Abstract
The aim is to investigate, by means of speckle tracking echocardiography, left ventricular (LV) contractile function at rest and during dipyridamole stress in patients with coronary microvascular dysfunction (CMD). 59 patients (39% women, mean age 65.6 ± 6.1 years) with history of chest pain and without obstructive coronary artery disease (CAD) underwent dipyridamole stress echocardiography. Coronary flow was assessed in the left anterior descending coronary artery. Coronary flow reserve (CFR) was determined as the ratio of hyperaemic to baseline diastolic coronary flow velocity. CMD was defined as CFR < 2. Global longitudinal strain (GLS) was measured at rest and at peak dose. Nineteen patients (32%) among the overall population showed CMD. Baseline GLS was significantly lower in patients with CMD (– 16.8 ± 2.7 vs. – 19.1 ± 3.1, p < 0.01). A different contractile response to dipyridamole infusion was observed between the two groups: GLS significantly increased up to peak dose in patients without CMD (from – 19.1 ± 3.1 to – 20.2 ± 3.1, p < 0.01), and significantly decreased in patients with CMD (from – 16.8 ± 2.7 to – 15.8 ± 2.7, p < 0.01). There was a significant inverse correlation between CFR and ∆GLS (r = – 0.82, p < 0.01). Rest GLS and GLS response to dipyridamole stress are markedly impaired among patients with chest pain syndrome, non-obstructive CAD and CMD, reflecting subclinical LV systolic dysfunction and lack of LV contractile reserve due to underlying myocardial ischemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chest pain in patients without obstructive coronary artery disease (CAD) is a frequent problem encountered in clinical practice [1]. Coronary microvascular dysfunction (CMD) is a potential mechanism of myocardial ischemia in this subset of patients [2].
The main underlying components of CMD are sympathetic activation, endothelial and smooth muscle cells dysfunction, and arteriolar remodeling, which determine impaired coronary vasodilator function and reduced coronary flow reserve (CFR). Traditional risk factors, first diabetes, but also aging, hypertension, obesity, dyslipidemia and insulin resistance, as well as chronic inflammation, have been shown to favor functional and structural alterations leading to this impaired microvascular response.
In patients without obstructive CAD, CMD can be identified through a reduced CFR, assessed by pulsed Doppler echocardiography associated with vasodilatory stress.
In these patients, CFR has proven to add incremental prognostic value to the risk stratification achieved with clinical and angiographic data [3]. Among these patients, regional and global left ventricular (LV) contractile function is often preserved at baseline and during stress. This may be explained by the fact that microvascular abnormalities do not uniformly involve all the myocardium, but are distributed in a scattered manner [2]. Thus, ischemic myocardium can be non-detectable, because surrounded by healthy and normally functioning tissue.
In the era of new ultrasound technologies, speckle tracking echocardiography (STE) is able to detect subclinical LV systolic dysfunction in early-stage cardiovascular diseases, when LV ejection fraction (LVEF) is still normal [4].
The aim of the present study was to investigate the changes in global longitudinal strain (GLS) evaluated by STE during dipyridamole stress echocardiography, in patients with CMD and non-obstructive coronary disease.
Methods
Patients
Fifty-nine patients referred to the Department of Cardiology of “Umberto I” Hospital (Nocera Inferiore, Italy) were prospectively enrolled from September 2019 to March 2020.
Patients were selected according to the following criteria: history of chest pain; electrocardiogram (ECG) changes or myocardial perfusion scintigraphic defects during effort; coronary angiogram showing absent or non-significant (< 50% quantitatively assessed) stenosis in any major vessel or secondary branch.
Patients with acute coronary syndrome and myocardial diseases were excluded.
All patients underwent pharmacological stress test with dipyridamole (0.84 mg/kg over 6 min) within 15 days of coronary angiography. This evaluation was performed on antianginal treatment. Stress echocardiographic data were collected and analyzed by echocardiographers not involved in patients’ care. Data were entered into the databank on the same day of test performance.
The study was conducted in accordance with the Declaration of Helsinki on ethical principles for medical research involving human subjects. All patients provided their written informed consent before undergoing stress echocardiography and authorized physicians to use their clinical data.
Stress echocardiography
Transthoracic echocardiography study was performed using the commercially available ultrasound machine GE Vivid S70, equipped with multifrequency, phased-array sector scan probe M5Sc, and with second harmonic technology.
A standard, baseline echocardiography was recorded before starting the stress study. Subsequently, high-dose dipyridamole stress test (up to 0.84 mg/Kg over 6 min) was performed. Blood pressure and ECG were acquired at baseline and each minute during the test.
Pharmacologic stress test was stopped for one of the following reasons: development of new or worsening wall motion abnormalities on echocardiography; ST-segment shift > 2.5 mV; severe chest pain; other intolerable symptoms; systolic blood pressure > 220 mmHg or diastolic blood pressure > 120 mmHg; decrease in blood pressure > 30 mmHg; supraventricular arrhythmias, atrial fibrillation, ventricular arrhythmias, or frequent and polymorphous premature ventricular beats.
In order to evaluate global and regional LV systolic function, standard views for echocardiographic stress testing (parasternal long axis, parasternal short axis at level of papillary muscles, apical 4-, 2-, and 3-chamber) were obtained at rest and at peak hyperemia. Global LV contractile function was calculated by Simpson biplane method. Segmental contractile function was graded for each of the 17 segments of the LV as 1 when normal, 2 when hypokinetic, 3 when akinetic, and 4 when dyskinetic. Wall motion score index (WMSI) was derived by dividing the sum of individual visualized segment scores by the number of visualized segments.
Baseline and peak stress LV GLS were calculated using two-dimensional STE, on ECG-gated, high quality apical 4-, 2-, and 3-chamber images, with gray-scale frame rate kept between 30 and 70 frames/s. Strain values and curves were obtained for all 17 myocardial segments, and LV GLS value was generated by the software. A bull’s eye, which intuitively displays segmental and global peak systolic longitudinal strain, was also provided by the system.
A specific projection (a modified apical 2-chamber view, obtained sliding upwards and medially the probe, and slightly turning it counterclockwise) was collected in order to assess left anterior descending (LAD) artery flow. Coronary flow was sampled at rest and at peak stress in the mid-distal portion of the LAD, under the guidance of color Doppler flow mapping. In all patients, color-coded blood flow from the LAD was visualized at baseline, thus there was no need to use contrast enhancement (SonoVue). CFR was defined as the ratio between hyperemic and basal peak diastolic coronary flow, and it was considered normal when > 2. CFR and GLS analysis were performed by different operators, blinded to the other data, to avoid bias.
Statistical analysis
The baseline characteristics are shown as means and standard deviations for continuous variables and as numbers and percentages for categorical variables. Unpaired t test and paired t test were, respectively, used to analyze differences in continuous variables between the 2 groups (with and without CFR), and between rest and peak hyperemia in each group. Analysis of categorical data was performed using the Chi-squared test.
Linear regression analysis and partial correlation tests by Pearson’s method were done to assess univariate relations. To identify independent determinants of CFR and LV GLS, their individual association with clinically relevant and echocardiographic variables was assessed by multivariate analysis. The included variables were diabetes and arterial hypertension. All tests of hypotheses were two-sided and p value < 0.05 was considered statistically significant.
Results
Fifty-nine patients were enrolled in the study, of which 39% were women. The mean age was 65.6 ± 6.1 years. Nineteen patients (32%) among the overall population showed CMD. There were no significant differences in baseline characteristics, including pharmacological treatment, between patients with and without CMD (Table 1). Dipyridamole infusion was well tolerated, and CFR was successfully performed in all patients. None of them developed new or worsening wall motion abnormalities on echocardiography.
Echocardiographic data at baseline and during stress are, respectively, reported in Tables 1 and 2. GLS, at baseline, was significantly lower in patients with CMD (– 16.8 ± 2.7 vs. – 19.1 ± 3.1, p < 0.001). A different response to dipyridamole stress echocardiography was observed between the two groups (Figs. 1, 2, Table 3): GLS significantly increased up to peak dose in patients without CMD (from – 19.1 ± 3.1 to – 20.2 ± 3.1, p < 0.001), whereas a significant decrease from rest to peak dose was observed in patients with CMD (from – 16.8 ± 2.7 to – 15.8 ± 2.7, p < 0.001). There was a marked inverse correlation between CFR and ∆GLS (r = – 0.82, p < 0.001; Fig. 3), using Pearson’s method. Univariate linear regression analysis confirmed a significant correlation between CFR and ∆GLS (standardized beta coefficient – 0.823; p < 0.001). In a multivariate analysis, diabetes was the only variable independently related to lower CFR levels (p = 0.003).
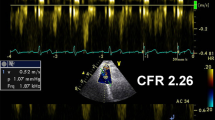
Global longitudinal strain (GLS) increase during dipyridamole stress echocardiography in a patient without coronary microvascular dysfunction. Coronary flow is sampled in the mid-distal portion of the left anterior descending (LAD) at rest (A) and at peak stress (B) under the guidance of color Doppler flow mapping. Peak diastolic LAD flow more than doubles at peak dose than baseline, indicating a normal coronary flow reserve. GLS value at peak stress (D) is higher than rest value (C)
Global longitudinal strain (GLS) decrease during dipyridamole stress echocardiography in a patient with coronary microvascular dysfunction. Coronary flow is sampled in the mid-distal portion of the left anterior descending (LAD) at rest (A) and at peak stress (B) under the guidance of color Doppler flow mapping. Peak diastolic LAD flow does not at peak dose, indicating an abnormal coronary flow reserve. GLS value at peak stress (D) is lower than rest value (C).
Scatter plot of the association between global longitudinal strain (GLS) reserve (∆GLS) and coronary flow reserve (CFR). Patients with CMD (low CFR in absence of obstructive coronary artery disease) show no contractile response of the left ventricle, characterized by GLS worsening from rest to peak dose of dipyridamole
Discussion
Patients with chest pain undergoing invasive coronary angiography are found to have normal-appearing coronary arteries (defined as lesions < 50%) up to 60% of cases [5]. In a substantial proportion of these patients, angina symptoms are due to other underlying mechanisms, different from coronary artery narrowing, including CMD [6, 7].
CMD can be detected by non-invasive tools, such as PET imaging, dipyridamole stress echocardiography, and other emerging imaging modalities in this field, like cardiac magnetic resonance and computed tomography [1]. In the present study, the non-invasive parameter chosen to identify CMD was the reduced CFR evaluated by dipyridamole stress echocardiography. The use of dipyridamole allowed to obtain good quality images at peak hyperemia, avoiding an excessive increase in heart rate, which would have affected speckle tracking analysis.
CFR is dependent on the combined effects of epicardial coronary stenosis and CMD. In the absence of obstructive coronary artery narrowing, impaired CFR reflects the presence of microvascular dysfunction. Therefore, CFR can be useful to assess CMD in patients with chest pain but no obstructive CAD [8]. According to both 2019 European guidelines for diagnosis and management of chronic coronary syndromes [9] and 2021 American guidelines for the evaluation and diagnosis of chest pain [10], a non-invasive measurement of CFR by means of transthoracic echocardiography and vasodilatory stress is advised in patients with suspected ischemia and no obstructive coronary artery disease (INOCA), with class of recommendation IIb.
Patients with CMD have traditionally been considered at “low-risk”. However, this issue remains controversial. This population is heterogeneous, including truly normal, smooth coronary arteries, and mild or moderate, isolated or multiple, single or multivessel non-significant coronary stenosis. It is reasonable to expect a less benign prognosis for patients with coronary disease, even if non-significant. Moreover, it has been shown that patients with chest pain and non-obstructive CAD are predominantly women, and their risk of cardiac events is higher when compared to asymptomatic subjects [11, 12]. Supporting this finding, the WISE study demonstrated that women with reduced CFR assessed by adenosine, had increased risk of major adverse outcomes (including cardiac death, stroke, and new onset of heart failure) over a 5.4-year follow-up period [13].
In the absence of obstructive CAD, CMD do not normally give rise to regional wall motion abnormalities during stress, even when ST-segment changes and positive perfusion scan are present [14,15,16,17,18,19]. However, it has been proven that impaired CFR in the LAD evaluated by dipyridamole stress echocardiography is associated with a less benign long-term outcome and a higher risk of hard events in patients with known or suspected CAD and negative stress echocardiography by wall motion criteria [20, 21].
CMD may contribute to subtle changes in myocardial contractile function, non-detectable with the traditional indices of LV systolic function. LV contractile dysfunction becomes more apparent using GLS, a parameter of myocardial deformation which is able to detect subclinical systolic impairment when LVEF is still normal.
The overall population of this study shows a negative stress echocardiography by traditional wall motion criteria; however, GLS at baseline is significantly lower in patients with impaired CFR if compared to controls, reflecting the presence of a LV subtle contractile dysfunction in case of CMD. A previous study by Michelsen et al. [22] found no association between baseline GLS and CFR in women with angina and non-obstructive CAD. Similarly, Rodriguez-Zanella et al. [23] recently found no significant difference in rest GLS between patients with and without CFR. However, the hypothesis of subclinical contractile dysfunction in patients with CMD cannot be excluded, since that microvascular dysfunction is one of the known mechanisms of myocardial ischemia, and that these patients show a poorer prognosis.
A novel finding emerging from the present study it the opposite response to dipyridamole stress echocardiography observed between the two groups. In particular, patients without CMD exhibit a certain contractile response to hyperemic stress evaluated by STE (mean improvement in GLS, % − 1.18 ± 0.84). Conversely, a significant impairment in GLS from rest to peak dose is observed among patients with CMD (∆GLS, % + 1.04 ± 0.82), which could be explained by a supply/demand mismatch of myocardial perfusion during stress [22, 24]. The linear correlation analysis between CFR and ∆GLS confirms these data: as the CFR increases, the LV contractile reserve improves, and vice versa (Fig. 3).
The results of the present study are in agreement with the data emerging from a recent study by Jovanovic et al [25]., who demonstrated that CFR, resting, peak, and ∆GLS were all markedly impaired in a population of 70 women with cardiac syndrome X compared to controls.
In conclusion, rest GLS and GLS response to dipyridamole stress are impaired among patients with chest pain syndrome, non-obstructive CAD and CMD, reflecting subclinical LV systolic dysfunction and lack of LV contractile reserve due to underlying myocardial ischemia.
The main limitation of this study is that it has been carried out in a single center, and the sample size is too small to drive definitive general conclusions. Further and larger studies are needed to clarify the association between baseline GLS and CFR, and to explain the mechanisms underlying the association between GLS reserve and CMD.
Moreover, it would be interesting to follow the study population over time in order to establish if GLS at rest and after dipyridamole stress echocardiography may be further useful tools to stratify the cardiovascular risk and choose the best therapy in patients with CMD.
References
Schindler TH, Dilsizian V (2020) Coronary microvascular dysfunction: clinical considerations and noninvasive diagnosis. JACC Cardiovasc Imaging 13(1 Pt 1):140–155
Crea F, Camici PG, Bairey Merz CN (2014) Coronary microvascular dysfunction: an update. Eur Heart J 35(17):1101–1111
Sicari R, Rigo F, Cortigiani L, Gherardi S, Galderisi M, Picano E (2009) Additive prognostic value of coronary flow reserve in patients with chest pain syndrome and normal or near-normal coronary arteries. Am J Cardiol 103(5):626–631
D’Andrea A, Sperlongano S, Pacileo M, Venturini E, Iannuzzo G, Gentile M, Sperlongano R, Vitale G, Maglione M, Cice G, Maria Sarullo F, Di Lorenzo A, Vigorito C, Giallauria F, Picano E (2020) New ultrasound technologies for ischemic heart disease assessment and monitoring in cardiac rehabilitation. J Clin Med 9(10):3131
Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, Brindis RG, Douglas PS (2010) Low diagnostic yield of elective coronary angiography. N Engl J Med 362(10):886–895
Camici PG, Gloekler S, Levy BI, Skalidis E, Tagliamonte E, Vardas P, Heusch G (2016) Ivabradine in chronic stable angina: effects by and beyond heart rate reduction. Int J Cardiol 215:1–6
Tagliamonte E, Cirillo T, Rigo F, Astarita C, Coppola A, Romano C, Capuano N (2015) Ivabradine and bisoprolol on Doppler-derived coronary flow velocity reserve in patients with stable coronary artery disease: beyond the heart rate. Adv Ther 32(8):757–767
Tagliamonte E, Rigo F, Cirillo T, Astarita C, Quaranta G, Marinelli U, Caruso A, Romano C, Capuano N (2015) Effects of ranolazine on noninvasive coronary flow reserve in patients with myocardial ischemia but without obstructive coronary artery disease. Echocardiography 32(3):516–521
Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C, Prescott E, Storey RF, Deaton C, Cuisset T, Agewall S, Dickstein K, Edvardsen T, Escaned J, Gersh BJ, Svitil P, Gilard M, Hasdai D, Hatala R, Mahfoud F, Masip J, Muneretto C, Valgimigli M, Achenbach S, Bax JJ (2019) ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41(3):407–477 (Erratum in: Eur Heart J. 41(44):4242)
Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, Blankstein R, Boyd J, Bullock-Palmer RP, Conejo T, Diercks DB, Gentile F, Greenwood JP, Hess EP, Hollenberg SM, Jaber WA, Jneid H, Joglar JA, Morrow DA, O’Connor RE, Ross MA, Shaw LJ (2021) (2021) AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation 144(22):e368–e454
Gulati M, Cooper-DeHoff RM, McClure C, Johnson BD, Shaw LJ, Handberg EM, Zineh I, Kelsey SF, Arnsdorf MF, Black HR, Pepine CJ, Merz CN (2009) Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the women’s ischemia syndrome evaluation study and the St James women take heart project. Arch Intern Med 169(9):843–850
Espersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, Jørgensen E, Kelbæk H, Prescott E (2012) Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 33(6):734–744
Pepine CJ, Anderson RD, Sharaf BL, Reis SE, Smith KM, Handberg EM, Johnson BD, Sopko G, Bairey Merz CN (2010) Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the national heart, lung and blood institute WISE (women’s ischemia syndrome evaluation) study. J American Coll Cardiol 55(25):2825–2832
Zeiher AM, Krause T, Schächinger V, Minners J, Moser E (1995) Impaired endothelium-dependent vasodilation of coronary resistance vessels is associated with exercise-induced myocardial ischemia. Circulation 91(9):2345–2352
Panting JR, Gatehouse PD, Yang GZ, Grothues F, Firmin DN, Collins P, Pennell DJ (2002) Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med 346(25):1948–1953
Lanza GA, Buffon A, Sestito A, Natale L, Sgueglia GA, Galiuto L, Infusino F, Mariani L, Centola A, Crea F (2008) Relation between stress-induced myocardial perfusion defects on cardiovascular magnetic resonance and coronary microvascular dysfunction in patients with cardiac syndrome X. J Am Coll Cardiol 51(4):466–472
Picano E, Pálinkás A, Amyot R (2001) Diagnosis of myocardial ischemia in hypertensive patients. J Hypertens 19(7):1177–1183
Cannon RO 3rd, Bonow RO, Bacharach SL, Green MV, Rosing DR, Leon MB, Watson RM, Epstein SE (1985) Left ventricular dysfunction in patients with angina pectoris, normal epicardial coronary arteries, and abnormal vasodilator reserve. Circulation 71(2):218–226
Kaski JC, Crea F, Nihoyannopoulos P, Hackett D, Maseri A (1986) Transient myocardial ischemia during daily life in patients with syndrome X. Am J Cardiol 58(13):1242–1247
Rigo F, Cortigiani L, Pasanisi E, Richieri M, Cutaia V, Celestre M, Raviele A, Picano E (2006) The additional prognostic value of coronary flow reserve on left anterior descending artery in patients with negative stress echo by wall motion criteria. A transthoracic vasodilator stress echocardiography study. Am Heart J 151(1):124–130
Rigo F, Sicari R, Gherardi S, Djordjevic-Dikic A, Cortigiani L, Picano E (2008) The additive prognostic value of wall motion abnormalities and coronary flow reserve during dipyridamole stress echo. Eur Heart J 29(1):79–88
Michelsen MM, Pena A, Mygind ND, Bech J, Gustafsson I, Kastrup J, Hansen HS, Høst N, Hansen PR, Prescott E (2018) Coronary microvascular dysfunction and myocardial contractile reserve in women with angina and no obstructive coronary artery disease. Echocardiography 35(2):196–203
Rodriguez-Zanella H, Arbucci R, Fritche-Salazar JF, Ortiz-Leon XA, Tuttolomondo D, Lowenstein DH, Wierzbowska-Drabik K, Ciampi Q, Kasprzak JD, Gaibazzi N, Lowenstein J, Posada-Martinez EL, Arias-Godinez JA, de la Fuente-Mancera JC, Picano E, On Behalf of the Stress Echo Study Group of the Italian Society of Echocardiography and Cardiovascular Imaging Siecvi (2022) Vasodilator strain stress echocardiography in suspected coronary microvascular angina. J Clin Med 11(3):711
Cadeddu C, Nocco S, Deidda M, Pau F, Colonna P, Mercuro G (2014) Altered transmural contractility in postmenopausal women affected by cardiac syndrome X. J Am Soc Echocardiogr 27:208–214
Jovanovic I, Tesic M, Giga V, Dobric M, Boskovic N, Vratonjic J, Orlic D, Gudelj O, Tomasevic M, Dikic M, Nedeljkovic I, Trifunovic D, Nedeljkovic MA, Dedic S, Beleslin B, Djordjevic-Dikic A (2020) Impairment of coronary flow velocity reserve and global longitudinal strain in women with cardiac syndrome X and slow coronary flow. J Cardiol 76(1):1–8
Acknowledgements
All the authors contributed to: (1) conception and design of the article; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tagliamonte, E., Sperlongano, S., Montuori, C. et al. Coronary microvascular dysfunction affects left ventricular global longitudinal strain response to dipyridamole stress echocardiography: a pilot study. Heart Vessels 38, 470–477 (2023). https://doi.org/10.1007/s00380-022-02191-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02191-z