Abstract
Although atrial natriuretic peptide (ANP) is widely used in patients with congestive heart failure (CHF), little is known about its effect on epicardial coronary arteries. Magnetic resonance imaging (MRI) enables precise measurement of coronary vasodilation and flow velocity. In this study, we examined the changes in epicardial coronary artery size and flow velocity in response to intravenous infusion of ANP or nitroglycerin (NTG) by using 3 T MRI in patients with CHF. The study cohort contained a total of 14 subjects: 8 patients with CHF and 6 healthy volunteers as controls, randomly divided into two groups: the ANP group (0.03 μg/kg/min) and the NTG group (0.3 μg/kg/min). Cross-sectional MR angiography and phase-contrast flow velocity of the right coronary artery in the same in-plane slice were obtained at the baseline, during drug infusion, and at two subsequent time points after stopping drug infusion. A significant increase was observed in the coronary cross-sectional area at 15 min after drug infusion in both groups compared with that at baseline; however, a late peak was observed at 15 min after stopping infusion in the ANP group. No significant differences were detected in the flow velocity in both groups. Furthermore, although NTG increased the heart rate, this change was not found in the ANP group. Coronary vasodilation and flow velocity can be measured simultaneously using 3 T MRI. Using this method, we showed that the effects of ANP on the coronary artery vasodilation and flow velocity were not inferior to those of NTG, with no significant alteration in heart rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite the development of effective medications during the past decade, congestive heart failure (CHF) remains the key cause of morbidity and mortality in the elderly worldwide [1]. Vasodilators such as nitroglycerin (NTG) or atrial natriuretic peptide (ANP) are widely used in patients with CHF caused by ischemic or nonischemic heart disease [2]. Despite the prompt and beneficial hemodynamic effect of NTG, this agent may stimulate the renin–angiotensin–aldosterone system (RAAS) and cause tachycardia. Moreover, long-term administration of NTG leads to impaired vasodilation, a phenomenon known as NTG tolerance [3, 4]. By contrast, ANP, a circulating hormone of cardiac organ, has vasodilatory and diuretic properties and suppresses the RAAS [5, 6]. In patients with CHF, ANP increased the cardiac index and stroke volume index, and significantly reduced pulmonary capillary wedge pressure and systemic vascular resistance [7]. However, there are limited data on epicardial coronary vasodilation caused by this agent in patients with CHF. Some previous studies using invasive coronary angiography (CAG) reported that ANP dilates the epicardial coronary artery in subjects with normal coronary arteries and normal ventricular function [8, 9].
The introduction of noninvasive techniques for measuring human epicardial coronary vasodilation directly would allow a widespread evaluation of coronary vasoreactivity. Coronary magnetic resonance angiography (MRA) has developed rapidly over the past decade. High-resolution coronary MRA can now achieve submillimeter spatial resolution by a variety of breath-hold and non-breath-hold techniques, making the measurement of coronary vasodilation feasible [10, 11]. This technique does not utilize ionizing radiation or contrast agents, making it particularly safe for serial measurements. Using this technique, Terashima et al. [12] reported a 23 % increase in coronary cross-sectional area (CSA) after sublingual NTG administration in patients with coronary artery disease and healthy subjects. Furthermore, magnetic resonance imaging (MRI) enables precise measurement of coronary blood flow velocity with a phase-contrast turbo gradient echo technique [13].
Although the efficacy of long-term administration of ANP to patients with CHF has been reported previously, little is known about the acute effect of this agent on epicardial coronary arteries in patients with CHF. The present study examines the changes in the epicardial coronary artery size and flow velocity in response to intravenous infusion of ANP or NTG by using 3 T MRI, in patients with CHF in the stable chronic phase and in healthy subjects.
Patients and methods
Patients
The study cohort contained a total of 14 subjects without contraindications to MRI: 8 patients with CHF due to idiopathic dilated cardiomyopathy (n = 4) or hypertensive heart disease (n = 4) who were enrolled from Osaka Social Medical Center, and 6 healthy volunteers as controls. All participants were men in the range of 31–72 years old (mean 49 ± 14 years) and in sinus rhythm. All patients with CHF showed clinically stable New York Heart Association (NYHA) functional class I/II symptoms. Each patient enrolled in the study met the following criteria: (1) normal sinus rhythm; (2) history of CHF within at least 6 months before the study; (3) no history of coronary artery disease, and no significant coronary artery stenoses with a lumen reduction of ≥50 % detected by CAG or multislice computed tomography coronary angiography. Patients were excluded from the study if they had primary valvular heart disease or any known cause of dilated cardiomyopathy. Patients continued on maintenance medications, including diuretics and β-blockers. All vasodilators, including calcium-channel blockers, angiotensin-converting enzyme inhibitors, or angiotensin II type 1 receptor blockers, were withheld for more than 24 h before the study. No patient was on nitrates treatment. Among the healthy volunteers, none had known cardiovascular disease, hypercholesterolemia, and diabetes mellitus, and two patients had a history of hypertension. These two hypertensive patients were stage I according to the criteria established by the Joint National Committee VII; no patient was using antihypertensive medication. All participants were in the fasting state for at least 6 h before the study. Patients and controls were randomly divided into two groups: the ANP group (4 patients with CHF and 4 controls) and the NTG group (4 patients with CHF and 2 controls). The study was approved by the hospital ethical committee (Osaka Social Medical Center), and informed consent was obtained from all participants before the study.
Acquisition of MRI data
Coronary MRI was performed by using a 3.0 T MRI unit (Achieva; Philips Medical Systems, Best, the Netherlands) with a 6-channel cardiac coil. First, free-breathing turbo gradient echo whole-heart coronary MRA images were acquired [14–16]. In brief, initial survey images were focused around the heart, and the reference images were then obtained for sensitivity of parallel imaging. Transaxial cine MR images were then acquired using a steady-state free precession sequence while breathing freely (repetition time, 2.6 ms; echo time, 1.3 ms; flip angle, 60°; field of view, 320 × 320 × 120 mm; acquisition matrix, 128 × 128; cardiac phases, 100; SENSE factor, 3.0 in the anteroposterior direction; imaging time, 3 s) to determine the trigger delay time when the motion of the right coronary artery (RCA) is minimum. Patient-specific acquisition windows were set during either the diastolic or the systolic phase, depending on the phase of minimal motion of the RCA. Coronary MRA was performed while patients were free-breathing by using a three-dimensional, segmented k-space turbo gradient echo sequence with T2 preparation and radial k-space sampling in Y–Z plane (repetition time 4.5 ms, echo time 2.1 ms, flip angle 20°, number of excitations 1, navigator gating window of ±2.0 mm with diaphragm drift correction, field of view 320 × 320 mm, acquisition matrix 256 × 256, reconstruction matrix 512 × 512, resulting in an acquired spatial resolution of 1.25 × 1.25 × 1.6 mm reconstructed to 0.625 × 0.625 × 0.8 mm). Diaphragm drift due to irregular respiration was corrected automatically by the diaphragm drift correction system attached to the MR system.
For quantitative analysis of coronary vasodilation and flow velocity, the cross-sectional RCA images were used. For that purpose, cross sections perpendicular to the linear portion of the proximal to mid-RCA obtained from whole-heart coronary MRA images, using double-oblique technique, were determined (Fig. 1). Then, multiple (typically eight) contiguous high-resolution cross-sectional images were acquired with a segmented turbo gradient echo sequence during free breathing with a right hemidiaphragm navigator (repetition time 3.7 ms, echo time 1.3 ms, flip angle 20°, number of excitations 3, navigator gating window of ± 2.0 mm with diaphragm drift correction, field of view 200 × 200 mm, acquisition matrix 224 × 224, reconstruction matrix 512 × 512, resulting in an acquired spatial resolution of 0.89 × 0.89 × 2.5 mm reconstructed to 0.39 × 0.39 × 2.5 mm).
Coronary magnetic resonance angiography (MRA) images of the right coronary artery (RCA) for the quantitative analysis of coronary vasodilation. a Whole-heart coronary MRA image shows the linear portion of the proximal to mid-RCA. b Cross sections perpendicular to the linear portion of the proximal to mid-RCA obtained from the whole-heart coronary MRA image are determined
Then, to measure coronary flow velocity, a segmented k-space phase-contrast turbo gradient echo sequence with symmetric bipolar gradient during breath-holding (repetition time 5.9 ms, echo time 3.7 ms, flip angle 10°, velocity encoding 50 cm/s, number of excitations 2, field of view 200 × 200 mm, acquisition matrix 128 × 128, reconstruction matrix 256 × 256, resulting in an acquired spatial resolution of 1.56 × 1.56 × 6.0 mm reconstructed to 0.78 × 0.78 × 6.0 mm) was used [13].
MRI data analysis
The reconstructed data were transferred to a workstation (Virtual Place; AZE, Tokyo, Japan) for postprocessing. As described above, the cross-sectional RCA images were used for quantitative analysis of coronary vasodilation. The slice with the most circular cross section was identified on the baseline (predrug infusion) images. The corresponding slices (during drug infusion, and 15 and 30 min after stopping infusion) were carefully matched according to the surrounding cardiac and chest wall structures. Then all the images were pooled and randomized, and no patient information was provided on the images. All MR images were analyzed by the same cardiologist who was unaware of patients’ clinical data. Images were magnified twofold, and CSAs of the RCA were manually traced.
We then measured the peak coronary flow velocity of the RCA. Regions of interest with an area of 2 × 2 pixels were placed in the center of the vessel on the flow images for each cardiac phase. The average flow velocity (cm/s) of this region of interest was determined for each phase. The highest value was used for the determination of peak flow velocity (Fig. 2) [13]. To evaluate interobserver and intraobserver variabilities, two independent observers determined the CSAs and peak flow velocity of 20 randomly selected images, and the same observer repeated the examination after 1 week. Both observers were cardiologists with 3 years of experience in cardiac imaging, and they were blinded to each other’s results and to clinical data.
Magnetic resonance phase-contrast coronary flow images of the RCA for the quantitative analysis of coronary flow velocity. a Regions of interest were placed in the center of the vessel on the flow images for each cardiac phase. b The average flow velocity (cm/s) of this region of interest was determined for each phase. The highest value was used for the determination of peak flow velocity
Study protocol
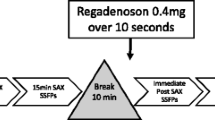
Subjects were placed in supine position in the magnet with surface coil placed over the anterior chest. All subjects underwent continuous heart rate and vector electrocardiographic monitoring, and their blood pressure was measured every 5 min. After placement of catheters into bilateral cubital veins, a 15-min period was allowed for hemodynamic stabilization. First, whole-heart coronary MRA images were acquired. Subsequently, baseline cross-sectional coronary MRA scans (eight slices) and coronary blood flow velocity with a phase-contrast turbo gradient echo technique were obtained. ANP (Carperitide; Daiichi-Sankyo, Tokyo, Japan) was prepared by dissolving it in 5 % glucose solution, and NTG (Millisrol; Nippon Kayaku, Tokyo, Japan) was diluted in saline. After obtaining baseline images, ANP or NTG infusion was started at a rate of 0.03 μg/kg/min (the ANP group) or 0.3 μg/kg/min (the NTG group) over 15 min via a cubital vein by an infusion pump, according to the previous report [9]. We then performed cross-sectional coronary MRA and determined the phase-contrast blood flow velocity in the same in-plane slice during drug infusion for 15 min and at two subsequent time points after stopping drug infusion (15 and 30 min after stopping infusion). At each point (baseline, during drug infusion, 15 min after stopping infusion, 30 min after stopping infusion), blood pressure and heart rates were recorded and blood samples were withdrawn from the opposite cubital vein of drug infusion. The study protocol is shown in Fig. 3.
Plasma samples and determination of plasma levels of ANP, renin, and aldosterone
To evaluate changes in plasma levels of ANP, renin, and aldosterone, blood samples were withdrawn at each step of the image acquisition. Blood samples for the assay of plasma ANP were collected in tubes containing ethylenediamine tetraacetic acid and aprotinin (3000 U), and those for renin and aldosterone were collected in tubes containing EDTA/2Na. These blood samples were immediately centrifuged at 3000 × g for 15 min at 4 °C. The plasma was then carefully removed and immediately stored at −20 °C until further assay. Plasma levels of ANP, renin, and aldosterone were measured at BML (Saitama, Japan).
Statistical analysis
The results were expressed as mean ± standard deviation (SD). Statistical analysis comparing the two groups was performed with unpaired two-tailed Student’s t test or with Mann–Whitney test when the variance was heterogeneous. Statistical comparisons among the three groups were performed by one-way analysis of variance (ANOVA) and post hoc multiple comparisons using Fisher’s test. Time-course data were analyzed with two-way repeated-measures ANOVA. If the global tests showed a significant difference, Fisher’s test for multiple comparisons was performed for data collected over a long period of time. Categorical variables were compared by Fisher’s exact test. Intraobserver and interobserver variability were analyzed by calculating both the percentage of the absolute difference between the two measurements divided by the mean of the measurements as well as the correlation coefficient. P values of less than 0.05 were considered statistically significant.
Results
Baseline characteristics
The characteristics of patients and control subjects are shown in Table 1. Patients with CHF were significantly older than control subjects (P < 0.0001). The average ejection fraction in patients with CHF was 35 ± 7 %. The medications before study were as follows: β-blockers (7 patients), calcium-channel blockers (2 patients), and angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers (3 patients).
Effect of ANP or NTG infusion on hemodynamic and neurohumoral variables
All subjects completed the study without any complications. As shown in Table 2, intravenous infusion of ANP and NTG decreased systolic blood pressure slightly but not significantly (P = 0.437). The heart rate was unchanged after ANP infusion, but NTG caused a statistically significant increase in heart rate (P < 0.05).
The ANP group showed a significant increase in plasma ANP levels at 15 min after ANP infusion compared with that at the baseline, and a subsequent decrease from 15 min after stopping ANP infusion; further, plasma ANP levels returned to those at the baseline by 30 min after stopping ANP infusion (ANP group: baseline, 32 ± 26; during drug infusion, 482 ± 124; 15 min after stopping infusion, 67 ± 31; 30 min after stopping infusion, 44 ± 33 pg/ml; ANOVA, P < 0.0001). The increase in plasma ANP levels did not differ between patients with CHF and controls. However, the NTG group did not show an increase in plasma ANP levels during the study. Plasma renin and aldosterone levels and aldosterone/renin ratio were not significantly changed in both the ANP and NTG groups.
Effects of either ANP or NTG on epicardial coronary vasodilation and peak flow velocity
The coronary area measurements had an intraobserver variability of 2.5 % ± 1.3 %, with a correlation of 0.99, and an interobserver variability of 4.7 % ± 1.9 %, with a correlation of 0.99. Regarding peak flow velocity, the intraobserver variability was 2.2 % ± 1.7 %, with a correlation of 0.99, and the interobserver variability was 3.5 % ± 1.8 %, with a correlation of 0.99. The time course of the coronary CSA and the peak flow velocity responses to either ANP or NTG infusion are shown in Table 3. Because of large individual variations in both the values (see SD in Table 3), the values were calculated as percentage changes from the baseline (the ratio of the CSA or peak flow velocity at the point during drug infusion and at the subsequent two time points after stopping drug infusion to those at baseline). The percentage changes in CSA and peak flow velocity are shown in Fig. 4. In the NTG group, a significant increase in CSA was observed at 15 min after NTG infusion compared with that at baseline, and a subsequent decrease from 15 min after stopping NTG infusion onward (during drug infusion, 1.25 ± 0.10; 15 min after stopping infusion, 1.17 ± 0.09; 30 min after stopping infusion, 1.10 ± 0.07; compared with the baseline, ANOVA: P < 0.0001). However, a late increase in CSA was observed in the ANP group at 15 min after stopping ANP infusion, and a subsequent decrease from 30 min after stopping ANP infusion (during drug infusion, 1.15 ± 0.09; 15 min after stopping infusion, 1.23 ± 0.10; 30 min after stopping infusion, 1.17 ± 0.08; compared with the baseline, ANOVA: P < 0.0001). However, the peak ratio of CSA did not differ between the NTG and ANP groups. By contrast, no significant differences were found in the time course of the peak flow velocity, although there was a trend of decreasing velocity after drug infusion in both the NTG (ANOVA, P = 0.687) and ANP (ANOVA, P = 0.292) groups. The representative coronary cross-sectional images at each point (baseline, during drug infusion, 15 min after stopping infusion, and 30 min after stopping infusion) for each patient infused with either ANP or NTG are shown in Fig. 5.
Representative coronary cross-sectional images at each point (baseline, during drug infusion, 15 min after stopping infusion, and 30 min after stopping infusion) in each patient infused with either ANP or NTG. Cross-sectional images of the ANP group are shown in the upper panel, and those of the NTG group in the lower panel
Discussion
To the best of our knowledge, this is the first study to investigate the changes in the epicardial coronary artery size and flow velocity in response to intravenous infusion of ANP or NTG by using coronary 3 T MRI, in patients with CHF in the stable chronic phase and in healthy subjects. In both the ANP and NTG groups, significant increases in the coronary CSA were observed at 15 min after drug infusion compared with that at baseline, although a late peak at 15 min after stopping infusion was found in the ANP group. After stopping drug infusion, subsequent decreases in the CSA were also observed. By contrast, significant differences in the time course of the maximum flow velocity were not detected, although there was a trend of decreasing velocity after drug infusion in both groups. Furthermore, although NTG caused a statistically significant increase in the heart rate after infusion, the heart rate in the ANP group was unchanged during the study period.
Thus far, there have been several quantitative studies on epicardial coronary artery size and coronary blood flow in response to intravenous infusion of ANP using invasive CAG or Doppler flow catheters. Chu et al. [8] reported that bolus injection of ANP caused sustained proximal epicardial coronary dilation that did not increase further after a subsequent injection of NTG. Moreover, they showed that coronary flow was not significantly increased after ANP injection, indicating that the proximal coronary dilation was a direct effect induced by ANP and was not secondary to flow-mediated changes [8, 17]. Egashira et al. [9] also showed that a clinical dose of ANP by intravenous infusion dilated the epicardial coronary arteries and increased the estimated coronary blood flow despite no change in the flow velocity. However, their studies did not include patients with recent heart failure as well as healthy subjects, because the study population consisted of patients who were clinically judged as requiring invasive CAG. Nevertheless, our present findings, including those of patients with CHF, that intravenous infusion of ANP dilates the epicardial coronary artery and the effect of vasodilation induced by ANP is not inferior to that of NTG, are in agreement with the previous findings. However, the results of studies examining the effects of ANP on the coronary blood flow have been conflicting [8, 9, 18]. The different responses may have been influenced by different conditions and different protocols for ANP infusions.
The mechanism of the vasodilation effect of ANP is not fully understood. The vasodilating activities of ANP and NTG are endothelium independent, and these drugs are believed to stimulate guanylate cyclase in the cell membrane, resulting in increased intracellular cyclic guanosine monophosphate (cGMP) and relaxation of vascular smooth muscle cells [19–22]. ANP activates the particulate guanylate cyclase, while NTG activates soluble guanylate cyclase [23]. Chu et al. [8] reported that the time course of proximal coronary dilation was related more closely to the time course of increase in plasma cGMP level than to that of plasma ANP. Recently, it has been revealed that cGMP is generated by two different pathways: by stimulating nitric oxide synthase to generate nitric oxide and activate soluble guanylate cyclase, or by natriuretic peptide activation of particulate guanylate cyclase [24–26]. In the present study, discordance between the duration of epicardial coronary dilation and the duration of plasma ANP elevation was observed. Perhaps the direct effects of ANP on the epicardial coronary arteries were similar to those of nitrates, but developed more gradually and were not accompanied by significant changes in systemic hemodynamics. We believe that this finding would be a valuable link between the pharmacology of ANP or NTG and its clinical relevance.
There is a crucial and important clinical implication in the present study. A noninvasive assessment of coronary vasodilation and flow velocity with coronary MRI may be useful for investigating the serial changes of coronary function in response to various therapeutic interventions, in a different study population including healthy subjects. Furthermore, our method may have potential value in understanding the relationship between coronary vasodilation and coronary flow by using noninvasive MRI. In addition, MRI allows us to analyze not only coronary vasoreactivity but also left ventricular systolic and diastolic function [27, 28]. The combination of coronary artery vasodilation, blood flow, and left ventricular function visualized using MRI will be useful for determining the pathophysiological mechanisms of human heart disease.
Limitations
This study has several limitations. First, the number of patients with CHF included in this study was very small. In addition, we examined two kinds of disease (dilated cardiomyopathy and hypertensive heart disease) in patients with nonischemic heart failure. By contrast, our study population did not contain patients with coronary artery disease. It is unknown whether ANP can reduce ischemia by dilation of the stenotic epicardial coronary arteries, leading to favorable redistribution of flow to the ischemic subendocardium. Further studies are needed to assess the clinical efficacy of ANP as a coronary dilator in the treatment of coronary artery disease. Second, for quantitative analysis of coronary vasodilation, only the cross-sectional RCA images were used. RCA measurements by MRA have shown good reproducibility [12, 29]. Further improvements in coronary MRA should allow quantitative analysis of the left coronary artery. Finally, we were able to assess only the peak flow velocity, not the mean flow velocity. Therefore, the coronary flow volume could not be calculated in this study.
Conclusions
This study shows that in both the patients with CHF in the stable chronic phase and the healthy subjects, the effect of ANP on the epicardial coronary artery vasodilation was not inferior to those of NTG, with no significant alteration in heart rate. This noninvasive assessment of coronary vasodilation and flow velocity with coronary MRI appears to be a promising tool for investigating the serial changes of coronary function in response to various therapeutic interventions, in different study populations, including healthy subjects.
References
Jessup M, Brozena S (2003) Heart failure. N Engl J Med 348:2007–2018
Hattori H, Minami Y, Mizuno M, Yumino D, Hoshi H, Arashi H, Nuki T, Sashida Y, Higashitani M, Serizawa N, Yamada N, Yamaguchi J, Mori F, Shiga T, Hagiwara N (2012) Differences in hemodynamic responses between intravenous carperitide and nicorandil in patients with acute heart failure syndromes. Heart Vessels. doi:10.1007/s00380-012-0252-7
Dalal JJ, Parker JO (1984) Nitrate cross-tolerance: effect of sublingual isosorbide dinitrate and nitroglycerin during sustained nitrate therapy. Am J Cardiol 54:286–288
Henry PJ, Horowitz JD, Louis WJ (1989) Nitroglycerin-induced tolerance affects multiple sites in the organic nitrate bioconversion cascade. J Pharmacol Exp Ther 248:762–768
Levin ER, Gardner DG, Samson WK (1998) Natriuretic peptides. N Engl J Med 339:321–328
Schultz HD, Gardner DG, Deschepper CF, Coleridge HM, Coleridge JC (1988) Vagal C-fiber blockade abolishes sympathetic inhibition by atrial natriuretic factor. Am J Physiol 255:R6–R13
Cody RJ, Atlas SA, Laragh JH, Kubo SH, Covit AB, Ryman KS, Shaknovich A, Pondolfino K, Clark M, Camargo MJ, Scarborough RM, Lewicki JA (1986) Atrial natriuretic factor in normal subjects and heart failure patients. Plasma levels and renal, hormonal, and hemodynamic responses to peptide infusion. J Clin invest 78:1362–1374
Chu A, Morris KG, Kuehl WD, Cusma J, Navetta F, Cobb FR (1989) Effects of atrial natriuretic peptide on the coronary arterial vasculature in humans. Circulation 80:1627–1635
Egashira K, Inou T, Imaizumi T, Tomoike H, Takeshita A (1991) Effects of synthetic human atrial natriuretic peptide on the human coronary circulation in subjects with normal coronary arteries. Jpn Circ J 55:1050–1056
Dirksen MS, Lamb HJ, Doornbos J, Bax JJ, Jukema JW, de Roos A (2003) Coronary magnetic resonance angiography: technical developments and clinical applications. J Cardiovasc Magn Reson 5:365–386
Danias PG, Stuber M, Botnar RM, Kissinger KV, Yeon SB, Rofsky NM, Manning WJ (2003) Coronary MR angiography clinical applications and potential for imaging coronary artery disease. Magn Reson Imaging Clin N Am 11:81–99
Terashima M, Meyer CH, Keeffe BG, Putz EJ, de la Pena-Almaguer E, Yang PC, Hu BS, Nishimura DG, McConnell MV (2005) Noninvasive assessment of coronary vasodilation using magnetic resonance angiography. J Am Coll Cardiol 45:104–110
Nagel E, Thouet T, Klein C, Schalla S, Bornstedt A, Schnackenburg B, Hug J, Wellnhofer E, Fleck E (2003) Noninvasive determination of coronary blood flow velocity with cardiovascular magnetic resonance in patients after stent deployment. Circulation 107:1738–1743
Sakuma H, Ichikawa Y, Chino S, Hirano T, Makino K, Takeda K (2006) Detection of coronary artery stenosis with whole-heart coronary magnetic resonance angiography. J Am Coll Cardiol 48:1946–1950
Kunimasa T, Sato Y, Matsumoto N, Chiku M, Tani S, Kasama S, Kunimoto S, Yoda S, Saito S, Nagao K (2009) Detection of coronary artery disease by free-breathing, whole heart coronary magnetic resonance angiography: our initial experience. Heart Vessels 24:429–433
Kato S, Kitagawa K, Ishida N, Ishida M, Nagata M, Ichikawa Y, Katahira K, Matsumoto Y, Seo K, Ochiai R, Kobayashi Y, Sakuma H (2010) Assessment of coronary artery disease using magnetic resonance coronary angiography: a national multicenter trial. J Am Coll Cardiol 56:983–991
Chu A, Cobb FR (1987) Effects of atrial natriuretic peptide on proximal epicardial coronary arteries and coronary blood flow in conscious dogs. Circ Res 61:485–491
Dubois-Rande JL, Adnot S, Benvenuti C, Merlet P, Hittinger L, Sediame S, Chabrier E, Braquet P, Castaigne A (1991) Hemodynamic response to intracoronary infusion of atrial natriuretic factor in patients with normal or altered left ventricular function. J Cardiovasc Pharmacol 17:608–614
Newman WH, Zhang LM, Castresana MR, Currie MG, Becker BF (1994) Correlation between vascular and cellular responses to atrial natriuretic peptide and to sodium nitroprusside. Life Sci 54:1351–1356
Murad F (1986) Cyclic guanosine monophosphate as a mediator of vasodilation. J Clin Invest 78:1–5
Waldman SA, Rapoport RM, Murad F (1984) Atrial natriuretic factor selectively activates particulate guanylate cyclase and elevates cyclic GMP in rat tissues. J Biol Chem 259:14332–14334
Matsumoto T, Okamura T, Kinoshita M, Toda N (1993) Interactions of nitrovasodilators and atrial natriuretic peptide in isolated dog coronary arteries. Eur J Pharmacology 237:31–37
Rapoport RM, Waldman SA, Schwartz K, Winquist RJ, Murad F (1985) Effects of atrial natriuretic factor, sodium nitroprusside, and acetylcholine on cyclic GMP levels and relaxation in rat aorta. Eur J Pharmacol 115:219–229
Derbyshire ER, Marletta MA (2012) Structure and regulation of soluble guanylate cyclase. Annu Rev Biochem 81:533–559
Potter LR (2011) Guanylyl cyclase structure, function and regulation. Cell Signal 23:1921–1926
Zhang M, Takimoto E, Lee DI, Santos CX, Nakamura T, Hsu S, Jiang A, Nagayama T, Bedja D, Yuan Y, Eaton P, Shah AM, Kass DA (2012) Pathological cardiac hypertrophy alters intracellular targeting of PDE5 from nitric oxide synthase-3 to natriuretic peptide signaling. Circulation. doi:10.1161/circulationaha.112.090977
Giannetta E, Isidori AM, Galea N, Carbone I, Mandosi E, Vizza CD, Naro F, Morano S, Fedele F, Lenzi A (2012) Chronic inhibition of cGMP phosphodiesterase 5A improves diabetic cardiomyopathy: a randomized, controlled clinical trial using magnetic resonance imaging with myocardial tagging. Circulation 125:2323–2333
Olimulder MA, Kraaier K, Galjee MA, Scholten MF, van Es J, Wagenaar LJ, van der Palen J, von Birgelen C (2012) Infarct tissue characteristics of patients with versus without early revascularization for acute myocardial infarction: a contrast-enhancement cardiovascular magnetic resonance imaging study. Heart Vessels 27:250–257
Keegan J, Horkaew P, Buchanan TJ, Smart TS, Yang GZ, Firmin DN (2004) Intra- and interstudy reproducibility of coronary artery diameter measurements in magnetic resonance coronary angiography. J Magn Reson Imaging 20:160–166
Acknowledgments
This work was supported by JSPS KAKENHI (23591057).
Conflict of interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ehara, S., Nakamura, Y., Matsumoto, K. et al. Effects of intravenous atrial natriuretic peptide and nitroglycerin on coronary vasodilation and flow velocity determined using 3 T magnetic resonance imaging in patients with nonischemic heart failure. Heart Vessels 28, 596–605 (2013). https://doi.org/10.1007/s00380-012-0292-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-012-0292-z