Abstract
Endomyocardial biopsy (EMB) and cardiac magnetic resonance (CMR) are useful modalities to study the characteristics of myocardial tissue. However, the prognostic impact of both diagnostic tools to predict subsequent left ventricular reverse remodeling (LVRR) has not been well elucidated. A total of 187 consecutive patients with idiopathic dilated cardiomyopathy (IDCM) who were treated by optimal pharmacotherapy (OPT) and underwent EMB of the LV wall were investigated. The myocardial specimens were semiquantitatively evaluated measuring cardiomyocyte degeneration (CD), interstitial fibrosis (IF), and hypertrophy. In addition, late gadolinium enhancement (LGE)-CMR was performed in 78 (48 %) patients. Seventy-eight (48 %) patients developed LVRR, defined as a ≥10 % increase in LV ejection fraction with a ≥10 % decrease in indexed LV end-diastolic dimension at 12 months after OPT. Multivariate regression analysis revealed that CD (P = 0.003), but not IF (P = 0.320), was an independent predictor of LVRR. In the patients with not only EMB but also CMR, the CD score and LGE area were independent predictors of LVRR (odds ratios/P values 0.268/0.010, 0.855/<0.001, respectively). The patients with mild CD and negative LGE had a better achievement rate of LVRR than those with severe CD and positive LGE (74 vs. 19 %). A combination of CD score on EMB and LGE-CMR is useful to predict subsequent LVRR in IDCM patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Idiopathic dilated cardiomyopathy (IDCM) is a common myocardial disease typically diagnosed by impaired left ventricular ejection fraction (LVEF) and LV dilation of unknown etiology. Heart failure (HF) management such as β-blockers (BB) [1] and CRT [2] has been shown to induce LV reverse remodeling (LVRR), characterized by a decrease in LV volume and improvement in pump function. The long-term management and stratification of these patients would benefit from the identification of reliable clinical predictors of LVRR to optimize the treatment strategy and patient prognosis.
A few studies attempted to identify clinical characteristics of IDCM predictive of LVRR developing in response to optimal pharmacotherapy (OPT). Merlo et al. [3] found that higher baseline systolic blood pressure and the absence of left bundle branch block were predictors of LVRR in a large population of IDCM patients. Choi et al. [4] found that higher systolic blood pressure, QRS duration <120 ms, the use of BB, and low midterm NT-proBNP levels were independent predictors of LVRR. Although LVRR may be derived from viable myocardium at baseline and following recovering cardiomyocytes and enhanced stem cell differentiation, the predictive value of tissue characteristics of the myocardium for LVRR has been scarcely investigated in clinical practice. Therefore, the aim of this study was to determine the relationship between LVRR after OPT in IDCM patients and myocardial tissue characteristics using both endomyocardial biopsy (EMB) and cardiac magnetic resonance (CMR).
Methods
Study population
This retrospective study involved 187 consecutive patients with IDCM who received OPT during their hospitalization at the Kitasato University Hospital between 1996 and 2012. The diagnosis of IDCM was based on various modalities including coronary angiography and EMB. Among these subjects, 78 consecutive patients without contraindication such as renal dysfunction also underwent late gadolinium enhancement (LGE)-CMR in 2008–2012. Echomorphometric abnormalities were defined as follows: LVEF <45 %, indexed LV end-diastolic dimension (LVDDI) >32 mm/m2, and LV wall thickness <12 mm. Patients with significant coronary artery disease (>50 % luminal stenosis on coronary angiography or prior myocardial infarction), cardiac amyloidosis, sarcoidosis, acute myocarditis, metabolic disorders, endocrine dysfunction, neuromuscular diseases, peripartum cardiomyopathy, organic heart valve disease, the use of cardiotoxic drugs, and alcohol abuse were excluded. During this study period, 25 patients diagnosed histologically with myocarditis were also excluded. After HF decompensation was relieved by standard methods if necessary, BB was up-titrated toward the target dose in Japan [5] (carvedilol 20 mg/day, bisoprolol 5 mg/day). Daily doses of BB were demonstrated as equivalents of carvedilol (carvedilol equivalent doses: metoprolol, 2; bisoprolol, 0.25). In this study, informed consent was obtained in accordance with the protocol, which was approved by our institution’s Committee on Human Investigation.
Clinical measurements and echocardiographic evaluation
Baseline clinical parameters were recorded from general laboratory analyses, electrocardiography (ECG), and echocardiography under clinically stable conditions before hospital discharge. 162 patients underwent echocardiograms. It was repeated at least twice at discharge and 12 months later. M-mode images were obtained in the left parasternal long-axis view to measure the dimension of each chamber. LVEF was calculated with a modified Simpson’s method using biplane images in the apical long-axis view. LVRR was defined as an increase in LVEF of ≥10 % and a decrease in LVDDI of ≥10 % [6] at 12 months after the administration of OPT.
Histopathological evaluation by EMB
At least three EMB samples were obtained at baseline from the posterior wall of the LV chamber in 162 patients. The specimens were fixed in formalin and sectioned, and tissue sections were subjected to hematoxylin–eosin and Masson’s trichrome staining. When showed significant infiltration of small round cells such as leukocytes (>5 small round cells per 400×-power microscope), tissue sections were labeled with antibodies against CD3, CD68, and tenascin C [7] to exclude myocarditis. Ten representative points, containing no endocardium or blood vessels, were randomly selected from each layer and evaluated using a 200×-power microscope. The following parameters were assessed: (1) interstitial fibrosis (IF), (2) hypertrophy (cross-sectional diameter at nuclear level), (3) vacuolization, and (4) scarcity of myofibrils (Fig. 1). The measurements were graded using a typical semiquantitative scoring system: 0 = no changes or minimal, 1 = mild, 2 = moderate, and 3 = severe changes. Cardiomyocyte degeneration (CD) was defined as follows: total score of “vacuolization” plus “scarcity of myofibrils”/2. This histological evaluation, modified from a previous study [8], was performed independently by threw well-trained cardiac pathologists blinded to the clinical data. Inter-rater reliability of the histopathological analysis was as follows: (1) Interstitial fibrosis (weighted κ statistics = 0.641), (2) hypertrophy (weighted κ statistics = 0.746), (3) vacuolization (weighted κ statistics = 0.588), (4) scarcity of myofibrils (weighted κ statistics = 0.515). When the decisions differed between them, the final decision was made by the third blinded investigator.
Histopathological scores on EMB specimens. a Interstitial fibrosis. Proliferation of collagen fibers could be easily detected on Masson’s Trichrome stained sections and the severity and extent can be graded. Grade 0 signified no apparent collagen fiber proliferation except for small islets of fibrous tissue around the capillaries and were intercellular single layer of collagenous tissue as in normal myocardium. Grade 1 was surrounded by fibers of two or more layers. The bundles of myocardial fibers were surrounded in grade 2. Most prominent fibrosis, covering more than half the area of specimen was graded as 3. Bar indicates 100 μm. b Hypertrophy. To evaluate the degree of hypertrophy, the shortest diameters of cardiomyocytes were measured only in nucleated transverse sections. Grade 0 was less than 18 μm. Grade 1 was from 19 to 23 μm. Grade 2 was from 24 to 28 μm. Grade 3 was more than 29 μm. Bar indicates 50 μm. c Vacuolization. Vacuolization should be applied to perinuclear or other areas where myofibrils disappeared with or without deposits of granular substance. Vacuolization often showed a perinuclear halo or a punched out area in the cytoplasm (grade 1). In a more disorganized myocardium, vacuoles or deposits often occupied more than one-third (grade 2) or a half (grade 3) of the area of muscle cells along with loss of myofibrils. Bar indicates 100 μm. d Scarcity. In degenerated myocardial cells, myofibrils were occasionally decreased in number or absent (grade 1). To identify a scarcity of myofibrils, an artifact-free area in longitudinal sections should be examined since the myofibrils appeared to be falsely scarce due to overstretched nature in excessively contracted areas. Marked scarcity of myofibrils was often accompanied by vacuoles or deposition of granular or peculiar substance (grade 2). When even worse, myofibrils showed a wavy form (grade 3). Bar indicates 100 μm
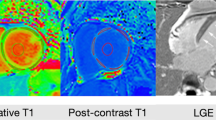
Histopathology by LGE-CMR
Among the patients who underwent UCG and EMB, 78 patients without contraindication such as renal dysfunction also underwent LGE-CMR. The interval between EMB and CMR was <3 weeks. All CMR examinations were performed using a 1.5-T clinical scanner (Signa HDxt 1.5T; GE Healthcare, Milwaukee, WI, USA) with a maximum gradient strength of 33 mT/m and slew rate of 120 mT/m/s. An eight-channel phased-array coil and a vector ECG were used for signal reception and cardiac gating, respectively. The ECG-gated two-dimensional LGE images were acquired 10–15 min after the intravenous injection of 0.2 mmol/kg gadolinium using segmented inversion recovery fast gradient-echo sequences with the following parameters: echo time, 4.2 ms; repetition time, 8.0 ms; views per segment, 24; flip angle, 20°; inversion time, 150–220 ms; bandwidth, ±25 kHz; number of excitations, 1; in-plane resolution, 1.5 × 1.7 mm2; field of view, 340 × 340 mm; slice thickness, 8 mm; interslice gap, 8 mm; and four slices acquired in the LV short-axis over two R–R intervals. The presence of LGE was determined by two experienced independent observers blinded to patients’ outcome. The extent of LGE was expressed as “LGE area,” defined as an area showing a signal intensity of less than or equal to five standard deviations above the mean of the remote reference myocardium. The LGE area was quantified by semiautomatic planimetry on the short-axis contrast images using Ziostation 2 (Ziosoft, Tokyo, Japan).
Clinical observations and statistical analysis
Clinical outcomes were periodically assessed at our outpatient clinics and/or associated institutes, and the clinical data were collected until the end of 2013. The patients were divided into two groups: those with LVRR <12 months (LVRR groups), and those without LVRR <12 months or until death (no-LVRR groups). The continuous variables were compared using the Student’s t test for normal distributions or the nonparametric equivalent Mann–Whitney U test for abnormal distributions. The binary variables were analyzed by Chi square test. Event-free survival curves were drawn according to the Kaplan–Meier method, and the curves of the two groups were compared using the log-rank test. Cardiovascular events including sudden death, readmission for HF exacerbation, and major ventricular arrhythmias (MVAs) were the secondary endpoints. Sudden death was defined as immediate death occurring within 1 h of the onset of symptoms or death in stable New York Heart Association (NYHA) functional class I–III. MVAs were defined as ventricular fibrillation/flutter, sustained ventricular tachycardia (hemodynamically unstable or lasting >30 s), or arrhythmia requiring implanted cardioverter/defibrillator intervention. Logistic regression analysis was used to assess LVRR at 12 months. Multivariate logistic regression analysis using a forward stepwise approach was performed on parameters found significant by univariate analysis. All values were reported as mean ± standard deviation or median (25th–75th percentile) or frequency and percentages. A P value <0.05 was considered to indicate statistical significance. The entire analysis was performed using a JMP 10 software for Windows (SAS Institute Inc, North Carolina, USA).
Results
Predictors of LVRR and outcome in patients who underwent EMB
The mean age of subjects enrolled in this study were 55 ± 14 years old. 64 % of patients were hospitalized because of decompensated heart failure. At discharge, most of patients (93 %) exhibited NYHA functional class I or II and a LVEF of 31 ± 8 % with mostly-optimized pharmacotherapy (Table 1). At 12 months after hospital discharge, LVRR was detected in 78 patients (48 %). Kaplan–Meier curves significantly indicated better cardiac event-free survival rates in the LVRR group than that in the no-LVRR group (Fig. 2). There were significant differences between the two groups in terms of History of decompensated heart failure, NYHA functional class, QRS duration, and BB dosage. Regarding myocardial tissue characterization by EMB, all three histological parameters were significantly different between the two groups, i.e., IF, hypertrophy, and the CD score of vacuolization and myofibril scarcity (Table 1).
Multivariate logistic regression analysis identified the CD score, QRS duration, and BB dosage as independent predictors of LVRR (Table 2). Cardiac event-free survival rates were significantly better in patients with mild CD (score 0–1) than in those with severe CD (score 2–3; Fig. 3a), but a similar trend was not recognized with regard to IF (Fig. 3b).
Histopathological evaluation of EMB and prognosis. In 162 patients who underwent EMB, cardiac event-free survival rates were significantly higher in patients with mild cardiomyocyte degeneration (CD; score 0–1.5) than in those with severe CD (score 2–3) (P = 0.020) (a), but a similar trend was not recognized with regard to interstitial fibrosis (IF) (b)
Predictive value of EMB and simultaneous CMR for LVRR and outcome
The LVRR subgroup of patients who underwent both EMB and CMR presented similar characteristics at baseline (Table 1). There was no correlation between the LGE area in CMR and any of the EMB histological scores, including IF (Fig. 4). Multivariate logistic regression analysis revealed that the CD score, LGE area, and QRS duration are independent predictors of LVRR (Table 3). When the patients were divided into four groups according to the CD score and presence of LGE, patients with mild CD and negative LGE had markedly higher achievement of LVRR than those with severe CD and positive LGE (74 vs. 19 %; Fig. 5).
Myocardial tissue characterization by EMB and CMR for predicting LVRR. Patients with mild CD and negative LGE had good achievement rate of LVRR compared to those with severe CD and positive LGE (74 vs. 19 %). LVRR left ventricular reverse remodeling, LGE late gadolinium enhancement, CD cardiomyocyte degeneration
Discussion
EMB for IDCM in clinical practice
Histopathological evaluation by EMB suggests that CD is an independent predictor of LVRR and outcome in IDCM patients managed by OPT. To the best of our knowledge, this is the first report indicating that EMB could predict LVRR in IDCM patients.
Recently, EMB has emerged as an approach to the differential diagnosis of IDCM to rule out myocarditis and infiltrative cardiomyopathies. As such, the histopathological aspects of the myocardium in IDCM patients are rarely described because EMB is only conducted in well-equipped cardiology institutes as a diagnostic tool for Class IIa conditions, according to the most recent HF guidelines [9]. In fact, one may question the clinical merit of assessing myocardial histology by EMB. Previous reports established a relationship between quantitative histological findings on EMB [10] or autopsy [11] and LV contractile function in IDCM patients. However, in recent years, with the recognition of evidence-based prognosis-oriented therapies such as BB and CRT, the value of histopathological findings such as myocardial fibrosis to correlate clinical and hemodynamic parameters has become controversial or even unfavorable [12].
Regarding the predictive value of EMB for LVRR, there is an ongoing debate on the relationship between the extent of myocardial fibrosis evaluated by EMB and LVRR in response to therapies such as BB or LVAD. Some reports demonstrated a significant correlation, [13, 14] whereas others have contradicted these findings, [15, 16] as shown in the present study. Although histological analysis targeting myocardial inflammation may assist in predicting spontaneous LVRR, [17, 18] the discussion is restricted to intrinsic cardiac recovery because this study excluded cases of histologically-proven myocarditis based on the immunohistochemical analysis of EMB.
EMB and LGE-CMR to detect myocardial fibrosis
Although it has been established that myocardial fibrosis evaluated by both EMB and LGE-CMR can estimate the extent of fibrosis in myocardial tissue [19, 20] the present study found no significant correlation between the degree of IF in EMB and LGE area by CMR (Fig. 4). The reasons for this apparent discrepancy remain elusive but may relate to the pathogenesis of myocardial fibrosis. Several mechanisms are believed to contribute to the development of myocardial fibrosis such as inflammation, neurohumoral changes, and microvascular ischemia [21]. Both reactive and reparative patterns of fibrosis are detected in IDCM patients. The presence of focal fibrosis detected by LGE-CMR was related to reparative inflammation, presumably leading to an adverse outcome [22]. On the other hand, diffuse cardiac fibrosis, mainly of reactive origin, cannot be detected by LGE-CMR [23]. Therefore, normal LGE-CMR imaging does not always exclude an increased IF that could be detected by EMB. Furthermore, there are some cases of IDCM whose interstitial myocardial fibrosis is detected by LGE-CMR but hardly recognized by EMB because of the difficulty to collect samples deeper than the endomyocardium. The present study identified the LGE area in CMR imaging, but not the degree of IF observed by EMB, as independent predictor of LVRR in response to OPT. Therefore, LGE-CMR provides more detailed histopathological information on the entire myocardial interstitium to predict HF prognosis compared with the focal restrictions of EMB.
Cardiomyocytes in EMB as indicators of cardiac function and prognosis
The physiological significance of cardiomyocytes for the pathogenesis of HF has been investigated at length, particularly in basic science. However, the morphological characteristics of cardiomyocytes have not been established using noninvasive diagnostic tools in clinical practice. So far, tissue characterization using CMR has been limited to myocardial fibrosis [24]. Myocardial scintigraphy can only estimate myocardial status by compiling information on dysfunctional cardiomyocytes and myocyte loss [25]. In contrast, EMB analysis assesses cardiac status and predicts LVRR by directly evaluating the cardiomyocytes. Notably, it has been demonstrated that the morphological evaluation of cardiomyocytes by EMB avoids the critical issue of sampling error always indicated for the evaluation of IF [10].
The present study determined the CD score of patients with IDCM under a light microscope based on cytoplasmic vacuolization and the scarcity of myofibrils. Logistic regression analysis identified this EMB characteristic as an independent predictor of LVRR in response to OPT. Scarcity is defined as the absence or decrease in the number of myofibrils. Marked scarcity is often accompanied by vacuolization [26], leading to colliquative myocytolysis [27]. This condition is associated with low cardiac pump function and dilated ventricular chambers reported in some reports [28]. Conversely, a lack of correlation was reported in others between colliquative myocytolysis and clinical parameters, i.e., chamber dilatation, cardiac indices, wall thickness, and myocardial ischemia [29]. Although myocardial vacuolization also occurs in other pathological conditions such as storage diseases or parasitic diseases, it may also be an artifact of autolysis or histological processing. Furthermore, the scarcity of myofibrils and prominent cytoplasmic vacuolization are sometimes shown to be derived from autophagic vacuoles by light microscopy [30], which are associated with adverse outcome in patients with IDCM and severe HF [31]. The clinical significance of vacuolization has not been fully established, presumably because of the various compositions of vacuoles. This issue would be clarified by studies using electron microscopy.
Clinical implication
The improvement of prognosis is currently the most important clinical goal of HF management teams, as indicated by the growing number of large-scale clinical trials. However, in practice, it is very difficult for the medical staff and patients to recognize survival benefit as the sole aim of pharmacotherapy and/or nonpharmacotherapy. In this context, additional clinical indicators of prognosis must be identified to develop personalized therapies. Among these, LVRR is generally recognized as an important outcome and indicator of a favorable prognosis [32].
Another major clinical benefit of predicting LVRR is the ability to make informed decisions regarding the optimal treatment strategy. When the probability of LVRR is high, even if baseline LVEF is low, it may be possible to delay invasive procedures, such as CRT, to see if LV functions may improve sufficiently by OPT alone. This is particularly important for elderly patients who cannot afford such costly and invasive treatments or do not meet the minimal health conditions. The present study demonstrated that the tissue characterization of the morphological reorganization of myocardial parenchyma (cardiomyocyte degeneration) and stroma (interstitial fibrosis), on the basis of the CD score on EMB and LGE area on CMR, has a prognostic impact on subsequent LVRR in response to OPT. Comprehensive management, including OPT and cardiac rehabilitation, may be suitable for patients with IDCM with negative LGE-CMR and mild CD on EMB. In summary, CMR imaging and EMB are complementary diagnostic tools to predict LVRR, and they provide distinct information for the evaluation and management of IDCM.
Study limitations
The present study has some limitations. Because it is a single center study, selection bias was a major concern. Given the low number of cardiac events in our cohort, accounting for a relatively small number of patients, the findings of this observational study should be interpreted with caution. There is also an inherent limitation to the EMB analysis. Although uniformly-distributed morphological changes over the entire myocardium is a prerequisite in patients with IDCM [33, 34], some focal processes could affect our analysis through the so-called sampling error for EMB. Finally, the proposed etiology of vacuolization that was based on light microscopy should be verified by detailed examination using an electron microscope.
References
Hori M, Sasayama S, Kitabatake A, Toyo-oka T, Handa S, Yokoyama M, Matsuzaki M, Takeshita A, Origasa H, Matsui K, Hosoda S, Investigators MUCHA (2004) Low-dose carvedilol improves left ventricular function and reduces cardiovascular hospitalization in Japanese patients with chronic heart failure: the Multicenter Carvedilol Heart Failure Dose Assessment (MUCHA) trial. Am Heart J 147:324–330
Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, Tavazzi L, Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators (2005) The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Eng J Med 352:1539–1549
Merlo M, Pyxaras SA, Pinamonti B, Barbati G, Di Lenarda A, Sinagra G (2011) Prevalence and prognostic significance of left ventricular reverse remodeling in dilated cardiomyopathy receiving tailored medical treatment. J Am Coll Cardiol 57:1468–1476
Choi JO, Kim EY, Lee GY, Lee SC, Park SW, Kim DK, Oh JK, Jeon ES (2013) Predictors of left ventricular reverse remodeling and subsequent outcome in nonischemic dilated cardiomyopathy. Circ J 77:462–469
JCS Joint Working Group (2013) Guidelines for treatment of acute heart failure (JCS 2011). Circ J 77:2157–2201
Ikeda Y, Inomata T, Iida Y, Iwamoto-Ishida M, Nabeta T, Ishii S, Sato T, Yanagisawa T, Mizutani T, Naruke T, Koitabashi T, Takeuchi I, Nishii M, Ako J (2015) Time course of left ventricular reverse remodeling in response to pharmacotherapy: clinical implication for heart failure prognosis in patients with idiopathic dilated cardiomyopathy. Heart Vessels. doi:10.1007/s00380-015-0648-2
Tsukada B, Terasaki F, Shimomura H, Otsuka K, Otsuka K, Katashima T, Fujita S, Imanaka-Yoshida K, Yoshida T, Hiroe M, Kitaura Y (2009) High prevalence of chronic myocarditis in dilated cardiomyopathy referred for left ventriculoplasty: expression of tenascin C as a possible marker for inflammation. Hum Pathol 40:1015–1022
Vasiljević JD, Otasević P, Popović ZB, Nesković AN, Vidaković R, Popović ZV, Radovancević B, Frazier OH, Gradinac S (2005) Semiquantitative histomorphometric analysis of myocardium following partial left ventriculectomy: 1-year follow-up. Eur J Heart Fail 7:763–767
Writing Committee Members, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128:e240–e327
Schwarz F, Mall G, Zebe H, Blickle J, Derks H, Manthey J, Kübler W (1983) Quantitative morphologic findings of the myocardium in idiopathic dilated cardiomyopathy. Am J Cardiol 51:501–506
Rose AG, Beck W (1985) Dilated (congestive) cardiomyopathy: a syndrome of severe cardiac dysfunction with remarkably few morphological features of myocardial damage. Histopathology 9:367–379
Shimura S, Matsui Y, Yutani C, Suto Y, Akashi O, Matsui K, Shingu Y, Sakakibara M, Yamaguchi M, Haruki Y, Takigami K, Minase T, Ueda T (2009) Histopathological study of specimens obtained by left ventricular biopsy during ventriculoplasty for idiopathic dilated cardiomyopathy. Tokai J Exp Clin Med 34:1–7
Yamada T, Fukunami M, Ohmori M, Iwakura K, Kumagai K, Kondoh N, Kondoh N, Minamino T, Tsujimura E, Nagareda T, Kotoh K (1993) Which subgroup of patients with dilated cardiomyopathy would benefit from long-term beta-blocker therapy? A histologic viewpoint. J Am Coll Cardiol 21:628–633
Yamada Y, Saito S, Nishinaka T, Yamazaki K (2012) Myocardial size and fibrosis changes during left ventricular assist device support. ASAIO J 58:402–406
Kawai K, Takaoka H, Hata K, Yokoya Y, Yokoyama M (1999) Prevalence, predictors, and prognosis of reversal of maladaptive remodeling with intensive medical therapy in idiopathic dilated cardiomyopathy. Am J Cardiol 84:671–676
Bruckner BA, Stetson SJ, Perez-Verdia A, Youker KA, Radovancevic B, Connelly JH, Koerner MM, Entman ME, Frazier OH, Noon GP, Torre-Amione G (2001) Regression of fibrosis and hypertrophy in failing myocardium following mechanical circulatory support. J Heart Lung Transplant 20:457–464
Kubanek M, Sramko M, Maluskova J, Kautznerova D, Weichet J, Lupinek P, Vrbska J, Malek I, Kautzner J (2013) Novel predictors of left ventricular reverse remodeling in individuals with recent-onset dilated cardiomyopathy. J Am Coll Cardiol 61:54–63
Boehmer JP, Starling RC, Cooper LT, Torre-Amione G, Wittstein I, Dec GW, Markham DW, Zucker MJ, Gorcsan J 3rd, McTiernan C, Kip K, McNamara DM, Investigators IMAC (2012) Left ventricular assist device support and myocardial recovery in recent onset cardiomyopathy. J Card Fail 18:755–761
Delnoij T, van Suylen RJ, Cleutjens JP, Schalla S, Bekkers SC (2009) In vivo histology by cardiovascular magnetic resonance imaging. Eur Heart J 30:2492
Nabeta T, Inomata T, Iida Y, Ikeda Y, Iwamoto M, Ishii S, Sato T, Watanabe I, Naruke T, Shinagawa H, Koitabashi T, Takeuchi I, Nishii M, Inoue Y, Izumi T (2014) Baseline cardiac magnetic resonance imaging versus baseline endomyocardial biopsy for the prediction of left ventricular reverse remodeling and prognosis in response to therapy in patients with idiopathic dilated cardiomyopathy. Heart Vessels 29:784–792
Schalla S, Bekkers SC, Dennert R, van Suylen RJ, Waltenberger J, Crijns HJ, Heymans S (2010) Replacement and reactive myocardial fibrosis in idiopathic dilated cardiomyopathy: comparison of magnetic resonance imaging with right ventricular biopsy. Eur J Heart Fail 12:227–231
Wu KC, Weiss RG, Thiemann DR, Kitagawa K, Schmidt A, Dalal D, Lai S, Bluemke DA, Gerstenblith G, Marbán E, Tomaselli GF, Lima JA (2008) Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 51:2414–2421
Jellis C, Martin J, Narula J, Marwick TH (2010) Assessment of nonischemic myocardial fibrosis. J Am Coll Cardiol 56:89–97
Masci PG, Schuurman R, Andrea B, Ripoli A, Coceani M, Chiappino S, Todiere G, Srebot V, Passino C, Aquaro GD, Emdin M, Lombardi M (2013) Myocardial fibrosis as a key determinant of left ventricular remodeling in idiopathic dilated cardiomyopathy: a contrast-enhanced cardiovascular magnetic study. Circ Cardiovasc Imaging 6:790–799
Suwa M, Otake Y, Moriguchi A, Ito T, Hirota Y, Kawamura K, Adachi I, Narabayashi I (1997) Iodine-123 metaiodobenzylguanidine myocardial scintigraphy for prediction of response to beta-blocker therapy in patients with dilated cardiomyopathy. Am Heart J 133:353–358
Noda S (1980) Histopathology of endomyocardial biopsies from patients with idiopathic cardiomyopathy; quantitative evaluation based on multivariate statistical analysis. Jpn Circ J 44:95–116
Dick MR, Unverferth DV, Baba N (1982) The pattern of myocardial degeneration in nonischemic congestive cardiomyopathy. Hum Pathol 13:740–744
Baroldi G (1988) Anatomy and quantification of myocardial cell death. Methods Achiev Exp Pathol 13:87–113
Turillazzi E, Baroldi G, Silver MD, Parolini M, Pomara C, Fineschi V (2005) A systematic study of a myocardial lesion: colliquative myocytolysis. Int J Cardiol 104:152–157
Shimomura H, Terasaki F, Hayashi T, Kitaura Y, Isomura T, Suma H (2001) Autophagic degeneration as a possible mechanism of myocardial cell death in dilated cardiomyopathy. Jpn Circ J 65:965–968
Vigliano CA, Cabeza Meckert PM, Diez M, Favaloro LE, Cortés C, Fazzi L, Favaloro RR, Laguens RP (2011) Cardiomyocyte hypertrophy, oncosis, and autophagic vacuolization predict mortality in idiopathic dilated cardiomyopathy with advanced heart failure. J Am Coll Cardiol 57:1523–1531
Hoshikawa E, Matsumura Y, Kubo T, Okawa M, Yamasaki N, Kitaoka H, Furuno T, Takata J, Doi YL (2011) Effect of left ventricular reverse remodeling on long-term prognosis after therapy with angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and β blockers in patients with idiopathic dilated cardiomyopathy. Am J Cardiol 107:1065–1070
Unverferth DV, Fetters JK, Unverferth BJ, Leier CV, Magorien RD, Arn AR, Baker PB (1983) Human myocardial histologic characteristics in congestive heart failure. Circulation 68:1194–1200
Roberts WC, Ferrans VJ (1975) Pathologic anatomy of the cardiomyopathies. Idiopathic dilated and hypertrophic types, infiltrative types, and endomyocardial disease with and without eosinophilia. Hum Pathol 6:287–342
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose regarding this study.
Rights and permissions
About this article
Cite this article
Ishii, S., Inomata, T., Fujita, T. et al. Clinical significance of endomyocardial biopsy in conjunction with cardiac magnetic resonance imaging to predict left ventricular reverse remodeling in idiopathic dilated cardiomyopathy. Heart Vessels 31, 1960–1968 (2016). https://doi.org/10.1007/s00380-016-0815-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0815-0