Abstract
The increased risk of cardiovascular morbidity and mortality among patients with sleep-disordered breathing (SDB) has been linked to arterial hypertension and insulin resistance. However, an effective antihypertensive agent for patients with SDB has not been identified. We investigated the effect of the angiotensin II subtype 1 receptor blocker olmesartan in hypertensive patients with SDB. This prospective, one-arm pilot study included 25 male patients with untreated SDB (mean age, 52.7 ± 11.4 years). We measured blood pressure, oxygen desaturation index (ODI), cardiac function using echocardiography, and insulin resistance using the homeostasis model assessment (HOMA) before and after 12 weeks of olmesartan therapy (mean dose, 17.6 ± 4.4 mg/day). Olmesartan significantly decreased systolic blood pressure (151.4 ± 8.0 vs 134.0 ± 7.4 mmHg; P < 0.001), diastolic blood pressure (93.4 ± 7.1 vs 83.9 ± 6.3 mmHg; P < 0.001), and HOMA index (3.7 ± 2.9 vs 2.8 ± 1.9; P = 0.012). Furthermore, left ventricular ejection fraction significantly increased at 12 weeks (68.1 ± 5.1 vs 71.6 ± 5.4%; P = 0.009). However, body mass index (BMI) and degree of SDB did not change (BMI, 26.6 ± 4.0 vs 26.6 ± 4.2 kg/m2, P = 0.129; 3% ODI, 29.5 ± 23.1 vs 28.2 ± 21.0 events/h, P = 0.394). Olmesartan significantly reduced blood pressure and insulin resistance in hypertensive patients with SDB without changing BMI or SDB severity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the early 1980s, sleep-disordered breathing (SDB) and the related clinical syndrome of sleep apnea have been associated with hypertension [1–4]. In patients with SDB, respiratory event-related intermittent hypoxia may lead to overactivation of the sympathetic nervous system and renin-angiotensin system (RAS), and the subsequent development of sustained increases in blood pressure [5, 6]. Sleep-disordered breathing is also associated with an increased risk of insulin resistance, type 2 diabetes, metabolic syndrome, and cardiac function [7–9]. However, there is insufficient evidence to suggest that a specific class of antihypertensive drugs should be used to control hypertension in patients with SDB.
None of the current hypertension guidelines address the use of antihypertensive agents in the treatment of hypertensive patients with SDB [10]. One study showed that in patients with obstructive sleep apnea (OSA), beta-blockers reduced blood pressure significantly more than calcium antagonists, diuretics, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin II subtype 1 receptors (ARB) [11]. By contrast, large-scale clinical trials have reported a significantly greater antihypertensive effect in hypertensive patients treated with an ARB compared with those taking beta-blockers [12, 13]. Because patients with SDB show enhanced RAS activity, drug therapy with RAS inhibitors might be useful in preventing subsequent organ damage. Olmesartan, an ARB, has been shown to lead to significantly greater reductions in blood pressure than other ARBs; it also has anti-inflammatory effects and reduces insulin resistance [14–18]. We investigated the effect of treatment with olmesartan in hypertensive patients with untreated SDB.
Methods
Patients
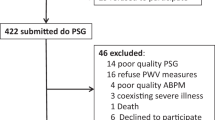
Patients who attended an outpatient clinic in the Sleep Center at the Toranomon Hospital for evaluation of SDB were prospectively screened for the study. Hypertensive patients from the outpatient clinic who had SDB were included in the present study. Other inclusion criteria were as follows: hypertensive patients who had withdrawn from continuous positive airway pressure (CPAP) treatment or had difficulties continuing CPAP treatment in the outpatient clinic, or hypertensive patients who could not be hospitalized for polysomnography in our hospital for a long period. Exclusion criteria were previous or current cardiovascular disease, pulmonary disorders, diabetes mellitus, chronic renal failure, wall motion abnormalities as determined by echocardiography, and receiving ACE inhibitors or ARBs. Arterial hypertension was defined as mean systolic blood pressure >140 mmHg and/or diastolic blood pressure >90 mmHg by mercury sphygmomanometer after at least 5 min of undisturbed rest in the sitting position, measured twice with an interval of 2 weeks. The assessment of disordered breathing during sleep was based on at least one overnight pulse oximetry. Informed consent was obtained from each patient. The protocol was approved by the institutional review board in our hospital, and the study was approved by the institutional ethics committee; all procedures were in accordance with institutional guidelines.
Study protocol
This was a prospective, single-center, before and after, pilot study. All patients were assigned to antihypertensive treatment with olmesartan for 12 weeks. Blood pressure was measured before and 4 and 12 weeks after treatment after a minimum of 5 min of undisturbed rest in the sitting position. For the purpose of consistency, conventional blood pressure measurements with mercury sphygmomanometers and appropriate cuff sizes were performed throughout the study. Blood pressure was measured in each patient by the same person at each visit. At least two measurements were made at each time point, and the mean values of these measurements were used. In addition, body mass index (BMI) and waist circumference were measured in the outpatient clinic before and 12 weeks after treatment.
Patients initially received either 10 or 20 mg olmesartan daily; the higher dose was used if systolic blood pressure was >150 mmHg or diastolic blood pressure was >100 mmHg. After 4 weeks, if systolic blood pressure was >140 mmHg or diastolic blood pressure was >90 mmHg, we increased the dose of olmesartan to 20 mg if the patient was already receiving 10 mg olmesartan or added diuretics (2 mg trichlormethiazide daily) if the patient was already receiving 20 mg olmesartan. In addition, if systolic blood pressure was <110 mmHg after 4 weeks, the dose was halved to 10 mg olmesartan if the patient was receiving 20 mg olmesartan or 5 mg olmesartan if the patient was receiving 10 mg olmesartan.
Evaluation of sleep-disordered breathing
We diagnosed SDB using pulse oximetry during one night of sleep at home. Assessments were made using the oxygen desaturation index (ODI), which measures oxygen desaturation per hour. A 3% ODI was selected as an index of oxygen desaturation, representing the number of events per hour of recording time in which blood oxygen fell ≥3%. A 3% ODI threshold recorded during an estimated sleep duration of more than 4 h was used for the analysis. Because the duration of sleep estimated by pulse oximetry is often longer than the actual total sleep time, we had subjects fill out a sleep diary in order to exclude waking time from the analysis and thereby minimize potential overestimation of sleep duration. We defined significant SDB as 3% ODI levels greater than 15 events per hour [4]. Other usually derived indexes of arterial oxygen saturation (SaO2), such as lowest SaO2 and cumulative time spent below 90% SaO2, were also calculated before and after 12 weeks of treatment. The degree of sleepiness was assessed by the Epworth Sleepiness Scale (ESS) [19] before and after 12 weeks of treatment. The ESS is a simple questionnaire measuring the general level of daytime sleepiness.
Blood tests and echocardiography
Blood samples were obtained before and 12 weeks after treatment. Serum blood glucose, insulin levels, C-peptide levels, and lipid profiles (total cholesterol, high-density lipoprotein cholesterol [HDL-C], low-density lipoprotein cholesterol [LDL-C], and triglycerides) were determined in the fasting state. The homeostasis model assessment for insulin resistance (HOMA-IR) was calculated as: HOMA-IR = fasting blood glucose × insulin/405.
We evaluated cardiac function using standard echocardiography methods. To obtain the chamber quantification using M-mode echocardiograms, the maximum minor axis of the left ventricle at end-diastole and end-systole was measured on the parasternal long-axis or short-axis view [20]. Left ventricular ejection fraction was calculated using the formula of Teichholz [21].
Statistical analysis
Continuous variables are expressed as mean ± SD. To compare demographic and laboratory parameters before and after treatment, we used the Wilcoxon rank-sum test for continuous variables. Analysis of variance was used to compare changes in blood pressure from baseline to 4 and 12 weeks. Post hoc Tukey HSD tests were used to compare parameters within groups. A two-sided P value of less than 0.05 was considered significant. All data were analyzed using JMP version 7.0 for Windows (SAS Institute, Cary, NC, USA).
Results
We enrolled 25 male patients (mean age, 52.7 ± 11.4 years) from January 2008 to December 2008. Baseline and follow-up clinical characteristics are shown in Table 1. Six patients (24%) were receiving hepatic hydroxymethyl glutaryl-CoA reductase inhibitors, 3 (12%) were receiving aspirin, 2 (8%) were receiving diuretics, and 5 (20%) were receiving calcium channel blockers. These drugs and their dosages were maintained throughout the study.
Blood pressure and physical characteristics
Olmesartan treatment (17.6 ± 4.4 mg/day) resulted in a significant decrease of systolic and diastolic blood pressure after 4 weeks (systolic blood pressure, 151.3 ± 7.9 to 139 ± 6.7 mmHg; diastolic blood pressure, 93.3 ± 7.0 to 87.5 ± 5.6 mmHg, P < 0.001 vs baseline for both comparisons). At 4 weeks, 3 patients were increased from 10 to 20 mg olmesartan, and 2 patients at 20 mg olmesartan received diuretics. Consequently, blood pressure showed significantly greater reductions at 12 weeks compared with 4 weeks (systolic blood pressure, 134.2 ± 7.3 mmHg; diastolic blood pressure, 83.6 ± 6.3 mmHg; P < 0.05 for both comparisons) (Fig. 1). On the other hand, BMI and waist circumference were not significantly changed after 12 weeks of treatment (26.6 ± 4.0 vs 26.6 ± 4.2 kg/m2, P = 0.129; 91.6 ± 10.0 vs 93.7 ± 15.2 cm, respectively, P = 0.612). No patient had their dose of olmesartan halved during the study. In addition, no patient experienced adverse effects during the study, based on patient reports and blood tests performed at 4 and 12 weeks.
Blood tests
Insulin resistance improved after olmesartan treatment. HOMA-IR was decreased from 3.7 ± 2.9 at baseline to 2.8 ± 1.9 at 12 weeks (P = 0.012) (Fig. 2). There was a tendency for fasting blood glucose to decrease from baseline to 12 weeks, but differences were not significant (108.0 ± 19.7 vs 102.0 ± 13.3 mg/dL, P = 0.310). Insulin levels decreased significantly from baseline to end of treatment (14.0 ± 10.9 vs 10.9 ± 7.6 mU/L, P = 0.004). C-peptide levels also decreased significantly from baseline to 12 weeks (3.3 ± 1.9 vs 2.6 ± 1.1 ng/mL, P = 0.023). On the other hand, there were no significant changes in total cholesterol, HDL-C, LDL-C, or triglyceride levels over 12 weeks.
SDB and cardiac function
There were no significant changes in the degree of SDB after olmesartan treatment (3% ODI, 29.5 ± 23.1 vs 28.2 ± 21.0 events/h, P = 0.394). Findings on pulse oximetry, including the lowest SaO2, percentage below 90%, and the ESS scores, did not change significantly. Results of echocardiography showed that systolic diameter was reduced after olmesartan treatment (30.3 ± 3.7 to 29.2 ± 3.8 mm, P = 0.019), whereas diastolic diameter was not significantly changed (49.3 ± 5.0 to 49.8 ± 5.0 mm, P = 0.594). Thus, ejection fraction was significantly increased after 12 weeks of treatment (68.1 ± 5.1 to 71.6 ± 5.4%, P = 0.009) (Table 2).
Discussion
Olmesartan significantly reduced blood pressure and improved insulin resistance in hypertensive patients with SDB. We believe the present study provides important information that can be used in the management of hypertension in patients with SDB.
Large cross-sectional studies have shown a relationship between SDB and hypertension that is not explained by potential confounding by age, sex, or obesity [22, 23]. Therefore, it is important to consider the presence of SDB in the management of hypertension in clinical practice. Evidence of a link between SDB and hypertension is provided by clinical trials of nasal CPAP, showing that this treatment lowers blood pressure in these patients [24, 25]. However, despite the positive aspects of CPAP, compliance can be difficult to achieve, as this treatment can cause nasal congestion, claustrophobic sensations, and other side effects. Adequate compliance with CPAP is being increasingly recognized as a major determinant of treatment success [26]. Thus, hypertensive patients with SDB who do not tolerate CPAP will remain at high risk for cardiovascular disease [27]. We think such patients should be considered high risk, and be treated with adequate and intensive treatment for blood pressure control. This study shows that olmesartan decreases blood pressure in patients with hypertension and SDB.
The present study also demonstrated that olmesartan treatment for 12 weeks improved insulin resistance in middle-aged Japanese men. The association between SDB and abnormal glucose metabolism (insulin resistance) has been investigated in several studies [28, 29]. Although increased insulin resistance has also been shown to be related to obesity, in multiple analyses the association between OSA and insulin resistance was independent of obesity [30, 31]. Furthermore, in a large prospective cohort study in Japan, Muraki et al. [32] recently reported that intermittent nocturnal hypoxia episodes during the night are associated with an increased risk for type 2 diabetes, independent of traditional risk factors for diabetes. Thus, early treatment intervention for both SDB and insulin resistance may help reduce the risk of diabetes in hypertensive patients. In our study, HOMA-IR was improved by olmesartan, although no improvements in SDB and BMI were seen. De Vinuesa et al. [18] also reported that treatment with olmesartan improves glucose metabolism and insulin sensitivity and decreases some inflammatory parameters in patients with renal disease, hypertension, and metabolic syndrome. Our results support the antimetabolic effects of olmesartan for hypertensive patients with SDB. It is not known whether this effect is shared by ARBs or is specific to olmesartan and independent of its angiotensin AT1 receptor-blocking activity [33]. In addition to changes in hemodynamic forces, additional mechanisms could be involved in the beneficial effects of olmesartan on insulin resistance because not all antihypertensive drugs improve insulin sensitivity [34]. In fact, diuretics and beta-blockers have been shown to worsen insulin sensitivity [35, 36]. In our results, insulin levels decreased significantly from baseline to 12 weeks. C-peptide is a pancreatic peptide of about 31 residues, depending on the species. Upon proteolytic cleavage of proinsulin, equimolar insulin and C-peptide are released. Therefore, we think the measurement of C-peptide is similar to the measurement of insulin. Measuring C-peptide in patients injecting insulin can help determine how much of their own natural insulin these patients are still producing. However, our study subjects did not include diabetic patients. Therefore, the changing levels of C-peptide might not have individual significance. In our results, there were similar changes in insulin and C-peptide levels before and after olmesartan treatment.
Moreover, it has been reported that patients with SDB have significantly higher levels of angiotensin II and aldosterone compared with healthy control subjects matched by body mass [37]. It is possible that the activation of the RAS is augmented by the presence of SDB and contributes to SDB-related hypertension. Therefore, we believe that olmesartan, an RAS inhibitor, is more effective than other classes of antihypertensive drugs for patients with hypertension and SDB. Pepin et al. [38] recently also reported the effect of ARB in hypertensive SDB patients in a randomized controlled trial. This report showed that valsartan, another ARB, induced a greater decrease in mean 24-h blood pressure than CPAP treatment, and the combination therapy of ARB and CPAP treatment was more effective. Thus, our results might further confirm the antihypertensive effects of an ARB in hypertensive SDB patients. We also consider RAS inhibition by olmesartan administration the effect of improvements in systemic vasoconstriction. As a result, we think afterload reduction induced by reduced systemic blood pressure influences the reduction of left ventricular wall stress. Moreover, this produces an increase in pump performance, as is seen from the effects on left ventricular systolic diameter and ejection fraction.
This study has several limitations. First, this was a small-scale, one-arm pilot study that included only 25 subjects. Large-scale, randomized controlled trials are needed to investigate the effects of olmesartan in comparison with other antihypertensive drugs. Second, we did not perform polysomnography to evaluate sleep quality. However, overnight pulse oximetry has been proposed as a simpler alternative to polysomnography in the diagnosis of OSA because it is readily available, relatively inexpensive, and could potentially meet the large demand for diagnostic testing in the community [39, 40]. Pulse oximetry can be easily done at home and repeated if need be, which is not the case with polysomnography. Therefore, we believe that overnight pulse oximetry was useful enough to evaluate SDB in daily clinical practice, particularly for the management of hypertensive patients. Third, we did not evaluate changes in blood pressure using ambulatory blood pressure monitoring (ABPM). We thought about assessing blood pressure using ABPM, as this method is more accurate than simple monitoring in SDB patients. In fact, BP levels normally vary during different physiologic states and decline by 10%–20% at night during sleep compared with daytime during wakefulness. A nocturnal blood pressure decrease less than 10% of daytime blood pressure is defined as “nondipping.” Nondipping has been shown in patients with clinically symptomatic OSA, regardless of hypertension status. Therefore, we consider further study is necessary to investigate the antihypertensive effect of olmesartan using ABPM to estimate the clinical implications regarding hypertension and SDB.
In conclusion, olmesartan, an ARB, significantly reduced blood pressure and insulin resistance in hypertensive patients with SDB without changing BMI or SDB severity. These results might be useful for managing hypertensive patients with SDB who are resistant to or unable to tolerate CPAP therapy.
References
Kales A (1984) Avoiding problems in the sleep laboratory. J Clin Psychopharmacol 4:14–16
Lavie P (1984) Nothing new under the moon. Historical accounts of sleep apnea syndrome. Arch Intern Med 144:2025–2028
Fletcher EC, DeBehnke RD, Lovoi MS, Gorin AB (1985) Undiagnosed sleep apnea in patients with essential hypertension. Ann Intern Med 103:190–195
Tanigawa T, Tachibana N, Yamagishi K, Muraki I, Kudo M, Ohira T, Kitamura A, Sato S, Shimamoto T, Iso H (2004) Relationship between sleep-disordered breathing and blood pressure levels in community-based samples of Japanese men. Hypertens Res 27:479–484
Fletcher A, van den Heuvel C, Dawson D (1999) Sleeping with an electric blanket: effects on core temperature, sleep, and melatonin in young adults. Sleep 22:313–318
Tamisier R, Gilmartin GS, Launois SH, Pepin JL, Nespoulet H, Thomas R, Levy P, Weiss JW (2009) A new model of chronic intermittent hypoxia in humans: effect on ventilation, sleep, and blood pressure. J Appl Physiol 107:17–24
Tasali E, Ip MS (2008) Obstructive sleep apnea and metabolic syndrome: alterations in glucose metabolism and inflammation. Proc Am Thorac Soc 5:207–217
Varol E, Akcay S, Ozaydin M, Ozturk O, Cerci SS, Sahin U (2010) Influence of obstructive sleep apnea on left ventricular mass and global function: sleep apnea and myocardial performance index. Heart Vessels 25:400–404
Maeno K, Kasai A, Setsuda M, Nishiyama A, Sakabe S, Ohnishi T, Saito K, Nishikawa H (2009) Advanced atrioventricular block induced by obstructive sleep apnea before oxygen desaturation. Heart Vessels 24:236–240
Baguet JP, Barone-Rochette G, Pepin JL (2009) Hypertension and obstructive sleep apnoea syndrome: current perspectives. J Hum Hypertens 23:431–443
Kraiczi H, Hedner J, Peker Y, Grote L (2000) Comparison of atenolol, amlodipine, enalapril, hydrochlorothiazide, and losartan for antihypertensive treatment in patients with obstructive sleep apnea. Am J Respir Crit Care Med 161:1423–1428
Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, Fyhrquist F, Ibsen H, Kristiansson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS, Omvik P, Oparil S, Wedel H (2002) Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 359:995–1003
Jordan J, Engeli S, Boschmann M, Weidinger G, Luft FC, Sharma AM, Kreuzberg U (2005) Hemodynamic and metabolic responses to valsartan and atenolol in obese hypertensive patients. J Hypertens 23:2313–2318
Oparil S, Williams D, Chrysant SG, Marbury TC, Neutel J (2001) Comparative efficacy of olmesartan, losartan, valsartan, and irbesartan in the control of essential hypertension. J Clin Hypertens (Greenwich) 3:283–291, 318
Smith DH, Dubiel R, Jones M (2005) Use of 24-hour ambulatory blood pressure monitoring to assess antihypertensive efficacy: a comparison of olmesartan medoxomil, losartan potassium, valsartan, and irbesartan. Am J Cardiovasc Drugs 5:41–50
Brunner HR, Arakawa K (2006) Antihypertensive efficacy of olmesartan medoxomil and candesartan cilexetil in achieving 24-hour blood pressure reductions and ambulatory blood pressure goals. Clin Drug Investig 26:185–193
Fliser D, Buchholz K, Haller H (2004) Antiinflammatory effects of angiotensin II subtype 1 receptor blockade in hypertensive patients with microinflammation. Circulation 110:1103–1107
de Vinuesa SG, Goicoechea M, Kanter J, Puerta M, Cachofeiro V, Lahera V, Gomez-Campdera F, Luno J (2006) Insulin resistance, inflammatory biomarkers, and adipokines in patients with chronic kidney disease: effects of angiotensin II blockade. J Am Soc Nephrol 17:S206–S212
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Teichholz LE, Kreulen T, Herman MV, Gorlin R (1976) Problems in echocardiographic volume determinations: echocardiographic–angiographic correlations in the presence of absence of asynergy. Am J Cardiol 37:7–11
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283:1829–1836
Young T, Peppard P, Palta M, Hla KM, Finn L, Morgan B, Skatrud J (1997) Population-based study of sleep-disordered breathing as a risk factor for hypertension. Arch Intern Med 157:1746–1752
Giles TL, Lasserson TJ, Smith BJ, White J, Wright J, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 3:CD001106
Bazzano LA, Khan Z, Reynolds K, He J (2007) Effect of nocturnal nasal continuous positive airway pressure on blood pressure in obstructive sleep apnea. Hypertension 50:417–423
Campos-Rodriguez F, Pena-Grinan N, Reyes-Nunez N, De la Cruz-Moron I, Perez-Ronchel J, De la Vega-Gallardo F, Fernandez-Palacin A (2005) Mortality in obstructive sleep apnea-hypopnea patients treated with positive airway pressure. Chest 128:624–633
Kario K (2009) Obstructive sleep apnea syndrome and hypertension: mechanism of the linkage and 24-h blood pressure control. Hypertens Res 32:537–541
Lattimore JD, Celermajer DS, Wilcox I (2003) Obstructive sleep apnea and cardiovascular disease. J Am Coll Cardiol 41:1429–1437
Pack AI (2006) Advances in sleep-disordered breathing. Am J Respir Crit Care Med 173:7–15
Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS (2002) Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med 165:670–676
Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL (2002) Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med 165:677–682
Muraki I, Tanigawa T, Yamagishi K, Sakurai S, Ohira T, Imano H, Kitamura A, Kiyama M, Sato S, Shimamoto T, Konishi M, Iso H (2010) Nocturnal intermittent hypoxia and the development of type 2 diabetes: the Circulatory Risk in Communities Study (CIRCS). Diabetologia 53:481–488
Berne C, Pollare T, Lithell H (1991) Effects of antihypertensive treatment on insulin sensitivity with special reference to ACE inhibitors. Diabetes Care 14(Suppl 4):39–47
Jacob S, Rett K, Henriksen EJ (1998) Antihypertensive therapy and insulin sensitivity: do we have to redefine the role of beta-blocking agents? Am J Hypertens 11:1258–1265
Lithell HO (1991) Effect of antihypertensive drugs on insulin, glucose, and lipid metabolism. Diabetes Care 14:203–209
Sowers JR, Bakris GL (2000) Antihypertensive therapy and the risk of type 2 diabetes mellitus. N Engl J Med 342:969–970
Moller DS, Lind P, Strunge B, Pedersen EB (2003) Abnormal vasoactive hormones and 24-hour blood pressure in obstructive sleep apnea. Am J Hypertens 16:274–280
Pepin JL, Tamisier R, Barone-Rochette G, Launois SH, Levy P, Baguet JP (2010) Comparison of continuous positive airway pressure and valsartan in hypertensive sleep apnea patients. Am J Respir Crit Care Med 182:954–960
Levy P, Pepin JL, Deschaux-Blanc C, Paramelle B, Brambilla C (1996) Accuracy of oximetry for detection of respiratory disturbances in sleep apnea syndrome. Chest 109:395–399
Epstein LJ, Dorlac GR (1998) Cost-effectiveness analysis of nocturnal oximetry as a method of screening for sleep apnea-hypopnea syndrome. Chest 113:97–103
Acknowledgments
The authors are grateful to the staff of the sleep center at Toranomon Hospital.
Conflict of interest
No author has any conflict of interest associated with this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dohi, T., Narui, K., Kasai, T. et al. Effects of olmesartan on blood pressure and insulin resistance in hypertensive patients with sleep-disordered breathing. Heart Vessels 26, 603–608 (2011). https://doi.org/10.1007/s00380-010-0104-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-010-0104-2