, CI: 0.53–4.38).
Among the 17 patients (9.7%) who had meningitis, 18% (n=3) required shunts: 1 primary shunt (6%) and 2 due to recurrence (12%) (p>5%, RR=1.12, CI: 0.38–3.31). From a histological point of view, we found 1 ependymoma (14% of shunted ependymomas), 1 medulloblastoma (8% of shunted medulloblastomas), no astrocytomas, and 1 malignant teratoma in the meningitis group.
Examining the different postoperative complications in the subgroup of patients below 3 years, we found higher rates: 14% (n=5) and 12% (n=4) for liquorrhea and meningitis, respectively, and 12% (n=4) for pseudomeningoceles, but none of these elevated percentages of postoperative complications were statistically significant (RR=2.59, CI: 0.90–7.43; RR=1.38, CI:0.48–3.94; RR=1.82, CI:0.59–5.56, respectively). Otherwise in this subgroup the patients with meningitis had a higher shunt insertion rate (total 50%: 1 primary shunt, 17%; 2 due to recurrence).
Children who underwent preoperative or postoperative EVD (n=27) had a shunt insertion rate of 41% compared with 11% of those who did not have EVD. This is a statistically significant difference (RR=3.67, CI: 1.94–6.94). The patients requiring definitive postoperative shunts had the EVD in place for 19.1 days on average, compared with 8.2 days among children who did not require shunts. Children having EVD in place for 8 days or less had a shunt insertion rate of 21.4%; those who required EVD for longer than 8 days had a shunt insertion rate of 62% (p=0.054).
Discussion
Shunt rate and timing, tumor recurrence
We had 12 patients (6.7%) out of the 180 patients who required direct primary postoperative shunts within 6 postoperative weeks. Eight patients (4.4%) were shunted due to tumor recurrence and 8 were other late shunts (4.4%). Even the overall 15.5% shunt insertion rate is lower than the 17–40% rate reported in more recent studies [3, 4, 13, 14, 16, 17], but with regard to the 6.7% rate of direct postoperative shunts we found a large difference. Only the 6.7% of the patients who underwent posterior fossa tumor removal developed hydrocephalus that required shunts directly after tumor removal. With regard to the postoperative natural shunt requirement, it is important to separate this group of early shunts from those that were realized because of tumor recurrence. Tumor recurrences that are in the early stages and have not yet been diagnosed radiologically, may play a role in the development of other late hydrocephalus that requires a shunt.
Age at diagnosis
The age at tumor diagnosis was found to be a significant predictor of postoperative shunt placement. The lower mean age of shunted patients and the higher shunt insertion rate in patients below 3 years show that the young children have a more express inclination to develop hydrocephalus that requires a shunt. Our results are similar to those reported in several other series [3, 10, 13].
Tumor type
In our study we found significant correlation between tumor type and the subsequent need for a shunt. The shunt requirement was the highest among ependymoma cases, followed by medulloblastomas, and the lowest was among patients with astrocytomas. This is in agreement with the data reported by Kumar and colleagues [10], but other investigators found no significant correlation [3, 4]. The same tendency was observed in the subgroup below 3 years of age.
Preoperative hydrocephalus
While most of the children had hydrocephalus at the time of diagnosis, the presence of preoperative hydrocephalus has not been found to be a significant factor for predicting the need for shunt placement, and even if the issue is restricted to primary shunts, only a marginal significance was found. These results are similar to those reported in other studies [3, 4, 17]. We had 137 patients presenting hydrocephalus on the preoperative imaging and 84.7% of them did not require any shunts after tumor resection. If we had performed endoscopic third ventriculostomy in all 137 patients, it would have led to 116 unnecessary operations.
Tumor location
In our series there was no statistically significant difference between the shunt requirements of patients with tumors involving vs. not involving the midline. This is consistent with the findings of some authors [4, 17], but other investigators have found a statistically significant difference [13]. We also had 11 patients whose tumors exclusively involved the cerebellar hemispheres and none of them required shunt insertions. Histologically, the majority of these were pilocytic astrocytomas (64%) and the rest were medulloblastomas.
Extent of resection
The extent of tumor resection, as determined by the surgeons' comments in the operative reports and the postoperative imaging, was not a statistically significant predictor of the need for a postoperative shunt. These results are similar to those reported by Cully et al. [3], but other studies report a statistically significant correlation [4, 10]. Stein et al.'s [19] evaluation of patients with astrocytomas, which was carried out before the routine use of CT and MRI imaging, reported exactly the reverse.
Pseudomeningocele, CSF leak, and infection
Examining the complications we found that in the direct postoperative shunt group there was a higher shunt insertion rate in patients with pseudomeningoceles and meningitis who were below 3 years. There was also a higher incidence of postoperative CSF leak and meningitis in children below 3 years. But the observed differences were not statistically different. This is in disagreement with the study of Cully et al., but similar to the results of Kumar et al. [10].
External ventricular drainage
In contrast to other studies [3, 4, 10], there was a statistically significant difference between the use of ventricular drainage and the postoperative shunt requirement. Children who underwent preoperative or postoperative EVD had a higher shunt insertion rate than those who did not have EVD. The correlation was near significant in the case of the duration of the EVD. Children having EVD in place for 8 days or less had a lower shunt insertion rate than those who required EVD for longer than 8 days.
Conclusion
We manage hydrocephalus due to posterior fossa tumors in children by early craniotomy for excision of the tumor. Preoperatively we use dehydration without steroids and emergency EVD in children in a critical condition because of hypertensive hydrocephalus.
In this retrospective analysis the low age at diagnosis, the tumor type, and the presence EVD were statistically significant predictors for postoperative shunt requirement. By contrast, preoperative hydrocephalus, tumor location, extent of tumor resection, postoperative pseudomeningocele, and CSF leakage or infection showed no significant association with subsequent shunt requirement.
The low postoperative shunt insertion rate in our series (15.5% all together, 6.7% separated from tumor recurrence group and other late shunts) is rare enough to think that the routine use of the preoperative third ventriculostomy is not absolutely justified. The decision about whether to use it should not be based exclusively on the presence of preoperative hydrocephalus. Other factors like patient age and tumor type potentially influencing shunt requirement should also be considered. We do not debate the effectiveness of the third ventriculostomy in the management of hydrocephalus in children with posterior fossa tumors, but we think that preoperatively it should only performed in patients with a known high risk of needing such an intervention.
References
Albright L (1983) The value of pre-craniotomy shunts in children with posterior fossa tumours. Clin Neurosurg 30:278–285
Albright L, Reigel DH (1977) Management of hydrocephalus secondary to posterior fossa tumors. J Neurosurg 46:52–55
Culley DJ, Berger MS, Shaw D, Geyer R (1994) An analysis of factors determining the need for ventriculoperitoneal shunts after posterior fossa tumor surgery in children. Neurosurgery 34:402–408
Dias MS, Albright AL (1989) Management of hydrocephalus complicating childhood posterior fossa tumors. Pediatr Neurosci 15:283–290
Epstein F, Murali R (1978) Pediatric posterior fossa tumors: hazards of the preoperative shunt. Neurosurgery 3:348–350
Hoffman HJ, Hendrick EB, Humphreys RP (1976) Metastasis via ventriculoperitoneal shunt in patients with medulloblastoma. J Neurosurg 44:562–566
Hoph NJ, Grunert P, Fries G et al (1999) Endoscopic third ventriculostomy: outcome analysis of 100 consecutive procedures. Neurosurgery 44:795–806
Imielinski BL, Kloc W, Wasilewski W, Liczbik W, Puzyrewski R, Karwacki Z (1998) Posterior fossa tumors in children—indications for ventricular drainage and for V-P shunting. Childs Nerv Syst 14:227–229
Jones RF, Stening WA, Brydon M (1990) Endoscopic third ventriculostomy. Neurosurgery 26:86–92
Kumar V, Phipps K, Harkness W, Haward RD (1996) Ventriculo-peritoneal shunt requirement in children with posterior fossa tumours: an 11-year audit. Br J Neurosurg 10:467–470
McLaurin RL (1983) Disadvantages of the preoperative shunt in posterior fossa tumors. Clin Neurosurg 30:286–294
McLaurin RL (1985) On the use of pre-craniotomy shunting in the management of posterior fossa tumours in children. Concepts Paediatr Neurosurg 6:1–5
Papo I, Caruselli G, Luongo A (1982) External ventricular drainage in the management of posterior fossa tumors in children and adolescents. Neurosurgery 10:13–15
Raimondi AJ, Tomita T (1981) Hydrocephalus and infratentorial tumors. Incidence, clinical picture, and treatment. J Neurosurg 55:174–182
Rappaport ZH, Shalit MN (1989) Perioperative external ventricular drainage in obstructive hydrocephalus secondary to infratentorial brain tumors. Acta Neurochir 96:118–121
Sainte-Rose C, Cinalli G, Roux FE, Maixner W, Chumas PD, Mansour M, Carpentier A, Bourgeois M, Zerah M, Kahn AP, Reiner D (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95:791–797
Schmid UD, Seiler RW (1986) Management of obstructive hydrocephalus secondary to posterior fossa tumors by steroid and subcutaneous ventricular catheter reservoir. J Neurosurg 65:649–653
Shalit MN, Ben Ari Y, Enyan N (1979) The management of obstructive hydrocephalus by the use of external ventricular drainage. Acta Neurochir (Wien) 47:161–172
Stein BM, Tenner MS, Fraser RA (1972) Hydrocephalus following removal of cerebellar astrocytomas in children. J Neurosurg 36:763–768
Taylor WAS, Todd NV, Leighton SEJ (1992) CSF drainage in patients with posterior fossa tumours. Acta Neurochir (Wien) 117:1–6
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bognár, L., Borgulya, G., Benke, P. et al. Analysis of CSF shunting procedure requirement in children with posterior fossa tumors. Childs Nerv Syst 19, 332–336 (2003). https://doi.org/10.1007/s00381-003-0745-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-003-0745-x