Abstract
Although single-source 64-multislice computed tomography coronary angiography (SSCTA) needs to reduce heart rate (HR), dual-source computed tomography coronary angiography (DSCTA) can acquire images even in tachycardia. The accuracy of DSCTA during tachycardia is compared to the accuracy of SSCTA at reduced HR. Patients who received invasive coronary angiography and either SSCTA or DSCTA were included. In the SSCTA group, HR was reduced to <65 beats per minute (bpm) with β-blocker (n = 27), while in the DSCTA group patients whose HR was >65 bpm were selected (n = 27). The diagnostic accuracy for significant coronary stenosis was calculated by comparing the invasive coronary angiography. Using dual-Doppler echocardiography, isovolumic relaxation time (IRT) and diastasis time (DT) were evaluated in these patients. In SSCTA, sensitivity was 89 %, specificity 99 %, the positive predictive value (PPV) 94 %, and the negative predictive value (NPV) was 98 %. In DSCTA, sensitivity was 96 %, the specificity was 99 %, PPV was 91 %, and NPV was 99 % (all NS compared to SSCTA). When HR was >75 bpm, DT was markedly shortened (<83 ms), however IRT was maintained >85 ms. Thus, the image reconstruction at the phase of IRT is feasible in DSCTA because of its temporal resolution of 83 ms. High temporal resolution of DSCTA shows equivalent accuracy of coronary stenosis detection to SSCTA, without reducing heart rate, because of its image reconstruction at IRT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Several reports have shown that the single-source 64-multislice computed tomography coronary angiography (SSCTA) is useful for diagnosing coronary artery disease when the heart rate (HR) is reduced to < 65 beats per minute (bpm) [1–3]. Recently, SSCTA is used to characterize plaque morphology before coronary intervention [4, 5]. However, when the HR is >65 bpm, the image quality becomes deteriorated and the diagnostic accuracy is markedly reduced, because of the motion artifact [6, 7]. This is attributed to the temporal resolution of >165 ms for conventional SSCTA, which is determined by the gantry rotation speed. This temporal resolution is adequate for image reconstruction during the long diastolic period when the HR is low; however, once the HR exceeds more than 65 bpm, the diastasis period becomes shortened, and the image reconstruction at diastasis becomes unsuitable. This is the reason why β-blocker administration is essential for conventional SSCTA when the HR is >65 bpm [7–9]. Recently, dual-source computed tomography coronary angiography (DSCTA) has become available [10–12]. It has two sets of an X-ray tube and image intensifier, and the gantry rotation speed is equivalent to SSCTA. Thus, the temporal resolution becomes half of SSCTA, i.e., 83 ms. It has been known when the HR increased, diastasis time (DT) becomes abbreviated, but the isovolumic relaxation time (IRT) is maintained even in the high HR. If the IRT is maintained more than 83 ms when the HR exceeds 65 bpm, theoretically the image reconstruction at IRT is possible using DSCTA. However, it remained unknown whether the IRT is more than 83 ms at HR more than 65 bpm in patients of this study. Thus we first checked the IRT and DT of patients with variable HR. Recently, a comparative study between conventional SSCTA and DSCTA was reported [12]. This study showed the improved evaluability of DSCTA even in the high HR; however, the mechanism remains to be elucidated. This prompted us to compare the diagnostic accuracy of DSCTA at HR >65 bpm without β-blocker treatment to that of SSCTA at HR <65 bpm with β-blocker treatment if needed. Furthermore, we analyzed the optimal image reconstruction timing of DSCTA at higher HR. We evaluated the relationship between HR and IRT, or DT using dual Doppler echocardiography and compared them to the temporal resolution of DSCTA and SSCTA.
Materials and methods
The protocol of this study was approved by the Ethical Committee of Yamaguchi University Hospital, and conforms to the Declaration of Helsinki. All patients gave informed consent. Patients who received invasive coronary angiography (ICA) and either SSCTA or DSCTA were included (n = 114). Among these patients, 27 undertook SSCTA at an HR <65 bpm with β-blocker treatment if needed (metoprolol, 20 mg orally at 1.5 h before the examination). Patients (n = 27) were imaged with DSCTA at an HR >65 bpm without metoprolol treatment. Coronary artery stenoses in ICA were evaluated according to the American Heart Association (AHA) criteria [13] and the AHA criteria ≥75 % is considered a significant stenosis. The diagnosis on SSCTA and DSCTA were performed by three radiologists according to the AHA criteria. AHA criteria ≥75 % were considered a significant stenosis. The diagnostic accuracy for significant coronary stenosis by either SSCTA or DSCTA was evaluated in comparison to ICA as a reference standard. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated for all segments, except the following conditions: severe arrhythmias, e.g., atrial fibrillation and frequent ventricular premature contraction, segments with heavy calcification, segments <1.5 mm in diameter, stent implantation site, and the chronic total occlusion. To determine the optimal time of image reconstruction, the axial images were viewed and the timing when proximal portions of right coronary artery and left coronary artery were most clearly viewed without motion artifact was detected manually at around 75 % RR interval and at around 30–35 % RR interval, which corresponds to DT and IRT. By comparing images at DT and IRT, the optimal timing was determined whether it is DT or IRT. To elucidate the relationship between HR and IRT or DT, we measured IRT and DT in a separate 32 patients whose characteristics were compatible to the CTA study group by using dual Doppler echocardiography (Hitachi, Japan). Dual Doppler echocardiography enables the simultaneous measurement of aortic and mitral flow [14], which is suitable for measuring the IRT and DT in the same beat (Fig. 1a). As shown in Fig. 1a and b, the IRT was measured as the duration between the end of the aortic flow and the beginning of the mitral flow. The DT was defined as the duration between the end of rapid mitral filling and the beginning of atrial filling [15].
Scan protocol
SSCTA was performed with Somatom sensation (Siemens Medical Solutions, Erlangen, Germany). The tube voltage, gantry rotation time, number of slices per rotation, and the individual detector width were 120 kV, 330 ms, 32 × 2, and 0.6 mm, respectively. The tube current was 770 mA and the table feed speed was 0.2 mm/rotation. DSCTA was performed with Somatom Definition (Siemens Medical Solutions). The tube voltage, gantry rotation time, number of slices per rotation, and the individual detector width were same as SSCTA. The tube current was 400 mA and the table feed speed was 0.2–0.4 mm/rotation. All patients received one puff of nitroglycerine spray (0.3 mg glyceryl trinitrate; Toa Eiyo, Tokyo, Japan) 5 min before the imaging. The iohexol 350 (Omnipaque 350; Schering AG, Germany) was injected at a rate of 4.0–5.0 ml/s depending on the body weight. The injection volume was calculated by the following equation: [(scan time + 3 s) × injection rate]. All patients received the contrast injection through the antecubital vein with a 22-G plastic needle. The bolus tracking technique was applied for SSCTA, while the test injection technique was applied for DSCTA. A 30-ml saline chaser was administered after the contrast injection. Image reconstruction and analysis was performed on a dedicated workstation (Ziostation; AMIN Inc., Tokyo, Japan).
Statistical analysis
The patients’ backgrounds were compared between SSCTA and DSCTA using the unpaired t test. The sensitivity, specificity, PPV, and NPV for the detection of significant coronary stenosis (≥75 %) were compared between SSCTA and DSCTA using the Chi-square test (StatView 5.0; SAS Institute Inc, Cary, NC, USA). p values <0.05 were considered statistically significant.
Results
The patients’ characteristics are shown in Table 1. None of the parameters were statistically different between the groups, except HR (p < 0.01). Seven patients (26 %) received β-blocker treatment in the SSCTA group, while none received β-blocker treatment in the DSCTA group. Approximately 50 % of the patients in both groups had a high calcium score >400 (Table 1 [16]). The average injected contrast volume was 61 ± 3.6 for SSCTA and 56.5 ± 13.0 ml for DSCTA (NS).
Diagnostic accuracy between SSCTA and DSCTA
In the SSCTA group, 376 out of 459 coronary segments were evaluable (81.9 %), and 348 out of 459 segments were evaluable in the DSCTA group (75.8 %, NS). The per-segment sensitivity was 89.4 % (34 of 38) by SSCTA and 96.6 % (29 of 30, NS) by DSCTA. The specificity was 99.4 % (336 of 338) for SSCTA and 99.0 % for DSCTA (315 of 318, NS), the PPV was 94.4 % (34 of 36) for SSCTA and 90.6 % (29 of 32, NS) for DSCTA, the NPV was 98.8 % (336 of 340) for SSCTA and 99.6 % (315 of 316, NS) for DSCTA, and accuracy was 98.4 % (370 of 376) for SSCTA and 98.8 % (344 of 348, NS) for DSCTA (Table 2). None of the parameters were statistically significant between SSCTA and DSCTA.
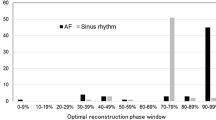
Optimal reconstruction timing
The optimal image reconstruction timing of SSCTA are all DT. However, as shown in Fig. 2, more than 50 % of patients in the DSCTA group were reconstructed at IRT. Especially, when the HR was >80 bpm, 100 % of the patients were reconstructed at IRT (Fig. 2).
The relationship between HR and IRT or DT
The relationship between HR and IRT or DT is shown in Figs. 3 and 4. The patients were divided into four groups depending on their HR: <60, 60–65, 65–70, and >75. The average HR of each group was 53.0 ± 4.4, 63.2 ± 1.6, 71.4 ± 3.2, and 82.3 ± 8.8, respectively. IRT was not significantly different among the four groups, and the averaged IRT of all patients was 103.2 ± 23.7 ms. Conversely, DT was significantly shortened according to the increase of the HR. When the HR was >65 bpm, DT becomes <165 ms. When the HR becomes >75 bpm, DT was shortened to <83 ms.
Discussion
The diagnostic accuracy of SSCTA has been reported to be excellent when the HR is <65 bpm [6–9]; however, when the HR exceeds 65 bpm, the evaluability of SSCTA is reduced from 93 to 69 % [12]. This is the reason why β-blocker pre-treatment is essential when the HR is >65 bpm for SSCTA. Recently, DSCTA is available, which equipped two imaging systems on a single gantry. Thus, the temporal resolution of DSCTA is 83 ms, which is half the temporal resolution of SSCTA, 165 ms. Because of the high temporal resolution, DSCTA has been reported to show an excellent diagnostic accuracy even in the high HR [10–12]. However, the detailed comparison between SSCTA with lower HR and DSCTA at higher HR had remained to be done. Our study is the first to demonstrate the equivalent diagnostic accuracy of the significant coronary stenosis between SSCTA with lower HR and DSCTA with higher HR. Thus, our results gave a rationale for DSCTA without β-blocker pre-treatment even in the high HR. Our results coincide with the data reported by Achenbach et al. [12], but their study did not assess the relationship between the HR and optimal reconstruction timing. Our study demonstrates that the optimal reconstruction timing of DSCTA shifted from the DT to IRT. Especially, we showed that 100 % of the patients showed optimal reconstruction timing at IRT when the HR is >80 bpm. We further clarify the relationship between HR and IRT or DT. Our data showed that IRT is constantly >83 ms, even at HR >75 bpm in the patients with suspected coronary artery disease. This indicates that the image reconstruction is feasible at IRT because of the short temporal resolution of 83 ms with DSCTA. On the other hand, DT was abbreviated remarkably to <83 ms when the HR becomes >75 bpm (Fig. 4). This indicates that even with DSCTA, DT is not long enough for image reconstruction when the HR becomes more than 75 bpm. The temporal resolution of SSCTA is 165 ms, which exceeds the IRT at any HR; thus, image reconstruction at IRT is impossible even in lower HR with SSCTA. The only optimal reconstruction phase for SSCTA is at DT when the HR is less than 65 bpm. Physiologically, the heart pauses momentarily during the isovolumic contraction phase, IRT, and DT [14, 15]. Among these periods, DT is usually longer than the other periods when the HR is low. However, DT is shortened dramatically when the HR increases, as shown in Fig. 4. When the HR is <65 bpm, DT is >165 ms. However, when the HR exceeds 65 bpm, DT becomes less than 165 ms. The isovolumic contraction time is usually <80 ms, which is less than the temporal resolution of DSCTA. IRT is always >83 ms, even in high HR (Fig. 4). Thus, IRT becomes the target period for image reconstruction [16–18]. We demonstrate for the first time that the temporal resolution of DSCTA (83 ms) enables image reconstruction at IRT and gave a theoretical background of the avoidance of β-blocker pre-medication. This study will promote the imaging of emergency cases and outpatient clinic for screening coronary artery disease in chest pain patients. However, β-blocker should be administered carefully to patients with vasospastic angina pectoris [19], bronchial asthma, chronic obstructive lung disease, and heart block. We need to consider a pitfall for DSCTA at high heart rate. The image is reconstructed at end-systolic phase, muscle squeezing resembles coronary narrowing [20]. This can be differentially diagnosed by considering the over-riding of epicardial muscle on the coronary artery. Finally, coronary calcification is still a big problem for diagnosing coronary stenosis even using DSCTA. As shown by a previous study, a higher calcium score relates more to a coronary stenotic lesion [21]. In our study, patients with a calcium score >400 exceeds more than 50 % in both SSCTA and DSCTA groups and not significantly different. Thus, the high calcium score does not influence the conclusions made in this study.
Conclusions
DSCTA can diagnose coronary artery disease without β-blocker pre-medication because temporal resolution of DSCT is less than IRT.
References
Mollet NR, Cademartiri F, van Mieghem CA, Runza G, McFadden EP, Baks T, Serruys PW, Krestin GP, de Feyter PJ (2005) High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112:2318–2823
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46:552–557
Ehara M, Surmely JF, Kawai M, Katoh O, Matsubara T, Terashima M, Tsuchikane E, Kinoshita Y, Suzuki T, Ito T, Takeda Y, Nasu K, Tanaka N, Murata A, Suzuki Y, Sato K, Suzuki T (2006) Diagnostic accuracy of 64-slice computed tomography for detecting angiographically significant coronary artery stenosis in an unselected consecutive patient population: comparison with conventional invasive angiography. Circ J 70:564–571
Utsunomiya D, Fukunaga T, Oda S, Awai K, Nakaura T, Urata J, Yamashita Y (2011) Multidetector computed tomography evaluation of coronary plaque morphology in patients with stable angina. Heart Vessels 26:392–398
Harigaya H, Motoyama S, Sarai M, Inoue K, Hara T, Okumura M, Naruse H, Ishii J, Hishida H, Ozaki Y (2011) Prediction of the no-reflow phenomenon during percutaneous coronary intervention using coronary computed tomography angiography. Heart Vessels 26:363–369
Leber AW, Knez A, von Zieler F, Becker A, Nikolaou K, Paul S, Wintersperger B, Reiser M, Becker CR, Steinbeck G, Boekstegers P (2005) Quantification of obstructive and non-obstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Ropers D, Rixe J, Anders K, Küttner A, Baum U, Bautz W, Daniel WG, Achenbach S (2006) Usefulness of multidetector row spiral computed tomography with 64- × 0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenosis. Am J Cardiol 97:343–348
Pugliese F, Mollet NR, Runza G, van Mieghem C, Meijboom WB, Malagutti P, Baks T, Krestin GP, deFeyter PJ, Cademartiri F (2006) Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol 16:575–582
Nagatani Y, Takahashi M, Takazakura R, Nitta N, Murata K, Ushio N, Matsuo S, Yamamoto T, Horie M (2007) Multidetector-row computed tomography coronary angiography-optimization of image reconstruction phase according to the heart rate. Circ J 71:112–121
Ropers U, Ropers D, Pflederer T, Anders K, Kuettner A, Stilianakis NI, Komatsu S, Kalender W, Bauts W, Daniel WG, Achenbach S (2007) Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J Am Coll Cardiol 50:2393–2398
Johnson TR, Nikolaou K, Busch S, Leber AW, Becker A, Wintersperger BJ, Rist C, Knez A, Reiser MF, Becker CR (2007) Diagnostic accuracy of dual-source computed tomography in the diagnosis of coronary artery disease. Invest Radiol 10:684–691
Achenbach S, Ropers U, Kuettner A, Anders K, Pflederer T, Komatsu S, Bautz W, Daniel WG, Ropers D (2008) Randomized comparison of 64-slice single- and dual-source computed tomography coronary angiography for the detection of coronary artery disease. J Am Coll Cardiol Cardiovasc Imaging 1:177–186
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB (1975) A reporting system on patients evaluated for coronary artery disease. Report of the ad-hoc committee for grading of coronary artery disease, Council on Cardiovascular Surgery. Circulation 51:5–40
Duzenli MA, Ozdemir K, Aygul N, Soylu A, Aygul MU, Gok H (2009) Comparison of myocardial performance index obtained either by conventional echocardiography or tissue Doppler echocardiography in healthy subjects and patients with heart failure. Heart Vessels 24:8–15
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB (1995) New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function—a study in normals and dilated cardiomyopathy. J Cardiol 26:357–366
Brodoefel H, Burgstahler C, Tsiflikas I, Reimann A, Schroeder S, Claussen CD, Heuschmid M, Kopp AF (2008) Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology 247:346–355
Leschka S, Scheffel H, Desbiolles L, Plass A, Gaemperli O, Valenta I, Husmann L, Flohr TG, Genoni M, Marineck B, Kaufmann PA, Alkadhi H (2007) Image quality and reconstruction intervals of dual-source CT coronary angiography: recommendations for ECG-pulsing windowing. Invest Radiol 42:543–549
Isma’eel H, Hamirani YS, Mehrinfar R, Mao S, Ahmadi N, Larijani V, Nair S, Budoff MJ (2009) Optimal phase for coronary interpretations and correlation of ejection fraction using late-diastole and end-diastole imaging in cardiac computed tomography angiography: implications for prospective triggering. Int J Cardiovasc Imaging 25:739–749
Seo SM, Kim PJ, Shin DI, Kim TH, Kim CJ, Min JS, Koh YS, Park HJ, Kim DB, Her SH, Chang KY, Baek SH, Chung WS, Seung KB (2012) Persistent coronary artery spasm documented by follow-up coronary angiography in patients with symptomatic remission of variant angina. Heart Vessels. doi:10.1007/s00380-012-0249-2
Takamura K, Fujimoto S, Nanjo S, Nakanishi R, Hisatake S, Namiki A, Ishikawa Y, Ishii T, Yamazaki J (2011) Anatomical characteristics of myocardial bridge in patients with myocardial infarction by multi-detector computed tomography. Circ J 75:642–648
Ueda H, Harimoto K, Tomoyama S, Tamaru H, Miyawaki M, Mitsusada N, Yasuga Y, Hiraoka H (2012) Relation of cardiovascular risk factors and angina status to obstructive coronary artery disease according to categorical coronary artery calcium score. Heart Vessels 2:128–134
Acknowledgments
We thank Yuichi Sano, Shohei Kudomi, and Ryoko Tanabe for their excellent support during image analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujimura, T., Miura, T., Nao, T. et al. Dual-source computed tomography coronary angiography in patients with high heart rate. Heart Vessels 29, 443–448 (2014). https://doi.org/10.1007/s00380-013-0383-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-013-0383-5