Abstract
Although measurement of right ventricular ejection fraction (RVEF) may be relevant for evaluation of therapeutic efficacy and/or prognosis in patients with pulmonary hypertension, RVEF obtained by echocardiography has limited accuracy. In contrast, radionuclide and/or magnetic resonance imaging can measure RVEF more reliably. In this study, we investigated the relationship between RVEF measured by radionuclide angiography and the echocardiographic parameters that are recommended by the American Society of Echocardiography as representative of right heart function. There were 23 study participants with pulmonary hypertension who underwent radionuclide angiography and 2-dimensional and Doppler echocardiography (n = 30 measurements). RVEF measured by radionuclide angiography correlated with right ventricular Tei index (RV Tei index) measured by Doppler echocardiography (r = −0.601, P < 0.0005). Receiver operating characteristic curve analysis showed that an RV Tei index cut-off value of 0.371 was the best of predictor of RVEF ≤35% (area under the curve = 0.768, sensitivity = 0.857, selectivity = 0.667). Multiple regression analysis showed that RVEF was correlated with the RV Tei index, and this association was independent of other echocardiographic right ventricular function parameters (r = −0.644, P < 0.005). The RV Tei index measured by Doppler echocardiography may be an acceptable surrogate marker of RVEF in patients with pulmonary hypertension.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular ejection fraction (LVEF), which is simply and accurately measured by 2-dimensional (2D) echocardiogram, is a powerful parameter to evaluate left ventricular function. However, right ventricular ejection fraction (RVEF) is difficult to assess by 2D echocardiography because of the unique morphology of the right ventricle. Radionuclide angiography, magnetic resonance imaging (MRI), and 3-dimensional echocardiography may be useful modalities for assessing RVEF, and radionuclide angiography has been shown to be the most reliable method [1, 2]. The RVEF measured by radionuclide angiography is thought to be an important parameter to predict the prognosis of patients with pulmonary hypertension [3]. It has been reported that MRI-based RVEF is more reliable than pulmonary vascular resistance (PVR) measured by right cardiac catheterization as a prognostic predictor [4]. However, radionuclide angiography as well as MRI is not common in general practice because of the size of the equipment needed and the high cost of these tests. On the other hand, 2D echocardiography is a simpler, noninvasive and less expensive method that is frequently used, even in outpatient clinics, and is often used to assess right cardiac function [5, 6]. Therefore, the American Society of Echocardiography (ASE) has suggested several right cardiac function parameters, but many of them have not been established.
In the present study, right cardiac function parameters were measured by echocardiography in patients with pulmonary hypertension. The assessment of right cardiac function is important to predict the prognosis of these patients, and thus we evaluated the association of these parameters with RVEF measured by radionuclide angiography.
Subjects and methods
Subjects
Subjects included 23 patients (5 males and 18 females aged 64 ± 14 years old) with pulmonary hypertension. The pulmonary hypertension was diagnosed using right cardiac catheterization and pulmonary angiography, based on the guidelines of the Japanese Circulation Society in 2012 (JCS 2012). Basal diseases were idiopathic pulmonary artery hypertension in 7 patients, chronic thromboembolic pulmonary hypertension in 13, pulmonary hypertension associated with congenital heart disease in 1, pulmonary hypertension associated with chronic obstructive lung disease in 1, and pulmonary hypertension associated with collagen disease in 1. The severity of dyspnea was class I in 3 patients, class II in 16, class III in 2, and class IV in 2, based on the World Health Organization (WHO) functional classification. The baseline medications were beraprost (not approved in United States and Europe) in 21 patients, sildenafil in 4, tadalafil in 6, and bosentan in 5 (Table 1). This study was approved by the ethics committee of Dokkyo Medical University and all patients provided written informed consent before participation.
Methods
In the 23 patients, a total of 30 radionuclide angiography procedures were performed (7 patients underwent 2 procedures) (Table 1). Echocardiography was also performed within several days of each radionuclide angiography procedure.
Radionuclide angiography
Red blood cells were labeled in vivo with an injection of 740 MBq of 99mTc-albumin 30 min after intravenous administration of pyrophosphate. A dual-head scinticamera (GCA 7200; Toshiba Corporation, Tokyo, Japan) equipped with a high-resolution collimeter was used to collect images as follows: (1) dynamic collection (collection every 0.5 s for 2 min), (2) STATIC collection (a front camera at an angle of 30° in the RAO direction, a lateral camera at an angle of 90° in the LAO direction), and (3) ECG-synchronized collection (an R–R acceptance window ±10%, 32 frames at cardiac cycle). Data sets were manually reconstructed by experienced physicians according to the orientation mode of the American College of Cardiology. For processing, mid-ventricular locations were determined by the maximum activity in the likely ventricle, and a continuous dynamic biventricular surface was generated by the combination of spatial and temporal information. Left and right ventricular volumes were computed from the number of voxels >50% of maximum volume counts, and LVEF and RVEF were computed from count changes in each area of the left and right ventricles with counts >35% of the maximum volume counts. The normal range of RVEF by radionuclide angiography was considered to be 45–50%.
Echocardiography
Among various echocardiographic parameters that the ASE recommends for evaluating right heart function, we selected the following 4 candidates: right ventricular Tei index (RV Tei index), right ventricular fractional area change (RVFAC), tricuspid annular plane systolic excursion (TAPSE), and tricuspid annular peak systolic velocity (S′). Echocardiography was performed by skilled physicians using a Vivid 7 (GE Medical Systems, Horton, Norway) instrument, and each parameter was measured at the end-expiratory phase. Pulsed wave Doppler imaging was acquired with subjects in the lateral decubitus position during shallow respiration. Tei index, which comprehensively indicates both systolic and diastolic function of the ventricles, is commonly calculated using isovolumic relaxation time (IRT), isovolumic contraction time (ICT), and ejection time (ET) according to the following formula: Tei index = (ICT + IRT)/ET [7,8,9]. We calculated the RV Tei index as RV Tei index = (a − b)/b, where ‘a’ is the period from the cessation to the onset of right ventricular inflow velocity observed in the apical four-chamber view, and ‘b’ is the duration of right ventricular outflow velocity observed in the parasternal short-axis view. RV Tei index ranges normally from 0.15 to 0.40 in healthy adults; thus, RV Tei index >0.40 suggests that right ventricular function is impaired [8, 9]. Subsequently, we measured right ventricular end-diastolic area (RVEDA) and end-systolic area (RVESA) in the apical four-chamber view, and RVFAC was calculated as RVFAC = (RVEDA − RVESA) × 100/RVEDA (%). A normal range of RVFAC is thought to be 35–63% in the ASE guidelines; [10] thus, RVFAC <35% is thought to reflect impaired right cardiac function. TAPSE was calculated by measuring the excursion of the tricuspid valve annulus by M-mode rendering at the free-wall side in the four-chamber view. Its normal range is 16–30 mm; thus, TAPSE <16 mm is thought to reflect impaired right cardiac function [10]. Guided by the four-chamber view, a 5-mm sample volume was placed at the lateral corner of the tricuspid annulus, exactly at the attachment of the anterior leaflet of the tricuspid valve. We were careful to obtain an ultrasound beam parallel to the direction of tricuspid annular motion. Finally, S′ was measured as the maximum velocity of tricuspid valve excursion at the free-wall side using tissue Doppler imaging. The velocities were recorded for 3–5 cardiac cycles and averaged. The normal range of S′ is 10–19 cm/sec; thus, S′ < 10 cm/sec is thought to reflect impaired right cardiac function.
Statistical analysis
Data were expressed as mean ± standard deviation and n (%). All statistical analyses were performed using statistical software (Stat Mate IV, ATMS, Tokyo, Japan). Multiple group comparisons for continuous variables were performed using a one-way analysis of variance (ANOVA) followed by a post hoc Bonferroni test. The correlations between 2 variables were examined by calculating Pearson’s correlation coefficient. Multiple regression analysis was performed to assess the independent correlation of the RVEF measured by radionuclide angiography with the echocardiographic right ventricular parameters. Receiver operating characteristic (ROC) curve analysis was performed to calculate sensitivity, specificity, and area under the curve (AUC). P values <0.05 were considered to be statistically significant.
Results
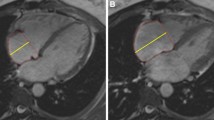
In 23 patients, right ventricular systolic pressure was 53.8 ± 17.4 mmHg, and the grade of tricuspid regurgitation was mild in 19 (83%), moderate in 4 (14%), and severe in none, based on initial Doppler echocardiography (Table 1). RVEF by radionuclide angiography (n = 30) was 31.1 ± 7.4%. In patients grouped according to their WHO functional class, the average RVEF was 34.2% in class I (n = 3), 32.3% in class II (n = 23), 28.8% in class III (n = 2) and 14.6% in class IV (n = 2). Values of each echocardiographic parameter in the 29 measurements were as follows: RV Tei index, 0.44 ± 0.21; RVFAC, 33.9 ± 9.0%; TAPSE, 19.0 ± 4.0 mm; and S′, 11.2 ± 2.8 cm/s. RVEF measured by radionuclide angiography was significantly and negatively correlated with RV Tei index measured by Doppler echocardiography (r = −0.601, P < 0.0005). However, RVEF was not correlated with RVFAC (r = 0.248), TAPSE (r = 0.031) or S′ (r = 0.097) (Fig. 1). Multiple regression analysis showed that RVEF was correlated with RV Tei index, and this correlation was independent of the other echocardiographic right ventricular function parameters (r = −0.644, P < 0.005) (Table 2) . ROC curve analysis indicated that an RV Tei index cut-off value of 0.371 was the best predictor of RVEF ≤35% (AUC = 0.768, sensitivity = 0.857, selectivity = 0.667) (Fig. 2).
The relationship between RVEF measured by radionuclide angiography and right ventricular function parameters measured by echocardiography. RVEF was significantly and negatively correlated with RV Tei index, but not with RVFAV, TAPSE, or S′. RVEF right ventricular ejection fraction, RV Tei index right ventricular Tei index, RVFAC right ventricular fractional area change, TAPSE tricuspid annular plane systolic excursion, S′ tricuspid annular peak systolic velocity
Discussion
In the present study, we investigated echocardiographic parameters that indicated right cardiac function in patients with pulmonary hypertension, using RVEF measured by radionuclide angiography as a gold standard. As a result, among various echocardiographic right ventricular function parameters such as RV Tei index, RVFAC, TAPSE, and S′, RV Tei index was the only parameter that showed a strong negative correlation with RVEF. These results suggest that RV Tei index may be a useful indicator of right ventricular systolic function in patients with pulmonary hypertension.
The right ventricle is composed of an inflow tract, trabeculated apex, and outflow tract; it has a trigonal pyramidal shape, whereas the left ventricle has a cone shape. Right ventricular contraction occurs from the inflow tract to the apical trabecular zone, and then reaches the outflow tract [11]. The contraction of the right ventricle includes the following components: long-axial shortening from the apex toward the tricuspid valve annulus caused by right ventricular papillary muscle contraction; the approach of the right ventricular free wall toward the septum caused by right ventricular contraction itself and by right ventricular strain associated with left ventricular contraction; and septal projection toward the right side by its bend caused by left ventricular contraction [12]. Furthermore, the right ventricular wall is composed of both subendocardial and subepicardial myocardial layers. The contraction of the subendocardial myocardium is directed towards the long axis, whereas the subepicardial myocardium is circumferentially oriented, and long axis contraction is more dominant in the normal right ventricle [13]. Such morphological and dynamic features of the right ventricle make it difficult to measure RVEF by echocardiography using Simpson’s method. In that respect, MRI or radionuclide angiography seems to be suitable to measure the RVEF. Vanderpool et al. [14] have shown that an MRI-based RVEF <35% was of poor prognosis in patients with pulmonary hypertension. Some investigators have reported that RVEF measured by MRI was correlated with each of the echocardiographic parameters such as RV Tei index, RVFAC, TAPSE, and S′ [15,16,17]. On the other hand, Cournand et al. [18] have demonstrated that pulmonary hypertension patients with a baseline RVEF >25%, measured by radionuclide angiography, had better survival than those with a RVEF <25%. In the present study, we selected 4 echocardiac parameters, RV Tei index, RVFAC, TAPSE, and S′, to be compared with RVEF measured by radionuclide angiography, because the ASE has advocated these 4 as powerful indicators of right cardiac function. In patients with pulmonary hypertension, Badagliacca et al. [19] demonstrated that RVFAC <36.5% along with peak oxygen pulse (peak oxygen uptake/heart rate) <8 mL/beat showed very low survival rate, and Ghio et al. [20] reported that a baseline TAPSE ≥15 mm was associated with a lower risk of death. In our results, RVEF by radionuclide angiography was correlated with RV Tei index alone, but not with any other echocardiographic parameters. Possible reasons for the lack of significant associations between RVEF and the other parameters may be as follows: first, accurate measurement of RVFAC is difficult because of complex right ventricular contraction patterns as mentioned above; second, the RVFAC is evaluated only at the inflow tract or the trabeculated apex, and thus cannot represent RVEF when contraction of the outflow tract greatly contributes to RVEF. Although both TAPSE and S′ represent long-axial contraction from the apex toward the tricuspid annulus [8], they are susceptible to changes due to volume loading. Therefore, the relationship between RVEF and these parameters depends on the severity of tricuspid regurgitation in patients with pulmonary hypertension [21]. In contrast, RV Tei index is calculated as a ratio of the time phase measured from blood flow waveforms at the inflow and outflow tracts, and thus is not influenced by the morphological features of the right ventricle [9]. Several investigators have reported an association between RV Tei index and RVEF. Moreover, patients with pulmonary hypertension who have an increased RV Tei have a poor prognosis [9, 22]. We believe that the results of our present study substantially support these previous findings.
Study limitations
The present study has several potential limitations. First, we used RVEF measured by radionuclide angiography as a gold standard, although MRI-based RVEF seems to be more reliable, considering previous descriptions [23]. In addition, as mentioned above, cut-off values of RVEF to predict prognosis of pulmonary hypertension were different between MRI (35%) [14] and radionuclide angiography (25%) [18]. Moreover, in our ROC curve analysis, we determined the value of RVEF by radionuclide angiography to be predicted by RV Tei index as a ≤35%, which is higher than the cut-off value to predict prognosis in the previous report [18]. Next, this study included a small sample size (29 measurements in 22 patents), and included duplicate measurements in 7 patients. In the future, we need to investigate the relationship between RVEF by radionuclide angiography or MRI and echocardiographic parameters in a larger number of patients. In addition, further investigation is needed in terms of therapeutic efficacy evaluation. In the present study, the patients had various causes of pulmonary hypertension. Especially, in chronic thromboembolic pulmonary hypertension, diastolic pulmonary artery pressure is commonly higher, so the pressure gradient across the pulmonary valve is higher compared with idiopathic pulmonary artery hypertension, potentially leading to differences in right ventricular hemodynamics between these two types of pulmonary hypertension. Therefore, a separate evaluation is needed in each type of pulmonary hypertension. Finally, evaluation of the interaction between the left and right ventricles in pulmonary hypertension would also be important.
Conclusion
Among echocardiography-based parameters, only RV Tei index is associated with RVEF measured by radionuclide angiography. The result suggests that RV Tei index is the most relevant echocardiographic parameter to estimate RVEF in patients with pulmonary hypertension. From our results, we can envision that RV Tei index-guided therapeutic interventions would be promising in the future.
References
Brent BN, Mahler D, Matthay RA, Berger HJ, Zaret BL, Lister G (1984) Noninvasive diagnosis of pulmonary arterial hypertension in chronic obstructive pulmonary disease: right ventricular ejection fraction at rest. Am J Cardiol 53(9):1349–1353
Kawut SM, Al-Naamani N, Agerstrand C, Rosenzweig EB, Rowan C, Barst RJ, Bergmann S, Horn EM (2009) Determinants of right ventricular ejection fraction in pulmonary arterial hypertension. Chest 135(3):752–759
Zafrir N, Zingerman B, Solodky A, Ben-Dayan D, Sagie A, Sulkes J, Mats I, Kramer MR (2007) Use of noninvasive tools in primary pulmonary hypertension to assess the correlation of right ventricular function with functional capacity and to predict outcome. Int J Cardiovasc Imaging 23(2):209–215
van de Veerdonk MC, Kind T, Marcus JT, Mauritz GJ, Heymans MW, Bogaard HJ, Boonstra A, Marques KM, Westerhof N, Vonk-Noordegraaf A (2011) Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol 58(24):2511–2519
Briongos Figuero S, Moya Mur JL, García-Lledó A, Centella T, Salido L, Aceña Navarro Á, García Martín A, García-Andrade I, Oliva E, Zamorano JL (2016) Predictors of persistent pulmonary hypertension after mitral valve replacement. Heart Vessels 31(7):1091–1099
Hioka T, Kaga S, Mikami T, Okada K, Murayama M, Masauzi N, Nakabachi M, Nishino H, Yokoyama S, Nishida M, Iwano H, Sakakibara M, Yamada S, Tsutsui H (2016) Overestimation by echocardiography of the peak systolic pressure gradient between the right ventricle and right atrium due to tricuspid regurgitation and the usefulness of the early diastolic transpulmonary valve pressure gradient for estimating pulmonary artery pressure. Heart Vessels. doi:10.1007/s00380-016-0929-4
Tei C (1995) New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol 26(2):135–136
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 26(6):357–366
Tei C, Dujardin KS, Hodge DO, Bailey KR, McGoon MD, Tajik AJ, Seward SB (1996) Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr 9(6):838–847
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713
Haddad F, Hunt SA, Rosenthal DN, Murphy DJ (2008) Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation 117(11):1436–1448
Rushmer RF, Crystal DK, Wagner C (1953) The functional anatomy of ventricular contraction. Circ Res 1(2):162–170
Petitjean C, Rou N, Cluzel P (2005) Assessment of myocardial function: a review of quantification methods and results using tagged MRI. J Cardiovasc Magn Reson 7(2):501–516
Vanderpool RR, Richard F, Naeije R, Hunter K, Simon MA (2016) Simple functional imaging of the right ventricle in pulmonary hypertension: can right ventricular ejection fraction be improved? Int J Cardiol 223:93–94
Anavekar NS, Gerson D, Skali H, Kwong RY, Yucel EK, Solomon SD (2007) Two-dimensional assessment of right ventricular function: an echocardiographic-MRI correlative study. Echocardiography 24(5):452–456
Kaul S, Tei C, Hopkins JM, Shah PM (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107(3):526–531
Pavlicek M, Wahl A, Rutz T, de Marchi SF, Hille R, Wustmann K, Steck H, Eigenmann C, Schwerzmann M, Seiler C (2011) Right ventricular systolic function assessment: rank of echocardiographic methods vs. cardiac magnetic resonance imaging. Eur J Echocardiogr 12(11):871–880
Courand PY, Pina Jomir G, Khouatra C, Scheiber C, Turquier S, Glérant JC, Mastroianni B, Gentil B, Blanchet-Legens AS, Dib A, Derumeaux G, Humbert M, Mornex JF, Cordier JF, Cottin V (2015) Prognostic value of right ventricular ejection fraction in pulmonary arterial hypertension. Eur Respir J 45(1):139–149
Badagliacca R, Papa S, Valli G, Pezzuto B, Poscia R, Manzi G, Giannetta E, Sciomer S, Palange P, Naeije R, Fedele F, Vizza CD (2016) Echocardiography combined with cardiopulmonary exercise testing for the prediction of outcome in idiopathic pulmonary arterial hypertension. Chest 150(6):1313–1322
Ghio S, Pica S, Klersy C, Guzzafame E, Scelsi L, Raineri C, Turco A, Schirinzi S, Visconti LO (2016) Prognostic value of TAPSE after therapy optimisation in patients with pulmonary arterial hypertension is independent of the haemodynamic effects of therapy. Open Heart 3(1):e000408
Hsiao SH, Lin SK, Wang WC, Yang SH, Gin PL, Liu CP (2006) Severe tricuspid regurgitation shows significant impact in the relationship among peak systolic tricuspid annular velocity, tricuspid annular plane systolic excursion, and right ventricular ejection fraction. J Am Soc Echocardiogr 19(7):902–910
Yeo TC, Dujardin KS, Tei C, Hodge DO, Rossi A, Seward JB (1998) Value of a Doppler-derived index combining systolic and diastolic time intervals in predicting outcome in primary pulmonary hypertension. Am J Cardiol 81(9):1157–1161
Vonk Noordegraaf A, Westerhof BE, Westerhof N (2017) The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol 69(2):236–243
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Amano, H., Abe, S., Hirose, S. et al. Comparison of echocardiographic parameters to assess right ventricular function in pulmonary hypertension. Heart Vessels 32, 1214–1219 (2017). https://doi.org/10.1007/s00380-017-0991-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-0991-6