Abstract
To assess aortic valve calcification (AVC) and aortic root calcification (ARC) and to examine their usefulness for predicting major adverse cardiovascular events (MACE). This multicenter prospective cohort study recruited 1187 patients suspected of coronary artery disease (CAD) who underwent coronary computed tomography. MACE included cardiovascular death, myocardial infarction, stroke, revascularization and hospitalization for unstable angina, heart failure or aortic disease. Cox proportional hazard model and C-statistic were used to assess mutual associations between Framingham risk score, coronary artery calcification (CAC) and AVC or ARC with incident MACE. A total of 980 patients (mean age, 65 ± 7 years; female, 45.8%) with assessment of AVC and ARC Agatston scores were analyzed. Among them, 86 developed MACE during a median follow-up of 4.04 years. Cox proportional hazard analyses showed that the presence or severity of AVC and ARC was significantly associated with MACE development after adjusting the CAC Agatston score. Compared with the model of Framingham risk score alone, C-statistics of the model adding AVC or ARC Agatston score to Framingham risk score increased (ΔC-statistic; + 0.013 or + 0.032, respectively). However, they were not superior to the model adding CAC Agatston (ΔC-statistic; − 0.077 and − 0.058, respectively). AVC or ARC on the top of CAC was a predictive factor for increased MACE in patients with suspected CAD. However, an additional model of AVC or ARC score to Framingham risk score was not as effective as that of CAC Agatston score.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery calcification (CAC) assessed using non-contrast cardiac computed tomography (CCT) has been reported to be a coronary atherosclerosis marker and to reflect the total atherosclerosis burden [1, 2]. CAC predicted coronary artery disease (CAD), with high specificity for Agatston score of > 310–400 [3]. Incremental prognostic values were also provided beyond those of traditional cardiovascular risk factors for cardiovascular disease (CVD) morbidity and mortality and helped reclassify patients at risk [4].
During the CCT assessment of patients highly at risk, concomitant aortic valve calcification (AVC) or aortic root calcification (ARC) are frequently observed. AVC is a characteristic of aortic stenosis (AS) and shares some cardiovascular risk factors with CAD [5]. Furthermore, it was reportedly assessed by CCT and the Agatston method, and associated with coronary plaque burden and CAD severity [6, 7]. Moreover, aortic calcium is an established marker of atherosclerosis [8]. Consistent with CAC, the prevalence of thoracic aortic calcification including ARC increased with age, was associated with coronary risk factors, and was correlated closely with CAC [9]. Several reports suggested that AVC and ARC predicted CVD events; however, conflicting results regarding its prognostic values in association with cardiovascular risk factors and CAC were also reported [10,11,12]. The association was a still debate topic. Therefore, we assessed the detailed relationship of AVC or ARC with CAC and examined their usefulness for predicting major adverse cardiovascular events (MACE) in patients suspected of CAD who underwent cardiac CT. Especially, we clarified whether they showed significant predictive values on the top CAC or conventional cardiovascular risk factor model such as Framingham risk scores (FRS).
Materials and methods
Study design
This was a sub-study of the Nationwide Gender-Specific Atherosclerosis Determinants Estimation and Ischemic Cardiovascular Disease Prospective Cohort (NADESICO) study, a prospective, multicenter cohort designed to evaluate the sex difference in the association of coronary atherosclerosis including CAC with MACE [13]. Our study protocol was registered with the UMIN Clinical Trials Registry (UMIN-CTR ID: UMIN000001577) before data were released to the lead author. The protocol and informed consent were approved by the institutional review board of each center including the National Cerebral and Cardiovascular Center (M20-029-7), and written informed consent was obtained from each patient before participation.
Participants
Patients included in this study were enrolled from the cardiology department of each hospital participating in the NADESICO study and were recruited from December 2008 to April 2013 among 15 hospitals in Japan. The inclusion criteria were as follows: (1) 50–74-year-old patients suspected with CAD in a stable setting, who had adequate indications for plain CT and coronary CT angiography and (2) patients without a history of myocardial infarction or coronary artery revascularization. Patients who fulfilled the following criteria were excluded: (1) patients with a history of Kawasaki disease, (2) coronary artery malformation, (3) familial hypercholesterolemia, (4) limited prognosis due to malignant tumors, (5) on dialysis, or (6) under treatment for a serious mental or neurological disorder.
Data collection
Clinical data of diagnostic and therapeutic measures were collected by investigators at each hospital and sent to National Cerebral and Cardiovascular Center. Hypertension was defined as systolic blood pressure (BP) of ≥ 140 mmHg or diastolic BP of ≥ 90 mmHg, or current use of antihypertensive agents. Diabetes mellitus was defined as an adult-onset self-reported history, fasting glucose level of ≥ 126 mg/dl, or usage of insulin or oral glucose-lowering medications. Dyslipidemia was defined as the current usage of any lipid-lowering agents, triglyceride level of ≥ 150 mg/dl, low-density lipoprotein cholesterol of ≥ 140 mg/dl, or high-density lipoprotein cholesterol of ≤ 40 mg/dl in male and ≤ 50 mg/dl in female. Data on smoking habits and medical history were collected using a questionnaire at enrollment. Laboratory examination included complete blood count, lipid profiles and fasting plasma glucose levels.
CT was performed using ≥ 64 channels with electrocardiography gating following the guidelines from the Japanese Circulation Society and institutional protocols. CT imaging was transferred to National Cerebral and Cardiovascular Center through digital imaging and interpreted in a blinded fashion with an independent imaging core laboratory using SYNAPSE VINCENT® (FUJIFILM Medical Co., Ltd., Tokyo, Japan). An experienced radiologist or cardiologist blinded to all clinical data interpreted plain CT scans with CAC, AVC, and ARC scores using the Agatston method. AVC was measured in the aortic valve leaflets and annular calcification [11]. ARC was measured in the part of the aorta lying within 3 cm of the aortic annulus involving the Valsalva sinuses and sinotubular junction, except for AVC [12].
Follow-up
Follow-up was conducted annually from enrollment until March 2020. The attending physician from each hospital checked the presence or absence of MACE. For patients who did not visit the hospital more than once a year, the attending physician of each hospital contacted the patients every year by telephone or mail. MACE was defined as the composite of cardiovascular death, myocardial infarction, stroke, revascularization, and hospitalization for unstable angina, heart failure or aortic disease. Cardiovascular death was defined as death due to myocardial infarction, heart failure, cardiac arrhythmia, sudden cardiac death, aortic disease, and stroke.
Statistical analysis
Continuous data were presented as mean ± standard deviation and categorical data were displayed as a number (%). One-way analysis of variance and chi-squared tests were used to test significant differences between three groups (according to AVC or ARC severity) for continuous and categorical variables, respectively. The relationship between CAC severity (no CAC: CAC Agatston score = 0, mild CAC: 0 < CAC Agatston score < 100; moderate CAC: 100 ≤ CAC Agatston score < 400; severe CAC: 400 ≤ CAC Agatston) and AVC or ARC severity (No: Agatston score = 0, mild: 0 < Agatston score < the 90th percentile value; and severe: the 90th percentile value ≤ Agatston score) were examined by Cochran–Armitage test. The cut-off level of AVC or ARC severity as 90th percentile value was exploratory determined considering the distribution of AVC or ARC Agatston score in this study. The logistic regression model was used to identify CV risk factors associated with the presence (Agatston score > 0) of AVC or ARC or CAC. Kaplan–Meier analysis was used to examine the incidence of MACE based on AVC or ARC severity. The Cox proportional hazard model for MACE was adjusted by age and/or CAC Agatston score. Harrell’s concordance statistic (C-statistic) for predicting MACE was examined by adding AVC and ARC Agatston score (continuous value) to calculated Framingham risk score directly [14] and/or CAC of each patient. This analysis was conducted in overall group and male/female groups. The 95% confidence intervals of C-statistic were estimated using 200 bootstrap samples. Statistical significance was defined as a two-tailed P value of < 0.05. In the analysis of reclassification of Framingham risk score after addition of CAC, AVC or ARC Agatston score, low risk was determined as a risk of < 6%, intermediate risk was 6–20% and high risk was > 20%. Also, Kaplan–Meier analysis and Cox proportional hazard model for MACE adjusted by age and/or CAC Agatston score were also examined using another criteria of AVC or ARC severity according to Agatston score (Agatston score = 0, 0 < Agatston score < 100, 100 ≤ Agatston score) based on previous study in addition to the severity classified by 90th percentile value [15]. Statistical analyses were performed using Stata 17 (StataCorp, College Station, TX, USA).
Results
Cardiovascular risk factors associated with AVC or ARC
A total of 980 patients (mean age, 65 ± 7 years) who were suspected with CAD and available for Agatston score of aortic valve, aortic root and coronary artery were investigated (Supplementary Fig. 1), which comprised 449 (45.8%) females. Patients with severe AVC or severe ARC were older and had hypertension, diabetes mellitus, chronic kidney disease, dyslipidemia, and current or past smoking more frequently (Supplementary Table 1). Multivariable analysis showed advanced age, hypertension, and dyslipidemia were independently associated with AVC, whereas advanced age, diabetes mellitus, dyslipidemia, and current or past smoking habits were independently associated with ARC (Table 1). In contrast, all risk factors except for body mass index ≥ 25 and chronic kidney disease were associated with CAC.
Association of AVC and ARC with MACE
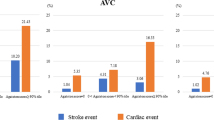
The distribution of Agatston scores in AVC and ARC is shown in Supplementary Fig. 2. The median AVC Agatston score was 0 (interquartile range [IQR]: 0–8.25), with the 90 percentile of 76.45. The median ARC Agatston score was 0 (IQR: 0–25.8), with the 90 percentile of 174.75. Kaplan–Meier analysis for MACE showed that incidences of MACE in patients with severe AVC and ARC were higher than those without (Fig. 1). The Cox proportional hazard model adjusted by age and sex (Model 1, Table 2) showed that the presence and severity of AVC and ARC were significantly associated with increased occurrence of MACE.
Kaplan–Meier analysis for MACE stratified by AVC or ARC severity. Blue line indicates no calcification (Agatston score 0), red line indicates mild calcification (0 < Agatston score < 90th percentile), and green line indicates severe calcification (90th percentile ≤ Agatston score). ARC aortic root calcification, AVC aortic valve calcification, MACE major adverse cardiovascular event
Association of AVC, ARC and CAC with MACE
Figure 2 shows that the severity of AVC or ARC was associated with that of CAC based on the Agatston score (P < 0.01, respectively). The Cox proportional hazard model adjusted by age, sex, and CAC Agatston score (Model 2, Table 2) showed that the presence and severe AVC and the presence, mild, and severe ARC were associated with increased occurrence of MACE. In all patients, the C-statistics were significantly increased by adding ARC assessment to Framingham risk score model (ΔC-statistic; + 0.032, P = 0.01), not significant by adding AVC (ΔC-statistic; + 0.013, P = 0.06) compared with Framingham risk score alone (Table 3). However, C-statistic in combined models adding AVC or ARC Agatston score to Framingham risk score model was significantly lower than that in model of adding CAC Agatston score to Framingham risk score model (ΔC-statistic; − 0.077, P < 0.01, or ΔC-statistic; − 0.058, P < 0.01, respectively). Additional assessment of AVC, ARC, or CAC Agatston score to Framingham risk score led to a net increase of 1, 5, or 9% in patients with MACE, and 1, 3, or 23% in patients without MACE correctly reclassified (net reclassification index, 0.25 ± 0.11, 0.38 ± 0.11, or 0.72 ± 0.11, respectively) (Supplementary Fig. 3). When compared to the combined model with Framingham risk score and CAC Agatston score, additional assessment of AVC and ARC Agatston scores led to a net increase of 5% in patients with MACE and 5% in patients without MACE correctly reclassified (net reclassification index, 0.32 ± 0.11), although C-statistic did not significantly increase.
The relationship between CAC and AVC or ARC according to calcification severity. AVC and ARC; No: Agatston score = 0, Mild: 0 < Agatston score < 90th percentile, Severe: 90th percentile ≤ Agatston score. CAC; No CAC: CAC Agatston score = 0, Mild CAC: 0 < CAC Agatston score < 100, Moderate CAC: 100 ≤ CAC Agatston score < 400, Severe CAC: 400 ≤ CAC Agatston score. ARC aortic root calcification, AVC aortic valve calcification, CAC coronary artery calcification
Sex difference in AVC and ARC
During a follow-up period, 65 male and 21 female patients developed MACE. In contrast to CAC, AVC, and ARC were not independently associated with gender (Table 1). In the stratified analysis by gender, differences were observed in cardiovascular risk factors associated with AVC and ARC (Supplementary Table 2). Age and dyslipidemia were associated with AVC in male, whereas age and hypertension in female. Conversely, age, diabetes mellitus, dyslipidemia, and smoking were associated with ARC in male and all these factors except for dyslipidemia in female. AVC and ARC severities were similarly associated with CAC severity in both sexes (Supplementary Fig. 4). Although MACE was lesser in female than in male, no differences were observed in the relationship of AVC or ARC with MACE between sexes (Supplementary Figs. 5 and 6). In male, C-statistic in the model adding CAC or ARC Agatston score to Framingham risk score significantly increased (ΔC-statistic; + 0.070, P < 0.01, or ΔC-statistics; + 0.035, P = 0.049, respectively, Supplementary Table 3). In female, C-statistic in the model adding CAC, AVC and ARC Agatston score to Framingham risk score significantly increased compared with Framingham risk score alone model (ΔC-statistic; + 0.056, P = 0.045).
Another grading of AVC, ARC using Agatston score 100
Of patients with AVC or ARC, 227 patients had ‘0 < AVC Agatston score < 100’ and 80 patients had ‘100 ≤ AVC Agatston score’, and 257 patients had ‘0 < ARC Agatston score < 100’, 135 patients had ‘100 ≤ ARC Agatston score’. Kaplan–Meier analysis for MACE showed that incidence of MACE in patients with AVC or ARC with ‘100 ≤ Agatston score’ was highest (Supplementary Fig. 7). Cox proportional hazard model adjusted by age, sex, and CAC Agatston score showed that AVC or ARC with ‘100 ≤ Agatston score’ was associated with increased incidence of MACE (Supplementary Table 4).
Discussion
Different pathogenesis between AVC and ARC
Extracoronary calcifications, AVC and ARC, were associated with cardiovascular risk factors differently. Hypertension was strongly associated with AVC, whereas diabetes mellitus and current or past smoking were associated with ARC in this study, suggesting that the formation mechanism may be different between AVC and ARC. Although AVC is a characteristic feature of AS and is not usually considered part of the atherosclerotic process, shared pathological mechanisms of the heart valve calcification and coronary atherosclerosis have been discussed [16]. Hypertension was independently associated with AVC, reflecting age-related degenerative calcification and contribution of mechanical stress through the blood flow [17,18,19,20]. Although chronic kidney disease has also been previously known as a strong factor for AVC formation [19], no significant relationship was observed in our study. This may be explained by including the small number of patients with chronic kidney disease in this NADESICO study. Moreover, aortic calcium is an established marker of atherosclerosis [8]. Consistent with CAC, the prevalence of thoracic aortic calcification including ARC increased with age, was associated with coronary risk factors, and was closely correlated with CAC [21, 22]. Especially, the aortic root has been characterized by its close anatomical proximity to the cardiac chambers and ostium of coronary arteries [10, 20].
AVC and ARC as predictive factors
In this study, the presence of AVC and ARC, especially with higher Agatston scores, was associated with MACE development in patients suspected of CAD. AVC has been reportedly associated with mortality in patients with AS, and the partial association of AVC and ARC with MACE has been previously suggested in the younger population [23,24,25]. Since these results analyzed with AVC and ARC severity using 90th percentile values (AVC 76.45 and ARC 174.75) were almost compatible with those with other categorical severity using Agatston score 100, setting the cut-off points of AVC or ARC around 100 seemed to be useful to predict incidence of MACE in patients with suspicious of CAD and without severe AS. This study was unique due to its usefulness of AVC, and ARC Agatston scores were examined by analyzing C-statistic with the combination of traditional Framingham risk score and CAC Agatston score. Models adding AVC or ARC Agatston scores to Framingham risk score were useful to predict for MACE; however, its usefulness was not superior to the model adding CAC Agatston score. This supports that CAC, based on its representation of the total atherosclerosis burden directly within the coronary arteries, remains a stronger predictor.
Sex differences in AVC and ARC
Factors associated with AVC and ARC seemed to be slightly different in analyzing each sex group. In this study, associations of hypertension and dyslipidemia with both AVC and ARC were observed in female and male, respectively. Erbel et al. reported that female with AVC tended to be accompanied by left ventricular hypertrophy, which may imply its association with HT [26]. Furthermore, AVC was reported to be mainly detected as the aortic valve degeneration in male and fibrosis in female. The etiology and formation of AVC and ARC may vary in sex; however, no difference was observed in the susceptibility of calcification. Moreover, the resulting calcification was associated with clinical outcomes without showing sex differences. This result was in contrast with that in CAC, which was more frequently observed in male by 2.48 times. In the analysis of C-statistic, additional assessment of CAC Agatston score in male and all CAC, AVC and ARC Agatston scores in female to Framingham risk score seemed to be most useful to predict MACE. Pressman et al. recently advanced the notion of “total cardiac calcium” as a predictor of cardiovascular risk [27], and sex difference may be also existed in the notion [28, 29]. However, the sex differences in cardiovascular calcifications are still controversial, and further studies in a larger and broad-spectrum cohort will be needed to clarify differences between the CAC and AVC or ARC based on sex differences.
Limitation
This study has several limitations. First, a small number of MACE occurrences may affect the result, especially in females. Previous studies have reported a similar relatively low incidence of MACE in patients suspected with CAD in Japan [30]. Information regarding medications during follow-up was not obtained and incorporated into the analysis. Second, AS is associated with AVC and one of the important factors which affect the incidence of MACE through angina or heart failure [31]. Most previous studies examined the AVC Agatston score in patients including severe AS [32, 33]. We could not examine the detailed association between AVC and severity of AS because echocardiographic data were not available in the present study. However, based on their medical history records, patients with at least moderate and severe AS were not included in the present study, and the impact of AS on the present findings may be small. Finally, our results from an Asian cohort may not be generalizable to other ethnic groups due to the existence of racial differences in the prevalence and severity of CAC and incidence of CAD [34, 35].
Conclusions
AVC or ARC was associated with specific cardiovascular risk factors and MACE incidence in patients suspected with CAD who underwent cardiac CT. Although AVC or ARC on the top of CAC was a predictive factor for increased MACE, additional effect of AVC or ARC Agatston score to Framingham risk score was modest and the model was not as useful as that of CAC Agatston score.
Abbreviations
- ARC:
-
Aortic root calcification
- AVC:
-
Aortic valve calcification
- AS:
-
Aortic stenosis
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CAC:
-
Coronary artery calcification
- CAD:
-
Coronary artery disease
- CAS:
-
Coronary artery stenosis
- CCT:
-
Cardiac computed tomography
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- eGFR:
-
Estimated glomerular filtration rate
- FRS:
-
Framingham risk score
- HR:
-
Hazard ratio
- MACE:
-
Major adverse cardiovascular events
- OR:
-
Odds ratio
References
Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS (1995) Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. Histopathol Correl Study Circ. 92:2157–2162
Clavel MA, Messika-Zeitoun D, Pibarot P, Aggarwal SR, Malouf J, Araoz PA, Michelena HI, Cueff C, Larose E, Capoulade R, Vahanian A, Enriquez-Sarano M (2013) The complex nature of discordant severe calcified aortic valve disease grading: new insights from combined Doppler echocardiographic and computed tomographic study. J Am Coll Cardiol 62:2329–2338
Leber AW, Knez A, Mukherjee R, White C, Huber A, Becker A, Becker CR, Reiser M, Haberi R, Steinbeck G (2001) Usefulness of calcium scoring using electron beam computed tomography and noninvasive coronary angiography in patients with suspected coronary artery disease. Am J Cardiol 88:219–223
Erbel R, Mohlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, Dragano N, Gronemeyer D, Seibel R, Kalsch H, Brocker-Preuss M, Mann K, Siegrist J, Jockel K, Heinz-Nixdorf Recall Study Investigative Group (2010) Coronary risk stratification, discrimination and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 56:1397–1406
Pohle K, Otte M, Maffert R, Ropers D, Schmid M, Daniel WG, Achenbach S (2004) Association of cardiovascular risk factors to aortic valve calcification as quantified by electron beam computed tomography. Mayo Clin Proc 79:1242–1246
Mahabadi AA, Bamberg F, Toepker M, Schlett CL, Rogers IS, Nagurney JT, Brady TJ, Hoffman U, Truong QA (2009) Association of aortic valve calcification to the presence, extent and composition of coronary artery plaqur burden: from the Rule Out Myocardial Infarction using Computer Assisted Tomography (ROMICAT) trial. Am Heart J 158:562–568
Qian Z, Anderson H, Marvasty I, Akram K, Vazquez G, Rinehart S, Voros S (2010) Lesion- and vessel- specific coronary artery calcium scores are superior to whole-heart Agatston and volume scores in the diagnosis of obstructive coronary artery disease. J Cardiovasc Comput Tomogr 4:391–399
Witteman JC, Kannel WB, Wolf PA, Grobbee DE, Hofman A, D’Agostino RB, Cobb JC (1990) Aortic calcified plaques and cardiovascular disease (the Framingham study). Am J Cardiol 66:1060–1064
Adler Y, Fisman EZ, Shemesh J, Schwammenthal E, Tanne D, Batavraham IRY, Motro M, Tenenbaum A (2004) Spiral computed tomography evidence of close correlation between coronary and thoracic aorta calcifications. Atherosclerosis 176:133–138
Nafakhi H, AI-Nafakh HA, AI-Mosawi AA (2016) Aortic root calcifications: a possible imaging biomarker of coronary atherosclerosis. Pulse 3:167–171
Pawade T, Sheth T, Guzzetti E, Dweck MR, Clavel M (2019) Why and how to measure aortic valve calcification in patients with aortic stenosis. JACC Cardiovasc Imaging 12:1835–1848
Okada H, Tada H, Hayashi K, Kawashima H, Takata T, Sakata K, Nohara A, Mabuchi H, Yamagishi M, Kawashiri M (2018) Aortic root calcification score as an independent factor for predicting major adverse cardiac events in familial hypercholesterolemia. J Atheroscler Thromb 25:634–642
Nakao YM, Miyamoto Y, Higashi M, Noguchi T, Ohnishi M, Kubota I, Tsutsui H, Kawasaki T, Furukawa Y, Yoshimura M, Morita H, Nishimura K, Kada A, Goto Y, Okamura T, Tei C, Tomoike H, Naito H, Yasuda S (2018) Sex difference in impact of coronary artery calcification to predict coronary artery disease. Heart 104:1118–1124
Vandvik PO, Lincoff AM, Gore JM, Gutterman DD, Sonnenberg FA, Alonso-Coello P, Akl EA, Lansberg MG, Guyatt GH, Spencer FA (2012) Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 141(2 Suppl):e637S-e668S
Han D, Cordoso R, Whelton S, Rozanski A, Budoff MJ, Miedema MD, Nasir K, Shaw LJ, Rumberger JA, Gransar H, Dardari Z, Blumenthal RS, Blaha MJ, Berman DS (2021) Prognostic significance of aortic valve calcium in relation to coronary artery calcification for long-term, cause-specific mortality: results from the CAC consortium. Eur Heart J Cardiovasc Imaging 22:1257–1263
Kälsch H, Lehmann N, Mahabadi AA, Bauer M, Kara K, Huppe P, Moebus S, Mohlenkamp S, Dragano N, Schmermund A, Stang A, Jockel K, Erbel R, Investigators Group of the Heinz Nixdorf Recall Study (2014) Beyond Framingham risk factors and coronary calcification: does aortic valve calcification improve risk prediction? The Heinz Nixdorf Recall study. Heart 100:930–937
Lindroos M, Kupari M, Valvanne J, Strandberg T, Heikkilä J, Tilvis R (1994) Factors associated with calcific aortic valve degeneration in the elderly. Eur Heart J 15:865–870
Gradman AH (1979) Rapid progression in valvular aortic stenosis. Chest 76:376–377
Freeman RV, Otto CM (2005) Spectrum of calcific aortic valve disease: pathogenesis, disease progression and treatment strategies. Circulation 111:3316–3326
Nassimiha D, Aronow WS, Ahn C, Goldman ME (2001) Rate of progression of valvular aortic stenosis in patients > or = 60 years of age. Am J Cardiol 87:807–809
Henein M, Hallgren P, Holmgren A, Sorensen K, Ibrahimi P, Kofoed KF, Larsen LH, Hassager C (2015) Aortic root, not valve, calcification correlated with coronary artery calcification in patients with severe aortic stenosis: a two-center study. Atherosclerosis 243:631–637
Nafakhi H, Al-Nafakh HA, AI-Mosawi AA, Graty FA (2015) Correlation between aortic root calcification and coronary artery atherosclerotic markers assessed using multidetector computed tomography. Acad Radiol 22:357–362
Tastet L, Enriquez-Sarano M, Capoulade R, Makouf J, Araoz PA, Shen M, Michelena HI, Larose E, Arsenault M, Bedard E, Pibatot P, Clavel M (2017) Impact of aortic valve calcification and sex on hemodynamic progression and clinical outcomes in AS. J Am Coll Cardiol 69:2096–2098
Clavel MA, Pibarot P, Messika-Zeitoun D, Capoulade R, Malouf J, Aggarval S, Araoz PA, Michelena HI, Cueff C, Larose E, Miller JD, Vahanian A, Enriquez-Sarano M (2014) Impact of aortic valve calcification, as measured by MDCT, on survival in patients with aortic stenosis: results of international registry study. J Am Coll Cardiol 64:1202–1213
Jeon DS, Atar S, Brasch AV, Luo H, Mirocha J, Naqvi TZ, Kraus R, Berman DS, Siegel RJ (2001) Association of mitral annulus calcification, aortic valve sclerosis and aortic root calcification with abnormal myocardial perfusion single photon emission tomography in subjects age ≤ 65 years old. J Am Coll Cardiol 38:1988–1993
Summerhill VI, Moschetta D, Orekhov AN, Poggio P, Myasoedova VA (2020) Sex-specific features of calcific aortic valve disease. Int J Mol Sci 21(16):5620
Pressman GS, Crudu V, Parameswaran-Chandrika A, Romero-Corral A, Purushottam B, Figueredo VM (2011) Can total cardiac calcium predict the coronary calcium score? Int J Cardiol 146:202–206
Zhang B, Miller VM, Miller JD (2019) Influences of sex and estrogen in arterial and valvular calcification. Front Endocrinol (Lausanne) 10:622
Simon LR, Scott AJ, Figueroa Rios L, Zembles J, Masters KS (2022) Cellular-scale sex differences in extracellular matrix remodeling by valvular interstitial cells. Heart Vessels. https://doi.org/10.1007/s00380-022-02164-2
Yamamoto H, Kihara Y, Kitagawa T, Ohashi N, Kunita E, Iwanaga Y, Kobuke K, Miyazaki S, Kawasaki T, Fujimoto S, Daida H, Fujii T, Sato A, Okimoto T, Kuribayashi S, Investigators PREDICT (2018) Coronary plaque characteristics in computed tomography and 2-year outcomes: the PREDICT study. J Cardiovasc Comput Tomogr 12:436–443
Joseph J, Naqvi SY, Giri J, Goldberg S (2017) Aortic stenosis: pathophysiology. Diagn Ther Am J Med 130:253–263
Pawade T, Clavel MA, Tribouilloy C, Dreyfus J, Mathieu T, Tastet L, Renard C, Gun M, Jenkins WSA, Macron L, Sechrist JW, Lacomis JM, Nguyen V, Galian Gay L, Cuéllar Calabria H, Ntalas I, Cartlidge TRG, Prendergast B, Rajani R, Evangelista A, Cavalcante JL, Newby DE, Pibarot P, Messika Zeitoun D, Dweck MR (2018) Computed tomography aortic valve calcium scoring in patients with aortic stenosis. Circ Cardiovasc Imaging 11:e007146
Veulemans V, Piayda K, Maier O, Bosbach G, Polzin A, Hellhammer K, Afzal S, Klein K, Dannenberg L, Zako S, Jung C, Westenfeld R, Kelm M, Zeus T (2021) Aortic valve calcification is subject to aortic stenosis severity and the underlying flow pattern. Heart Vessels 36:242–251
Owens DS, Katz R, Takasu J, Kronmal R, Budoff MJ, O’Brien KD (2010) Incidence and progression of aortic valve calcium in the Multi-ethnic Study of Atherosclerosis (MESA). Am J Cardiol 105:701–708
Shaikh K, Nakanishi R, Kim N, Budoff MJ (2019) Coronary artery calcification and ethnicity. J Cardiovasc Comput Tomogr 13:353–359
Acknowledgements
We would like to thank Drs. Masanao Naya (Hokkaido University Hospital, Sapporo, Japan), Masafumi Watanabe (Yamagata University Hospital, Yamagata, Japan), Tetsu Watanabe (Yamagata University Hospital, Yamagata, Japan), Satoshi Yasuda (Tohoku University Hospital, Sendai, Japan), Michihiro Yoshimura (Jikei University School of Medicine, Tokyo, Japan), Makoto Kawai (Jikei University School of Medicine, Tokyo, Japan), Tomonori Okamura (Keio University School of Meidicine, Tokyo, Japan), Hiroaki Naito (Nissei Hospital, Osaka, Japan), Masahiro Higashi (National Hospital Organization Osaka National Hospital, Osaka Japan), Hideaki Morita (Osaka medical College, Takatsuki, Japan), Kunihiro Nishimura (National Cerebral and Cardiovascular center, Suita, Japan), Yoko Nakao (National Cerebral and Cardiovascular Center, Suita, Japan), Yasuhide Asaumi (National Cerebral and Cardiovascular Center, Suita, Japan), Hiroyuki Miura (National Cerebral and Cardiovascular Center, Suita, Japan), Yutaka Furukawa (Kobe City Medical Center General Hospital, Kobe, Japan), Hiroyuki Tsutsui (Kyusyu University Hospital, Fukuoka, Japan), Tomohiro Kawasaki (Shin Koga Hospital, Kurume, Japan), Mitsuru Oishi (Kagoshima University Hospital, Kagoshima, Japan), Masaaki Miyata (Kagoshima University Hospital, Kagoshima Japan), Hitonobu Tomoike (NTT Research, Inc. MEI Lab, Tokyo, Japan), Junko Masue (National Cerebral and Cardiovascular Center, Suita, Japan), Yoko Sumita (National Cerebral and Cardiovascular Center, Suita, Japan), and Yusuke Sasahara (National Cerebral and Cardiovascular Center, Suita, Japan) for supporting NADESICO Study.
Funding
This research was supported by Japan Agency for Medical Research and Development under Grant Number 20gk0210026h001.
Author information
Authors and Affiliations
Contributions
Study concept and design: SW, YI, and TN; data curation: SW and MN; analysis and interpretation of data: SW, MN, and YI; interpretation of results: YM and TN; supervision: YM and TN; writing–original draft: SW; writing–reviewing and editing: YI.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wada, S., Iwanaga, Y., Nakai, M. et al. Aortic valve and aortic root calcifications for predicting major adverse cardiovascular events: NADESICO study. Heart Vessels 38, 562–569 (2023). https://doi.org/10.1007/s00380-022-02187-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02187-9