Abstract
The therapeutic effects of reperfusion strategies with complete revascularization (CR) or incomplete revascularization (IR) in non-ST segment myocardial infarction (NSTEMI) patients with multivessel disease (MVD) are controversial. In such patients, whether utilization of different generations of drug-eluting stents (DES) for IR or CR affect long-term major adverse cardiovascular events (MACE) is unknown. This study included 702 NSTEMI patients with MVD who received first-generation (1G) or second-generation (2G) DES. In multivariable analysis, chronic kidney disease, chronic total, 1G DES and IR were independent predictors of long-term MACE. In patients receiving 1G DES, no significant differences of MACE were observed between the IR and CR groups (39.1% vs. 36.2%, p = 0.854). However, in patients receiving 2G DES, significantly fewer MACE were observed in the CR group than in the IR group (3.7% vs. 10.2%, p = 0.002). Compared with patients receiving 1G DES for IR, those receiving 2G DES for IR and CR exhibited significantly lower risk of MACE (59% and 83% lower, respectively). CR could not provide clinical benefits over IR in NSTEMI patients with MVD receiving 1G DES. However, in patients receiving 2G DES, compared with IR, CR was associated with a lower risk of long-term MACE, which was mainly caused by low rates of non-TLR and any revascularization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multivessel disease (MVD) is present in about half of patients with non-ST segment elevation myocardial infarction (NSTEMI) [1]. According to clinical guidelines, coronary artery bypass grafting (CABG) is recommended for coronary revascularization in MVD [2, 3]. However, patients with NSTEMI often present with high-risk factors for surgery such as old age and left ventricular dysfunction. Moreover, with advancements in techniques and designs of devices for percutaneous coronary intervention (PCI), the proportion of NSTEMI patients with MVD undergoing PCI has increased in the recent years, whereas the proportion of such patients undergoing CABG has decreased [4]. The main advantage of CABG over PCI is extensive revascularization [5]. Therefore, in NSTEMI patients with MVD undergoing PCI, it is reasonable to pursue complete revascularization (CR) rather than culprit-only or incomplete revascularization (IR).
However, randomized studies addressing optimal PCI reperfusion strategies (CR or IR) in NSTEMI patients with MVD are scant. Some observational studies have concluded that CR yields more favorable clinical outcomes than IR; however, some studies have not obtained such a finding [6,7,8,9,10,11]. Kim et al. showed that NSTEMI patients with MVD receiving CR have significantly lower risk of death, myocardial infarction (MI), and non-target lesion revascularization (non-TLR) than those receiving IR [8]. However, a recent meta-analysis demonstrated that in NSTEMI patients with MVD, routine multivessel CR did not appear to provide a clinical benefit over culprit-only IR [12]. In most related studies, bare-metal stent (BMS) or first-generation (1G) drug-eluting stent (DES) has been used for analysis. However, it is well known that second-generation (2G) DES, which possesses new metal and polymer designs, yields more favorable clinical outcomes than do BMS and 1G DES [13,14,15]. Therefore, in this study, we analyzed the long-term clinical outcomes of different generations of DES (1G and 2G) and reperfusion strategies (IR and CR) in NSTEMI patients with MVD.
Materials and methods
Study population
This study analyzed NSTEMI patients with MVD who underwent DES implantations between April 2005 and April 2016 from the Cardiovascular Atherosclerosis and Percutaneous TrAnsluminal INterventions (CAPTAIN) registry. The inclusion criteria for stenting were as follows: evidence of myocardial ischemia or infarction and > 50% stenosis in a native coronary artery suitable for stenting. The exclusion criteria were as follows: STEMI, receipt of BMS for revascularization, receipt of mixed 1G and 2G DES, MVD patients who received bypass surgery, intolerance to dual antiplatelet therapy, and inability to follow the study protocol. Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor (clopidogrel or ticagrelor) was administered to all enrolled patients for at least 9 months. Ethical approval for this study was obtained from the Institutional Review Board of Chang Gung Medical Foundation. In addition to providing consent to publish case details, all patients provided informed consent to undergo PCI and the follow-up protocol.
Interventional procedures, definitions, and clinical follow-up
All stent implantations were performed using the radial or femoral artery approach according to standard techniques. For lesions with very narrow diameters (> 70% stenosis), predilations were performed using undersized balloons. Selection of stent type was left to the operator’s discretion and primarily based on available stent sizes. The 1G DESs used in the present study are outlined as follows: Cypher (Johnson and Johnson, Warren, NJ, USA) or TAXUS (Boston Scientific, Natick, MA, USA). The 2G DESs used in the present study were Promus (Boston Scientific, Natick, MA, USA), Endeavor and Resolute (Medtronic, Minneapolis, MD, USA), Xience (Abbott Vascular, Santa Clara, CA, USA), Biomatrix (Biosensor, Singapore), and Nobori (TERUMO, Tokyo, Japan). A review of medical records was conducted to obtain information on clinical status, medical management, and occurrence of any adverse event for all patients. The patients were clinically followed up through outpatient visits or telephone contact; follow-up was scheduled at 1, 2, 3, 6, 9, and 12 months after the procedure and every 3 months thereafter.
Angiographic MVD was defined as the presence of ≥ 50% stenosis in at least two major coronary vessels or their major branches. Angiographic CR was defined as ≥ 50% stenosis in a segment of at least 2.25-mm diameter that was successfully treated during index hospitalization or staged electively within 30 days after discharge from index hospitalization. To define CR, the cutoff value of the segment diameter was determined based on the smallest diameter of the currently available DESs. Long-term major adverse cardiovascular events (MACE) during follow-up included cardiac death, recurrent MI, and any revascularization, including TLR and non-TLR. Recurrent MI was diagnosed if a patient experienced prolonged chest pain for more than 30 min, ST segment elevation or depression of at least 0.2 mV in at least two contiguous electrocardiogram leads, and significantly elevated levels of cardiac enzymes.
Statistical analysis
All results are presented as means ± standard deviations or percentages, and categorical data are presented as numbers. The normality of all variables was analyzed. For continuous data, the groups were compared using a t test or Wilcoxon rank-sum test based on the distribution. Categorical variables were compared using the Chi-squared test. A multivariable logistic regression model was used to identify the independent predictors of MACE. Survival curves for all groups were generated and compared using an adjusted Cox regression model. All statistical analyses were performed using SPSS 17.0 for Windows.
Results
Baseline characteristics
A total of 702 NSTEMI patients with MVD receiving either 1G or 2G DES were enrolled in this study. The baseline characteristics of the study population are shown in Table 1. The mean age was 64.2 ± 11.8 years. Moreover, 77.2% of the patients were men, 40.2% had diabetes mellitus (DM), 20.4% had chronic kidney disease (CKD), 49.1% had triple-vessel disease, and 10.5% had chronic total occlusion (CTO) lesions; 575 (82%) patients received 2G DES and 358 (51%) patients achieved CR. The patients were divided into IR and CR groups; for almost all clinical characteristics, no significant differences were observed between the IR and CR groups, except that the IR group had a lower left ventricular ejection fraction (LVEF) and more cases of CKD and triple-vessel disease than did the CR group.
Independent predictors of MACE
The multivariable logistic regression model revealed that the following 19 potential covariates were independent predictors of long-term outcomes: age > 65 years, sex, hypertension, DM, smoking, dyslipidemia, family history of coronary artery disease (CAD), CKD, previous MI, previous stroke, triple- versus two-vessel CAD, cardiogenic shock, LVEF < 40%, 1G DES versus 2G DES, IR versus CR, a calcified lesion, a bifurcation lesion, an ostial lesion, and a CTO lesion. The independent prognostic predictors of long-term MACE were CKD [Odds ratio (OR): 2.48; 95% confidence interval (CI): 1.59–3.88; p < 0.001], CTO (OR 1.91; 95% CI 1.01–3.60; p = 0.048), 1G DES (OR 3.35; 95% CI 2.14–5.24; p < 0.001), and IR (OR 1.75; 95% CI 1.10–2.79; p = 0.019) (Table 2).
Subgroup analysis stratified based on clinical characteristics
As shown in Table 3, all patients receiving 1G or 2G DES were further divided into four subgroups: IR combined with 1G DES (n = 69), CR combined with 1G DES (n = 58), IR combined with 2G DES (n = 275), and CR combined with 2G DES (n = 300). The IR and CR subgroups receiving 1G DES did not differ significantly in terms of age, sex, DM, hypertension, dyslipidemia, smoking, family history of CAD, previous MI, previous stroke, CKD, cardiogenic shock, LVEF, a calcified lesion, an ostial lesion, a bifurcation lesion, a CTO lesion or DAPT. More patients in the IR combined with 1G DES subgroup had triple-vessel disease (68.1% vs. 32.8%, p < 0.001) than in the CR combined with 1G DES subgroup. The IR and CR subgroups receiving 2G DES did not differ significantly in terms of age, sex, DM, hypertension, dyslipidemia, smoking, family history of CAD, previous MI, previous stroke, a calcified lesion, an ostial lesion, a bifurcation lesion, a CTO lesion or DAPT. More patients in the IR combined with 2G DES subgroup had CKD (25.8% vs. 15.0%, p = 0.002), cardiogenic shock (5.5% vs. 1.7%, p = 0.021), triple-vessel disease (61.1% vs. 37.0%, p < 0.001), and decreased LVEF (58.8 ± 12.5% vs. 61.1 ± 11.4%, p = 0.035) than in the CR combined with 2G DES subgroup.
Long-term outcomes
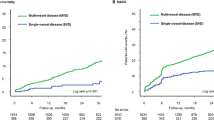
During a follow-up period of 37 ± 31 months, 87 (12.4%) patients experienced MACE. In general, patients receiving 2G DES had lower rates of MACE (6.8% vs. 37.8%, p < 0.001), cardiac death (1.7% vs. 15%, p < 0.001), recurrent MI (1.0% vs. 11.0%, p < 0.001), any revascularization (5.2% vs. 19.7%, p < 0.001), non-TLR (3.1% vs. 8.7%, p = 0.011), and TLR (2.8% vs. 13.4%, p < 0.001) than those receiving 1G DES. The clinical outcomes of the four subgroups are shown in Fig. 1. In patients receiving 1G DES, the long-term risk of TLR was significantly higher in the CR group than in the IR group (20.2% vs. 7.2%, p = 0.036), and no significant differences were observed for non-TLR (11.6% vs. 5.2%, p = 0.226), any revascularization (18.8% vs. 20.7%, p = 0.826), recurrent MI (13% vs. 8.6%, p = 0.572), cardiac death (18.8% vs. 10.3%, p = 0.218), or total MACE (39.1% vs. 36.2%, p = 0.854) between the IR and CR subgroups. In patients receiving 2G DES, no significant differences were observed for TLR (3.3% vs. 2.3%, p = 0.614), recurrent MI (1.1% vs. 1%, p = 1.000), or cardiac death (2.5% vs. 1%, p = 0.206) between the IR and CR subgroups. However, the patients receiving 2G DES in the CR subgroup had more favorable outcomes for non-TLR (0.7% vs. 5.8%, p < 0.001) and any revascularization (2.7% vs. 8.0%, p = 0.005) than those in the IR subgroup; this translated to a lower rate of total MACE (3.7% vs. 10.2%, p = 0.002) in patients receiving 2G DES in the CR subgroup than in those receiving 2G DES in the IR subgroup.
Clinical events of four subgroups: a IR with 1G DES, b CR with 1G DES, c IR with 2G DES, and d CR with 2G DES; clinical events between subgroups were compared (*p < 0.05). 1G first generation, 2G second generation, CR complete revascularization, CV cardiovascular, DES drug-eluting stent, IR incomplete revascularization, MACE major adverse cardiovascular events, MI myocardial infarction, TLR target lesion revascularization
As shown in Fig. 2, to eliminate the confounding effects of clinical covariates in the four subgroups, potential clinical covariates, namely age > 65 years, sex, hypertension, DM, smoking, dyslipidemia, family history of CAD, previous MI, previous stroke, CKD, cardiogenic shock, and triple-vessel disease, LVEF < 40%, a calcified lesion, a bifurcation lesion, an ostial lesion, and a CTO lesion, were adjusted for in the Cox regression model. After adjustment, compared with the IR combined with 1G DES subgroup (HR: 1.00), the CR combined with 1G DES subgroup did not exhibit a significantly reduced risk of MACE (HR: 0.95, 95% CI 0.54–1.69; p = 0.869); however, the IR combined with 2G DES subgroup (59%; HR: 0.41, 95% CI 0.24–0.71; p = 0.001) and CR combined with 2G DES subgroup (83%; HR: 0.17, 95% CI 0.08–0.35; p < 0.001) had significantly reduced risks of MACE.
Survival curves for NSTEMI patients with MVD from a Cox proportional hazard model for four subgroups. 1G first generation, 2G second generation, CR complete revascularization, DES drug-eluting stent, HR hazard ratio, IR incomplete revascularization, MVD multivessel disease, NSTEMI non-ST segment elevation myocardial infarction
Discussion
The major findings of this study are as follows: (1) NSTEMI patients with MVD receiving 2G DES for revascularization had more favorable long-term outcomes than did those receiving 1G DES for revascularization. (2) In NSTEMI patients with MVD receiving 1G DES for revascularization, CR did not result in significantly better clinical outcomes than did IR after long-term follow-up. (3) In NSTEMI, patients receiving 2G DES, CR was associated with a lower risk of long-term non-TLR, any revascularization, and MACE than was IR. To the best of our knowledge, this was the first study to compare 1G and 2G DES implantation in NSTEMI patients with MVD. In addition, the current study had a longer follow-up period than those in previous related studies, and thus the clinical outcomes of 2G DES for CR were verified.
It is known that compared with 2G DES treatment, 1G DES treatment has unfavorable outcomes such as late stent thrombosis, in-stent restenosis, and late catch up, particularly in patients with acute coronary syndrome, complex lesions, and diabetes and elderly patients [16,17,18,19]. One study showed that over a 10-year follow-up, the annual MACE rate in patients receiving 1G DES was consistent and did not decrease over time as has been observed in patients receiving 2G DES [20, 21]. A recent optical coherence tomography study showed that compared with patients receiving 2G DES, those receiving 1G DES had a longer lipid length, larger lipid arc, greater prevalence of the 360° lipid arc, and thinner fibrous cap, resulting in more unstable neoatherosclerosis over time [22]. These results have been confirmed by previous reports that 1G DES use is associated with greater atherosclerosis progression than is 2G DES use after long-term follow-up [16,17,18,19]. Therefore, in NSTEMI patients with MVD, the clinical efficacy of 2G DES is better than that of 1G DES in terms of TLR, non-TLR, recurrent MI, cardiovascular death, and MACE.
Most studies addressing the issue of CR and IR in NSTEMI patients with MVD are observational studies, and most of their follow-up durations are approximately 1 year [6,7,8,9,10,11]. Hassanin et al. utilized the Acute Catheterisation and Urgent Intervention Triage StrategY (ACUITY) randomized study database to analyze the outcomes of 2255 patients with MVD who underwent single-vessel PCI (IR) and 609 patients who underwent MV PCI (CR) in the setting of NSTEMI [11]. Compared with IR, a negative benefit of CR was found. In the ACUITY trial, selection of stent type was dependent on the operator’s choice, and 65% of the patients received DES [23]. Because the ACUITY trial was performed from August 2003 to December 2005, it is reasonable to speculate that BMS or 1G DES was used. To achieve CR, patients may receive more and longer stent implantation. Theoretically, patients receiving CR have a higher risk of TLR than those receiving IR because the stents used in angioplasty are associated with a high event rate. The findings of the current study proved this hypothesis and showed that patients who received 1G DES had a significantly higher risk of TLR in those who achieved CR than those who achieved IR (20.2% vs. 7.2%, p = 0.036) after more than 3 years of follow-up. However, because of the progression of residual coronary lesions, patients with IR have a higher risk of non-TLR than do those with CR; therefore, use of old generations of stents may result in a higher TLR rate, which would negate the benefits of CR. This may explain why CR did not have clear clinical benefits over IR in Hassanin’s post hoc analysis [11].
The clinical efficacy of different generations of DES applied for different reperfusion strategies (CR or IR) has not been discussed in detail in previous studies. Kim et al. conducted a nationwide registry-based study of patients who received mixed BMS, 1G DES, and 2G DES from November 2005 to January 2008. The researchers only reported that DES was used in more than 90% of the patients and that CR could reduce the occurrences of non-TLR, recurrent MI, death, and MACE after 1-year of follow-up [8]. Lee et al. conducted a single-center observational study of patients who received both 1G and 2G DES from April 2003 to December 2006 and compared the clinical outcomes of IR and CR in NSTEMI patients with MVD during a median follow-up of 36 months [9]. The researchers reported that the CR group had lower 1G DES use than did the IR group (76% vs. 92.5%, p = 0.01) and found that the CR group had a lower incidence of revascularization after a 3-year follow-up period than did the IR group. The present study had a long (mean) follow-up period of 37 ± 31 months, and the results demonstrated that 2G DES, with a more effective stent design, used in both the IR and CR groups resulted in very low incidences of TLR; no significant difference was observed between the two groups (3.3% vs. 2.3%, p = 0.614). However, because of the progression of residual coronary lesions, patients receiving 2G DES in the IR group had a higher risk of non-TLR than did those in the CR group (5.8% vs. 0.7%, p < 0.001); therefore, patients receiving 2G DES in the CR group had a lower risk of stent-related TLR and fewer residual lesions with lower non-TLR, which translated to lower risks of any revascularization (2.7% vs. 8.0%, p = 0.005) and MACE (3.7% vs. 10.2%, p = 0.002) in these patients than in those receiving 2G DES in the IR group.
This prospective observational study had several limitations. First, the definition of CR in this study was determined based on anatomic criteria instead of functional criteria (such as fractional flow reserve). Second, DAPT with aspirin and a P2Y12 inhibitor has been the standard therapy for acute coronary syndrome. Using new generation of P2Y12 inhibitors such as ticagrelor or prasugrel had more favorable clinical outcomes than clopidogrel for acute coronary syndrome patients in clinical trials [24, 25]. However, in our hospital, ticagrelor launched since April 2014 and prasugrel is not yet available. Therefore, DAPT with aspirin and clopidogrel was used in most patients in this study. In addition, no data risk factor control, and patient compliance were available; these may have influenced the present results. Third, this study used a real-world registry. Although adjustment for confounding factors was performed, confounding effects may have resulted in bias in the study results. Additional large, prospective, randomized trials are warranted to confirm the benefits of CR in similar clinical settings.
Conclusions
CR could not provide clinical benefits over IR in NSTEMI patients with MVD receiving 1G DES. In patients receiving 2G DES, compared with IR, CR was associated with a lower risk of long-term MACE, which was mainly caused by low rates of non-TLR and any revascularization.
References
Breeman A, Mercado N, Lenzen M, van den Brand MM, Harrington RA, Califf RM, Topol EJ, Simoons ML, Boersma E, Investigators P (2002) Characteristics, treatment and outcome of patients with non-ST-elevation acute coronary syndromes and multivessel coronary artery disease: observations from PURSUIT (platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrelin therapy). Cardiology 98:195–201
Authors/Task Force m, Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, Filippatos G, Hamm C, Head SJ, Juni P, Kappetein AP, Kastrati A, Knuuti J, Landmesser U, Laufer G, Neumann FJ, Richter DJ, Schauerte P, Sousa Uva M, Stefanini GG, Taggart DP, Torracca L, Valgimigli M, Wijns W, Witkowski A (2014) 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 35:2541–2619
Fihn SD, Blankenship JC, Alexander KP, Bittl JA, Byrne JG, Fletcher BJ, Fonarow GC, Lange RA, Levine GN, Maddox TM, Naidu SS, Ohman EM, Smith PK (2014) 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 64:1929–1949
Pandey A, McGuire DK, de Lemos JA, Das SR, Berry JD, Brilakis ES, Banerjee S, Marso SP, Barsness GW, Simon DN, Roe M, Goyal A, Kosiborod M, Amsterdam EA, Kumbhani DJ (2016) Revascularization trends in patients with diabetes mellitus and multivessel coronary artery disease presenting with non-ST elevation myocardial infarction: insights from the national cardiovascular data registry acute coronary treatment and intervention outcomes network registry-get with the guidelines (NCDR ACTION Registry-GWTG). Circ Cardiovasc Qual Outcomes 9:197–205
Ahn JM, Park DW, Lee CW, Chang M, Cavalcante R, Sotomi Y, Onuma Y, Tenekecioglu E, Han M, Lee PH, Kang SJ, Lee SW, Kim YH, Park SW, Serruys PW, Park SJ (2017) Comparison of stenting versus bypass surgery according to the completeness of revascularization in severe coronary artery disease: patient-level pooled analysis of the SYNTAX, PRECOMBAT, and BEST trials. JACC Cardiovasc Interv 10:1415–1424
Brener SJ, Murphy SA, Gibson CM, DiBattiste PM, Demopoulos LA, Cannon CP, Aggrastat T-TITAw, Determine Cost of Therapy with an Invasive or Conservative Strategy-Thrombosis in Myocardial I (2002) Efficacy and safety of multivessel percutaneous revascularization and tirofiban therapy in patients with acute coronary syndromes. Am J Cardiol 90:631–633
Palmer ND, Causer JP, Ramsdale DR, Perry RA (2004) Effect of completeness of revascularization on clinical outcome in patients with multivessel disease presenting with unstable angina who undergo percutaneous coronary intervention. J Invasive Cardiol 16:185–188
Kim MC, Jeong MH, Ahn Y, Kim JH, Chae SC, Kim YJ, Hur SH, Seong IW, Hong TJ, Choi DH, Cho MC, Kim CJ, Seung KB, Chung WS, Jang YS, Cho SY, Rha SW, Bae JH, Cho JG, Park SJ, Korea Acute Myocardial Infarction Registry I (2011) What is optimal revascularization strategy in patients with multivessel coronary artery disease in non-ST-elevation myocardial infarction? Multivessel or culprit-only revascularization. Int J Cardiol 153:148–153
Lee HJ, Song YB, Hahn JY, Kim SM, Yang JH, Choi JH, Choi SH, Choi JH, Lee SH, Gwon HC (2011) Multivessel vs single-vessel revascularization in patients with non-ST-segment elevation acute coronary syndrome and multivessel disease in the drug-eluting stent era. Clin Cardiol 34:160–165
Onuma Y, Muramatsu T, Girasis C, Kukreja N, Garcia-Garcia HM, Daemen J, Gonzalo N, Piazza N, Einthoven J, van Domburg R, Serruys PW, Interventional cardiologists of the T (2013) Single-vessel or multivessel PCI in patients with multivessel disease presenting with non-ST-elevation acute coronary syndromes. EuroIntervention 9:916–922
Hassanin A, Brener SJ, Lansky AJ, Xu K, Stone GW (2015) Prognostic impact of multivessel versus culprit vessel only percutaneous intervention for patients with multivessel coronary artery disease presenting with acute coronary syndrome. EuroIntervention 11:293–300
Mariani J, Macchia A, De Abreu M, Gonzalez Villa Monte G, Tajer C (2016) Multivessel versus single vessel angioplasty in non-ST elevation acute coronary syndromes: a systematic review and metaanalysis. PLoS One 11:e0148756
De Luca G, Smits P, Hofma SH, Di Lorenzo E, Vlachojannis GJ, Van’t Hof AWJ, van Boven AJ, Kedhi E, Stone GW, Suryapranata H, Drug-Eluting Stent in Primary Angioplasty c (2017) Everolimus eluting stent vs first generation drug-eluting stent in primary angioplasty: a pooled patient-level meta-analysis of randomized trials. Int J Cardiol 244:121–127
Stone GW, Midei M, Newman W, Sanz M, Hermiller JB, Williams J, Farhat N, Caputo R, Xenopoulos N, Applegate R, Gordon P, White RM, Sudhir K, Cutlip DE, Petersen JL, Investigators SI (2009) Randomized comparison of everolimus-eluting and paclitaxel-eluting stents: two-year clinical follow-up from the Clinical Evaluation of the Xience V Everolimus Eluting Coronary Stent System in the Treatment of Patients with de novo Native Coronary Artery Lesions (SPIRIT) III trial. Circulation 119:680–686
Varenhorst C, Lindholm M, Sarno G, Olivecrona G, Jensen U, Nilsson J, Carlsson J, James S, Lagerqvist B (2018) Stent thrombosis rates the first year and beyond with new- and old-generation drug-eluting stents compared to bare metal stents. Clin Res Cardiol 107(9):816–823
Rodriguez AE, Santaera O, Larribau M, Sarmiento R, Haiek C, Del Pozo JF, Pavlovsky H, Rodriguez-Granillo AM, Investigators EI (2017) Second vs. first-generation drug-eluting stents in complex lesions subsets: 3 years’ follow-up of ERACI IV study. Miner Cardioangiol 65:81–90
Wanha W, Kawecki D, Roleder T, Morawiec B, Gladysz S, Kowalowka A, Jadczyk T, Adamus B, Pawlowski T, Smolka G, Kazmierski M, Ochala A, Nowalany-Kozielska E, Wojakowski W (2017) Second-generation drug-eluting stents in the elderly patients with acute coronary syndrome: the in-hospital and 12-month follow-up of the all-comer registry. Aging Clin Exp Res 29:885–893
Kawecki D, Morawiec B, Dola J, Wanha W, Smolka G, Pluta A, Marcinkiewicz K, Ochala A, Nowalany-Kozielska E, Wojakowski W (2016) First- versus second-generation drug-eluting stents in acute coronary syndromes (Katowice-Zabrze registry). Arq Bras Cardiol 106:373–381
Kawecki D, Morawiec B, Dola J, Wanha W, Smolka G, Pluta A, Marcinkiewicz K, Ochala A, Nowalany-Kozielska E, Wojakowski W (2015) Comparison of first- and second-generation drug-eluting stents in an all-comer population of patients with diabetes mellitus (from Katowice-Zabrze registry). Med Sci Monit 21:3261–3269
Galloe AM, Kelbaek H, Thuesen L, Hansen HS, Ravkilde J, Hansen PR, Christiansen EH, Abildgaard U, Stephansen G, Lassen JF, Engstrom T, Jensen JS, Jeppesen JL, Bligaard N, Investigators SOI (2017) 10-Year clinical outcome after randomization to treatment by sirolimus- or paclitaxel-eluting coronary stents. J Am Coll Cardiol 69:616–624
Jensen LO, Thayssen P, Christiansen EH, Maeng M, Ravkilde J, Hansen KN, Hansen HS, Krusell L, Kaltoft A, Tilsted HH, Berencsi K, Junker A, Lassen JF, Investigators SOI (2016) Safety and efficacy of everolimus- versus sirolimus-eluting stents: 5-year results from SORT OUT IV. J Am Coll Cardiol 67:751–762
Kobayashi N, Ito Y, Yamawaki M, Araki M, Sakai T, Obokata M, Sakamoto Y, Mori S, Tsutsumi M, Nauchi M, Honda Y, Tokuda T, Makino K, Shirai S, Hirano K (2018) Differences between first-generation and second-generation drug-eluting stent regarding in-stent neoatherosclerosis characteristics: an optical coherence tomography analysis. Int J Cardiovasc Imaging. https://doi.org/10.1007/s10554-018-1375-4
Stone GW, McLaurin BT, Cox DA, Bertrand ME, Lincoff AM, Moses JW, White HD, Pocock SJ, Ware JH, Feit F, Colombo A, Aylward PE, Cequier AR, Darius H, Desmet W, Ebrahimi R, Hamon M, Rasmussen LH, Rupprecht HJ, Hoekstra J, Mehran R, Ohman EM, Investigators A (2006) Bivalirudin for patients with acute coronary syndromes. N Engl J Med 355:2203–2216
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM, Investigators T-T (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, Horrow J, Husted S, James S, Katus H, Mahaffey KW, Scirica BM, Skene A, Steg PG, Storey RF, Harrington RA, Freij A, Thorsen M, Investigators P (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057
Acknowledgements
This work was supported by Chang Gung Medical Foundation, Grant no. CORPG 3C0162 & 3G0281.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Hsieh, MJ., Chen, CC., Lee, CH. et al. Complete and incomplete revascularization in non-ST segment myocardial infarction with multivessel disease: long-term outcomes of first- and second-generation drug-eluting stents. Heart Vessels 34, 251–258 (2019). https://doi.org/10.1007/s00380-018-1252-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1252-z