Abstract
Inflammation activation is associated with adverse outcomes in patients with heart failure (HF). Sleep-disordered breathing (SDB) observed in 50% of patients with HF worsens the clinical outcome of HF, possibly through the exacerbation of inflammation. However, data on inflammation activation related to SDB are limited in patients with HF. We investigated the relationship between SDB severity and serum levels of C-reactive protein (CRP) and tumor necrotic factor (TNF)-α in HF patients with systolic dysfunction. Nineteen patients with HF were enrolled (mean age, 67.3 years; 16 men; mean ejection fraction, 33.6%). No significant correlation was observed between log-transformed CRP level and apnea–hypopnea index (AHI). In univariable analysis for serum CRP level, the percentage of rapid eye movement (REM) sleep per total sleep time was the only significant factor. The lower the percentage of REM sleep, the higher was the CRP level (coefficient, − 0.474; P = 0.047). In contrast, the serum TNF-α level was significantly correlated with age, ischemic etiology, diabetes mellitus, estimated glomerular filtration rate (eGFR), and AHI. In multivariable analysis, eGFR (coefficient, − 0.486; P = 0.017) and AHI (coefficient, 0.399; P = 0.044) significantly and independently correlated with TNF-α level. The severity of SDB expressed as AHI was directly related to the circulating level of TNF-α, but not circulating CRP level, in HF patients with systolic dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammation is associated with adverse outcomes in patients with heart failure (HF) [1, 2]. Studies have highlighted the close relationship between elevated levels of circulating inflammatory biomarkers and increased mortality and morbidity in patients with HF [3, 4]. HF condition activates inflammation [3, 5], which is further exacerbated by comorbidities such as sleep-disordered breathing (SDB). SDB, one of the common comorbidities in patients with HF (approximately 50% of HF patients exhibit SDB), enhances inflammation via frequent episodes of intermittent hypoxia/reoxygenation [6,7,8], possibly leading to the worsening of the HF condition [9, 10].
Although many studies in the non-HF population have revealed the relationship between elevated circulating inflammatory biomarkers and SDB, data on SDB-associated inflammation activation in patients with HF are limited. A previous study reported the weak relationship between circulating levels of C-reactive protein (CRP) and severity of SDB [11]. Therefore, we conducted a sub-analysis of our prospective pilot study in HF patients with left ventricular (LV) systolic dysfunction [12] to investigate the relationship between circulating inflammatory biomarkers (i.e., CRP and tumor necrotic factor [TNF]-α) and SDB severity. We hypothesize that the circulating level of CRP or TNF-α is directly associated with SDB severity in patients with HF.
Methods
Subjects
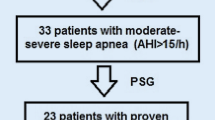
We enrolled patients with systolic HF at the Juntendo University Hospital (Tokyo, Japan) who met the following criteria: men and women aged ≥ 20 years; HF owing to ischemic or non-ischemic cardiomyopathy; left ventricular ejection fraction (LVEF) < 50% on echocardiography; New York Heart Association (NYHA) functional class ≥ II; and stable clinical status, as evident from the absence of symptoms related to the acute exacerbation of HF. Exclusion criteria were as follows: patients who failed to perform the 6-min walk test; those who could not answer questionnaire by themselves; current smokers; those with acute coronary syndrome and cardiac surgery during the previous 4 weeks; patients with treated SDB, organic valvular heart diseases, chronic inflammatory diseases, chronic lung diseases, and malignancy; those under dialysis. This is a sub-study of a prospective observational pilot study (UMIN 000014088), which was approved by the Juntendo University Hospital Institutional Review Board (#14-019). The study complied with the ethical principles of the Declaration of Helsinki [12]. Written informed consents were obtained from all participants.
Sleep study
All patients underwent overnight polysomnography using a digital polygraph system (Alice PDX; Philips Respironics, Murrysville, PA). Definitions and scoring methods were set as per the American Academy of Sleep Medicine manual version 2.2 [13]. Thoracoabdominal motion was monitored via respiratory inductance plethysmography, and air flow was measured using an oronasal thermal airflow sensor and a nasal pressure cannula. Oxyhemoglobin saturation (SO2) was monitored by oximetry. Apneas were classified as obstructive sleep apnea (OSA) or central sleep apnea (CSA) according to the presence or absence of thoracoabdominal motion, respectively. Hypopneas were classified as central in the absence of the following: snoring during the event, increased inspiratory flattening of the nasal pressure as compared with baseline breathing, and associated thoracoabdominal paradox during but not before the event [13]. Apneas and hypopneas were quantified, and SDB severity was assessed based on the frequency of apneas and hypopneas per hour of sleep (i.e., apnea–hypopnea index [AHI]). Obstructive and central AHI were separately computed, and the percentage of central AHI per total AHI was calculated. In addition, the number of desaturations (≥ 3% decrease in the saturation level) per hour of sleep (i.e., 3% oxygen desaturation index (ODI)) was computed. Polysomnography was scored by personnel blinded to the patients’ blood and urine test results.
Blood sampling and other data collection
Venous blood samples were obtained at morning after overnight fasting. The estimated glomerular filtration rate (eGFR) based on serum creatinine level, [14] serum CRP level, and serum TNF-α level were determined using commercially available human Quantikine HS enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, Minneapolis, USA). In addition, the plasma level of B-type natriuretic peptide (BNP) was assessed.
Height and weight were measured at morning to calculate body mass index (BMI). Blood pressure (BP) and heart rate were measured at the same time. Cardiac chamber quantification using two-dimensional echocardiography was performed according to the American Society of Echocardiography guidelines [15]. LVEF was calculated as per the modified Simpson method. All echocardiographic studies were performed and interpreted by experienced cardiologists who were blinded to the clinical data. The protocol for the 6-min walk test has been described elsewhere [16]. The total distance walked in 6 min (6MWD) was measured and assessed. Subjective sleepiness was evaluated by the Epworth sleepiness scale (ESS) [17].
Statistical analysis
As the original study was conducted as a pilot study, we did not calculate specific sample size in this sub-study. Continuous variables were expressed as mean ± standard deviation (SD) upon normal distribution of data or as median (interquartile range) in case of non-normally distributed data, unless otherwise indicated. Nominal variables were expressed as numbers and proportions. A univariable regression analysis was performed with CRP or TNF-α levels as dependent variables and the following independent variables: age, sex, BMI, etiology of LV systolic dysfunction (ischemic or nonischemic), NYHA class (class II or III/IV), presence or absence of diabetes, use of drugs, systolic and diastolic BP, heart rate, eGFR, BNP level, LVEF, ESS score, sleep study parameters (total sleep time, percentage of slow wave sleep per total sleep time, percentage of rapid eye movement [REM] sleep per total sleep time, arousal index, AHI including total, central, and obstructive, percentage of central respiratory events per total AHI, 3%ODI, time spent at below 90% SO2, and mean and minimum SO2). Variables with P < 0.05 in two separate univariate analyses were evaluated in a multivariate stepwise regression analysis for CRP and TNF-α levels. In the regression analysis, BNP level, ESS score, CRP level, percentage of slow wave sleep, and time spent below 90% SO2 were subjected to natural log-transformation owing to the non-normal distribution of the data. In cases when the data contained zero values, natural log-transformation using the formula Ln_X = log (X + 0.01) was performed [18]. A value of P < 0.05 indicated statistical significance. Analyses were performed using SPSS 23.0 (IBM Corp., Armonk, NY, USA).
Results
Patient characteristics
Overall, the data of 19 patients were used for the analysis. The characteristics of these patients, including 16 men and 3 women, are summarized in Table 1. Most patients were elderly and non-obese, and had HF with NYHA class II symptoms. Half of the patients had ischemic etiology, and all of them had an AHI ≥ 5 events/h. Most patients had severe SDB. Sleep study findings are shown in Table 2.
Relationship between inflammatory biomarkers and other variables
No significant correlation was observed between the log-transformed CRP levels and total AHI (Fig. 1). In the univariable analysis based on serum CRP levels, the percentage of REM sleep per total sleep time was the only significant factor that correlated with the log-transformed CRP levels; at a lower percentage of REM sleep, the CRP levels were higher (Table 3). As only a single variable exhibited significant correlation in the univariable analysis, no multivariable analysis was performed. In contrast, the serum TNF-α levels correlated significantly with age, ischemic etiology, diabetes mellitus, eGFR, and 3%ODI (Table 3), along with total AHI (Fig. 2). To avoid the issue of collinearity between 3%ODI and total AHI, separate multivariable analyses were conducted. In the multivariable analysis including total AHI, the final model included eGFR (coefficient, − 0.486; P = 0.017) and AHI (coefficient, 0.399; P = 0.044). In the multivariable analysis including 3%ODI, the final model included eGFR (coefficient, − 0.477; P = 0.016) and total AHI (coefficient, 0.435; P = 0.025).
Discussion
The present study provides a novel insight into the relationship between inflammation and SDB in patients with HF. We showed that the circulating level of CRP had no correlation with the severity of SDB. Furthermore, a significant correlation was observed between circulating TNF-α level and SDB severity even in the multivariable analysis. In addition to the severity of SDB, eGFR, the variable indicative of renal functions, significantly correlated with TNF-α level. These observations show that the elevated circulating inflammatory biomarker in HF patients with systolic dysfunction was associated with SDB severity and renal function but not with cardiac function. Such a relationship was observed with the serum TNF-α level but not with the serum CRP level.
SDB is associated with the activation of the inflammation process possibly through the intermittent hypoxia and sympathetic nerve activation [6, 7, 19,20,21]. Several studies have demonstrated the increased levels of inflammatory markers such as CRP and TNF-α in non-HF patients with SDB [8, 22, 23]. Furthermore, some studies have reported the decrease in CRP and TNF-α levels following specific treatment for SDB [24, 25], suggestive of the causal relationship between SDB and elevated CRP and TNF-α levels. However, the data on the elevation in the circulating CRP level in patients with HF and its association with SDB are scarce. Schmalgemeier and colleagues studied 966 patients with HF and reported significant association between SDB severity and elevated CRP level. However, these authors reported a very weak correlation between AHI and CRP level (correlation coefficient, 0.138) [11], consistent with the results of the present study reporting no association between AHI and serum CRP level. Koyama and colleagues observed a strong significant correlation between AHI and CRP level in HF patients with SDB and reported a decrease in CRP level following treatment for SDB [26]. However, these authors did not take into account the effects of confounders on the relationship between AHI and CRP level. Therefore, the relationship between SDB severity and inflammatory biomarkers in patients with HF remains to be elucidated.
While we failed to observe any significant relationship between the serum levels of TNF-α and either obstructive or central AHI, the serum levels of TNF-α correlated significantly with total AHI. In addition, the correlation between TNF-α and total AHI remained significant in the multivariable analysis. Collectively, the frequency of respiratory events, irrespective of whether obstructive or central, is a critical aspect in the relationship between SDB and TNF-α. Conversely, reasons for discrepancies in the relationship of total AHI with CRP levels or with TNF-α levels remain unclear. However, we believe that the elevation in the circulating CRP level may be multifactorial and the contribution of each factor may be minor and insignificant, especially owing to the small sample size. Although some studies have reported the significant independent relationship between CRP and AHI in patients without HF [22, 25], others have suggested the association between CRP level and obesity if not AHI [27, 28]. In contrast, no data on TNF-α level in HF patients with SDB are available. Therefore, the importance and novelty of the present study is the significant relationship between TNF-α level and AHI observed in patients with HF. In addition, it should be noted that at 3%ODI, the frequency of intermittent hypoxia/reoxygenation independently correlated with TNF-α levels, with similar, rather better correlation coefficient in the multivariable model in which 3%ODI was included instead of total AHI. This suggests that frequent episodes of intermittent hypoxia/oxygenation play an important role in the relationship between SDB and TNF-α levels even in patients with HF [7]. Other indices that enhance SDB severity, such as subjective sleepiness, degree of sleep disturbance, mean and minimum SO2, and time spent at below 90% SO2, exhibited no significant association with TNF-α levels in patients with SDB and HF. In a previous study by Vgontzas and colleagues, the relationship between sleepiness and inflammatory biomarkers was investigated in a non-HF population, and the primary factor influencing TNF-αl level was found to be degree of nocturnal sleep disturbance [29]. In the present study, however, we did not observe any relationship between sleepiness, degree of sleep disturbance, and TNF-α, probably owing to the specific features of sleep in HF patients; patients with HF, in general, have less sleep or sleeplessness as compared with those without HF and this phenomenon is independent of SDB [30]. Minoguchi and colleagues investigated the relationship between SDB severity and TNF-α level (both circulating level and that in monocytes) in a non-HF population, and found percentage of time spent below 90% SO2, rather than AHI, to be independently correlated with circulating and monocyte levels of TNF-α [23]. This observation may at least in part be explained by the mixture of CSA, wherein the hypoxic burden was generally lower than that in OSA [31]. The effects of time spent at below 90% SO2 on circulating or monocyte levels of TNF-α in patients with HF may be different from those observed in the general population, in which the mixture of CSA is rare.
We found a significant independent relationship between eGFR and TNF-α level; the lower the eGFR, the higher was the circulating level of TNF-α. This observation is consistent with several studies reporting elevated circulating TNF-α levels in patients with chronic kidney disease and the inverse relationship between eGFR and circulating TNF-α level in patients with HF [32, 33]. Furthermore, we found that the only factor correlating with elevated CRP level was lower percentage of REM sleep, consistent with the results of a recent study that reported the association between less REM sleep and higher CRP levels in Swedish women from the general population [34]. Although the causal relationship between REM sleep and CRP level and its effect remain controversial, the previous findings by Irwin and colleagues [35] revealed the reduced REM sleep following administration of interleukin-6—a well-known activator of CRP in the liver.
The present study has several limitations, including the small number of participants. Owing to this, the results of the present study do not provide a definitive conclusion regarding the relationship between inflammation and SDB in patients with HF. Therefore, future studies with a larger sample size are necessary to confirm the findings of this study. Second, as this was an observational cross-sectional study, the results do not prove the cause-and-effect relationship between SDB and TNF-α. One way to determine the existence of a cause-and-effect relationship between these factors is through an interventional trial for SDB. Finally, the ability to control confounders may be limited by the sample size. It is, therefore, possible that other unmeasured factors may have affected the relationship between SDB and TNF-α.
In conclusion, we show that the severity of SDB expressed as AHI in patients with HF is directly related to the circulating level of TNF-α but not circulating CRP level. These findings should be confirmed in a larger randomized controlled trial investigating whether any effective intervention for SDB may reduce the circulating level of TNF-α in patients with HF.
References
Deswal A, Petersen NJ, Feldman AM, Young JB, White BG, Mann DL. Cytokines and cytokine receptors in advanced heart failure: an analysis of the cytokine database from the Vesnarinone trial (VEST). Circulation. 2001;103:2055–9.
Murray DR, Freeman GL. Proinflammatory cytokines: predictors of a failing heart? Circulation. 2003;107:1460–2.
Chaikijurajai T, Tang WHW. Reappraisal of inflammatory biomarkers in heart failure. Curr Heart Fail Rep. 2020;17:9–19.
Matsumoto H, Kasai T, Sato A, Ishiwata S, Yatsu S, Shitara J, et al. Association between C-reactive protein levels at hospital admission and long-term mortality in patients with acute decompensated heart failure. Heart Vessels. 2019;34:1961–8.
Anker SD, von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004;90:464–70.
Kasai T, Floras JS, Bradley TD. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation. 2012;126:1495–510.
Kasai T. Sleep apnea and heart failure. J Cardiol. 2012;60:78–85.
Kasai T, Inoue K, Kumagai T, Kato M, Kawana F, Sagara M, et al. Plasma pentraxin3 and arterial stiffness in men with obstructive sleep apnea. Am J Hypertens. 2011;24:401–7.
Wu J, Stefaniak J, Hafner C, Schramel JP, Kaun C, Wojta J, et al. Intermittent hypoxia causes inflammation and injury to human adult cardiac myocytes. Anesth Analg. 2016;122:373–80.
Sano K, Watanabe E, Hayano J, Mieno Y, Sobue Y, Yamamoto M, et al. Central sleep apnoea and inflammation are independently associated with arrhythmia in patients with heart failure. Eur J Heart Fail. 2013;15:1003–100.
Schmalgemeier H, Bitter T, Fischbach T, Horstkotte D, Oldenburg O. C-reactive protein is elevated in heart failure patients with central sleep apnea and Cheyne-Stokes respiration. Respiration. 2014;87:113–20.
Kato T, Kasai T, Sato A, Ishiwata S, Yatsu S, Matsumoto H, et al. Effects of 3-month astaxanthin supplementation on cardiac function in heart failure patients with left ventricular systolic dysfunction—a pilot study. Nutrients. 2020;12:1896.
Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, et al. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.2. Darien: American Academy of Sleep Medicine; 2015.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–633.
Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–23.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5.
Haas DC, Foster GL, Nieto FJ, Redline S, Resnick HE, Robbins JA, et al. Age-dependent associations between sleep-disordered breathing and hypertension: importance of discriminating between systolic/diastolic hypertension and isolated systolic hypertension in the sleep heart health study. Circulation. 2005;111:614–21.
Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. 2005;112:2660–7.
Jelic S, Padeletti M, Kawut SM, Higgins C, Canfield SM, Onat D, et al. Inflammation, oxidative stress, and repair capacity of the vascular endothelium in obstructive sleep apnea. Circulation. 2008;117:2270–8.
Kasai T, Bradley TD. Obstructive sleep apnea and heart failure: pathophysiologic and therapeutic implications. J Am Coll Cardiol. 2011;57:119–27.
Shamsuzzaman AS, Winnicki M, Lanfranchi P, Wolk R, Kara T, Accurso V, et al. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation. 2002;105:2462–4.
Minoguchi K, Tazaki T, Yokoe T, Minoguchi H, Watanabe Y, Yamamoto M, et al. Elevated production of tumor necrosis factor-alpha by monocytes in patients with obstructive sleep apnea syndrome. Chest. 2004;126:1473–9.
De Santis S, Cambi J, Tatti P, Bellussi L, Passali D. Changes in ghrelin, leptin and pro-inflammatory cytokines after therapy in obstructive sleep apnea syndrome (OSAS) patients. Otolaryngol Pol. 2015;69:1–8.
Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation. 2003;107:1129–34.
Koyama T, Watanabe H, Kobukai Y, Makabe S, Munehisa Y, Iino K, et al. Beneficial effects of adaptive servo ventilation in patients with chronic heart failure. Circ J. 2010;74:2118–244.
Guilleminault C, Kirisoglu C, Ohayon MM. C-reactive protein and sleep-disordered breathing. Sleep. 2004;27:1507–11.
Taheri S, Austin D, Lin L, Nieto FJ, Young T, Mignot E. Correlates of serum C-reactive protein (CRP)–no association with sleep duration or sleep disordered breathing. Sleep. 2007;30:991–6.
Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab. 1997;82:1313–6.
Arzt M, Young T, Finn L, Skatrud JB, Ryan CM, Newton GE, et al. Sleepiness and sleep in patients with both systolic heart failure and obstructive sleep apnea. Arch Intern Med. 2006;166:1716–22.
Arzt M, Oldenburg O, Graml A, Erdmann E, Teschler H, Wegscheider K, et al. Phenotyping of sleep-disordered breathing in patients with chronic heart failure with reduced ejection fraction-the Schla HF registry. J Am Heart Assoc. 2017;6:e005899.
Pugliese NR, Fabiani I, Conte L, Nesti L, Masi S, Natali A, et al. Persistent congestion, renal dysfunction and inflammatory cytokines in acute heart failure: a prognosis study. J Cardiovasc Med (Hagerstown). 2020;21:494–502.
Putko BN, Wang Z, Lo J, Anderson T, Becher H, Dyck JR, et al. Circulating levels of tumor necrosis factor-alpha receptor 2 are increased in heart failure with preserved ejection fraction relative to heart failure with reduced ejection fraction: evidence for a divergence in pathophysiology. PLoS ONE. 2014;9:e99495.
Ghilotti F, Bellocco R, Trolle Lagerros Y, Thorson A, Theorell-Haglöw J, Åkerstedt T, Lindberg E. Sleep characteristics and markers of inflammation in Swedish women from the general population. J Sleep Res. 2020; e13093. https://doi.org/10.1111/jsr.13093.
Irwin MR. Sleep and inflammation: partners in sickness and in health. Nat Rev Immunol. 2019;19:702–15.
Funding
This study was supported by AstaReal Co., Ltd., and partly by a Grant-in-Aid for Scientific Research (Grant number, 26507010); JSPS KAKENHI (Grant number, JP17K09527); JSPS KAKENHI (Grant number, JP18K15904); a grant to The Intractable Respiratory Diseases and Pulmonary Hypertension Research Group from the Ministry of Health, Labor and Welfare (H29-027); and MEXT ∗ -Supported Program for the Strategic Research Foundation at Private Universities, 2014–2018 (∗ Ministry of Education, Culture, Sports, Science and Technology). These sources have no other roles in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Sato, Ishiwata, Matsue, Naito, and Kasai are affiliated to a department endowed by Philips, Fukuda Denshi, and ResMed. Dr. Daida received manuscript fees, research funds, and scholarship funds from Kirin Co. Ltd., Kaken Pharmaceutical Co. Ltd., Abbott Japan Co. Ltd., Astellas Pharma Inc., Astrazeneca K.K., Bayer Yakuhin Ltd., Boston Scientific Japan K.K., Bristol-Myers Squibb, Daiichi Sankyo Company, MSD K.K., Pfizer Inc., Philips, Sanofi K.K., and Takeda Pharmaceutical Co. Ltd. Other authors report no conflicts of interest.
Ethical Committee Permission
This study was approved by the Juntendo University Hospital Institutional Review Board (#14-019). This is a research involving Human Participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sato, A., Kato, T., Kasai, T. et al. Relationship between inflammatory biomarkers and sleep-disordered breathing in patients with heart failure. Sleep Biol. Rhythms 19, 55–61 (2021). https://doi.org/10.1007/s41105-020-00287-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-020-00287-5