Abstract
Purpose
To compare the perioperative and functional outcomes of holmium laser enucleation of the prostate (HoLEP) and thulium laser enucleation of the prostate (ThuLEP) for the treatment of large-volume benign prostatic hyperplasia (BPH) (> 80 ml).
Methods
A total of 116 consecutive patients with BPH were randomized to be treated surgically with either HoLEP (n = 58) or ThuLEP (n = 58), following the classical three-lobe enucleation technique. Follow-up was assessed at 1, 3, 6, 12 and 18 months after surgery.
Results
At 18 months, the lower urinary tract symptom index was improved significantly in both groups compared with the baseline values. The operative time (78.4 ± 8.0 vs. 71.4 ± 6.4 min) and enucleation time (61.2 ± 5.4 vs. 56.4 ± 8.4 min) were significantly shorter for ThuLEP compared to HoLEP (both p < 0.001). There were no significant differences between the two groups regarding morcellation time, resected weight, hemoglobin decrease, catheter time and hospital stay (p > 0.05). The HoLEP and ThuLEP groups had equivalent International Prostate Symptom Scores (3 [3–3] vs. 3 [3–3], p = 0.776), quality of life (1 [1–2] vs. 2 [1–2], p = 0.809), Qmax (25.3 ± 4.8 ml/s vs. 24.7 ± 4.4 ml/s, p = 0.470), postvoid residual urine (PVR) (6.1 [2.6–20.8] vs. 7.7 [3.1–22.8] ml, p = 0.449) and PSA (0.84 ± 0.32 vs. 0.90 ± 0.34 ml, p = 0.309) at 18 months postoperatively.
Conclusion
Both HoLEP and ThuLEP relieve lower urinary tract symptoms in a comparable way with high efficacy and safety. ThuLEP was statistically superior to HoLEP in operation time and enucleation time, although the differences were clinically negligible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open prostatectomy (OP) is generally considered the gold standard for benign prostate hyperplasia (BPH) in large prostates [1]. Despite the overall good long-term results and the low reoperation rates after OP, the high perioperative morbidity associated with this approach stresses the need to find an adequate alternative that can reproduce the same functional results and drastically reduce morbidity [2].
Over the past decades, different laser systems for enucleation of the prostate have been successfully introduced, including holmium laser [3], thulium laser [4], green light laser [5], and diode laser [6]. Holmium laser enucleation of the prostate (HoLEP) has been proven to be a minimally invasive, size-independent method in numerous randomized controlled trials (RCTs) with excellent long-term results [3] and is recommended by the current guidelines of the European Association of Urology (EAU) in men with substantially enlarged prostates (e.g., > 80 ml) as the first choice [1].
Based on the HoLEP technique, Bach et al. first described the enucleation with the thulium laser, called ThuVEP, in 2009 [7], and Herrmann et al. proposed ThuLEP 1 year later [8]. The main difference between the two lasers is that holmium has a pulsed energy, while thulium emits a continuous laser wave [9]. ThuLEP may have several advantages over the holmium laser, including improved spatial beam quality and more precise tissue incision [10]. ThuLEP has been shown to be the technique that best fits all types of prostatic adenomas, giving optimal outcomes in terms of urinary symptom resolution and preservation of urinary continence and erectile function [11].
Herein, we present this randomized controlled trial to further investigate the possible differences in terms of intra- and postoperative variables, surgical complications, and outcomes of ThuLEP with HoLEP in patients with large-volume prostates (> 80 ml) during a medium-term 18-month follow-up.
Patients and methods
Study design and enrollment
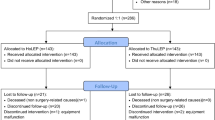
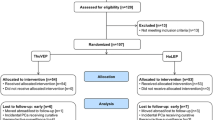
After receiving institutional review board approval, from March 2016 to September 2017, a total of 116 consecutive patients (Fig. 1) who suffered from BPH-related obstructed voiding symptoms with prostate volume > 80 ml, as determined by transrectal ultrasound (TRUS), were considered eligible for surgical treatment and enrolled in this RCT. Inclusion criteria were maximum urinary flow rate (Qmax) ≤ 15 ml/s, International Prostate Symptom Score (IPSS) ≥ 12, urodynamic obstruction without detrusor dysfunction and no response to pharmacologic therapy. The exclusion criteria were neurogenic bladder, findings suspicious for prostate cancer or urethral strictures, and poor tolerance for surgery. The study was approved by our ethics committee, and informed consent was obtained from all patients.
Randomization and preoperative assessments
The patients were randomized to be treated surgically with either HoLEP (n = 58) or ThuLEP (n = 58) by a computer-based prospective random sequence generator in a 1:1 ratio. Preoperative assessment included a physical examination with digital rectal examination (DRE), prostate-specific antigen (PSA), prostate volume by TRUS, uroflowmetry, postvoid residual urine (PVR) and by scoring of subjective symptoms with the IPSS and quality of life (QOL) questionnaires.
Interventions
The high-power pulsed 100-W VersaPulse holmium laser unit (Lumenis, Santa Clara, CA) was used for the HoLEP procedure, with an energy setting of 90 W for cutting and 20 W for coagulation. The thulium:YAG laser unit (Vela® XL, Boston Scientific, Ratingen, Germany) was used for the ThuLEP, with an energy setting of 120 W for cutting and 60 W for coagulation. A 26-F continuous-flow laser resectoscope (Karl Storz, Tuttlingen, Germany) in combination with a mechanical tissue morcellator (R. Wolf, Piranha™, Knittlingen, Germany) was used in both procedures.
All procedures were performed by two surgeons who had performed more than 300 HoLEP and 200 ThuLEP procedures both. Enucleation of the prostate using holmium:YAG and thulium:YAG is similar, and the three-lobe technique was usually performed in cases of large prostates. Following the initial depiction by Gilling [12] for HoLEP and Herrmann [8] for ThuLEP, enucleation was performed.
In brief, two incisions of the median lobe deep into the plane of the surgical capsule were progressively made at the 5- and 7-o’clock positions. Then the median lobe was enucleated following the margin of the prostatic capsule toward the verumontanum. Subsequently, an upper incision at 12 o’clock separated the lateral lobes, which were enucleated by joining the lower and upper resection planes of the lateral lobes. All enucleation was carried out while maintaining the sight of the surgical capsule. The enucleation was performed by bluntly exposing the plane of the adenoma and separating it from the capsule by means of laser energy. Physiological saline solution as irrigation fluid was used throughout the entire procedure. Morcellation was performed after completing the enucleation by means of a long nephroscope. A double inflow maintains safe bladder distension, avoiding injuries to the bladder wall. Following surgery, all patients had a Foley catheter with continuous bladder irrigation.
Data collection and follow-up
Perioperative data included the total operative time, enucleation time, morcellation time, resected weight, hemoglobin decrease, catheter time and hospital stay. All patients were reassessed 1, 3, 6, 12, and 18 months after surgery by IPSS, QoL, Qmax, PVR, and PSA. Perioperative and postoperative complications were reported according to the modified Clavien–Dindo system [13, 14].
Statistical analysis
The primary endpoint of the study was Qmax (ml/s) at 1 year postoperatively. The sample size was calculated for the detection of statistically significant differences. The calculation assumed that the relevant difference in Qmax would be 3 (SD = 5.5) ml/s. With α = 0.05 and a power of 80% (β = 0.20), a sample size of 53 patients per group was calculated. Assuming a 10% loss to follow-up over 1 year, we enrolled 58 patients in each group.
The secondary endpoints included Qmax at other time points after surgery, operative time, resected weight, hemoglobin decrease, catheter time and hospital stay. Postoperative variables included IPSS, QOL, PVR and PSA.
Statistical analysis was performed using SPSS 23 (IBM Corp, Armonk, NY, USA). Parametric continuous variables are expressed as mean ± standard deviation and were compared with the independent-sample t test. Nonparametric continuous variables are expressed as median and interquartile range and were analyzed with the Mann–Whitney U test or Wilcoxon matched-pairs signed rank test. Categorical variables were compared with the Chi-square test or Fisher’s exact probability test. For all statistical comparisons, a p value ≤ 0.05 was considered statistically significant.
Results
Baseline characteristics
Table 1 lists the baseline characteristics of the patients. There were no statistically significant differences in baseline characteristics between the HoLEP (n = 58) and ThuLEP groups (n = 58).
Perioperative results
Table 2 lists perioperative data. The operation was successful for all patients. The operative time (78.4 ± 8.0 vs. 71.4 ± 6.4 min) and enucleation time (61.2 ± 5.4 vs. 56.4 ± 8.4 min) were significantly longer for HoLEP compared to ThuLEP (both p < 0.001). There were no significant differences between the two groups regarding morcellation time, resected weight, hemoglobin decrease, catheter time or hospital stay.
Follow-up results
Table 3 lists the changes in IPSS, QoL, Qmax, PVR and PSA in 1, 3, 6, 12 and 18 months after the operation. There were no statistically significant differences between the two groups with respect to follow-up data (p > 0.05). Of the 116 patients, 107 completed the 18-month follow-up: 54 of 58 in the HoLEP group and 53 of 58 in the ThuLEP group. The reasons for dropouts were decision to withdraw by five patients and loss of contact by four patients.
Complications
Table 4 lists detailed information on all complications and treatment modalities. Slight postoperative hematuria was observed in three (5.2%) patients in the HoLEP group and one (1.7%) patient in the ThuLEP group, who all received prolonged bladder irrigation. After catheter removal, only one patient in the HoLEP group needed recatheterization because of urinary retention, while five (8.6%) patients in the HoLEP group and two (3.4%) patients in the ThuLEP group developed a self-limiting transient incontinence. Bladder mucosal injury was observed in four (6.9%) patients in the HoLEP group and one (1.7%) patient in the ThuLEP group. During the first 3 months of follow-up, four patients (one in the HoLEP group and three in the ThuLEP group) complained of urinary tract infection, but this resolved with sensitive antibiotics. In total, there was no significant difference in the first 3-month side effect rate between the HoLEP and ThuLEP groups (p = 0.147).
Within the observation periods of 12 months and 18 months, the complications included urethral stricture and bladder-neck contracture, which required internal urethrotomy or bladder-neck incisions. However, no significant differences were observed between the two groups.
Using the modified Clavien classification system (Table 5), minor complications requiring slight treatment occurred in 14 (24.1%) patients in the HoLEP group (Clavien 1: 22.4%; Clavien 2: 1.7%) and 7 (12.1%) patients in the ThuLEP group (Clavien 1: 6.9%; Clavien 2: 5.2%). Major complications requiring interventions occurred in two (3.4%) patients in the HoLEP group (Clavien 3a: 0; Clavien 3b: 3.4%) and two (3.4%) patients in the ThuLEP group (Clavien 3a: 0; Clavien 3b: 3.4%). No life-threatening complications occurred. There was no significant difference between the two groups in the occurrence of Clavien grade 1–3b complications.
Discussion
Laser enucleation of the prostate has developed as an efficient and minimally invasive method that may provide similar outcomes compared with TURP and OP [15]. Introduction of the holmium laser represented a turning point in minimally invasive laser therapy for BPH [16]. Newly emerging ThuLEP also showed comparable results to HoLEP, with the same efficacy and safety. Complications associated with these two techniques recorded within the intra- and perioperative period were mostly minor [17]. While long-term safety and efficiency for even large-volume prostates have been noted for HoLEP [2], evidence is still pending on the safety and efficiency of ThuLEP. Only Becker et al. recently reported the 48-month durability of ThuVEP for large-volume prostate [18]. Herein, we report the results of a RCT comparing ThuLEP with HoLEP in patients with large-volume prostates (> 80 ml) during an 18-month follow-up.
In our study, we observed a significant difference in operation time, which favored the ThuLEP technique. The difference in the energy setting might be a reasonable explanation. The HoLEP procedure was performed with an energy setting of 90 W for cutting and 20 W for coagulation. The ThuLEP procedure was performed with an energy setting of 120 W for cutting and 60 W for coagulation. A higher energy setting may result in faster enucleation speed and less operation time [19, 20]. The physical properties of the thulium laser may also play an important role. On the one hand, the wavelength of the thulium laser is closer to the water absorption peak compared with holmium laser, and water is the main absorbing substance, which comprises about two-thirds of the prostate, thus resulting in a high energy absorption rate and tissue vaporization even during enucleation [8, 21]. On the other hand, compared with the pulsed mode of the holmium:YAG laser, the continuous-wave mode of the thulium:YAG laser might provide a faster enucleation [22].
Several studies have reported that the overall PSA reduction could be a marker of complete removal of the adenoma [23, 24]. In our study, the mean decrease in PSA after HoLEP and ThuLEP at 18 months was 83.5 and 81.9%, respectively, which might be higher than the data reported in the literature [18, 25]. The more obvious PSA reduction in our study can be explained in part by the larger prostate size. In the study from Zhang and his colleagues [23], a mean PSA reduction of 71.3% and 77.2% was obtained in four HoLEP patients and five ThuLEP patients with a prostate 70 ml, while another two patients with a prostate 35 ml had a 24.2% and 26.1% PSA reduction. In the present study, all patients had a prostate over 80 ml, which might explain the result of PSA reduction.
HoLEP and ThuLEP are similarly associated with a high risk of postoperative ejaculatory dysfunction, especially retrograde ejaculation, which was an inevitable sequel of enucleation prostatectomy if the verumontanum was not spared [11, 26]. A recent study from Briganti and his colleagues reported that retrograde ejaculation was the major adverse event of men undergoing HoLEP, and the incidence of retrograde ejaculation was up to 78.3% [27]. Another study from Carmignani et al. reported that of the sexually active patients, 47.3% experienced retrograde ejaculation after ThuLEP [28]. However, in the present study, we failed to use the IIEF-5 questionnaire and calculate the rate of retrograde ejaculation during the follow-up. Because the patients in our center are elderly (ages 63–85 years), almost none participate in sexual activity. Most elderly Chinese men are sexually conservative and consider that the loss of libido and erectile function are natural consequences of aging. Thus, they seldom consult with a doctor about this embarrassing situation, although it is sometimes morbid and could be treated.
Clavien 1 grade complications were significantly different between the two groups. Of note, transient incontinence and bladder mucosal injury mainly accounted for this difference. The main factor in the occurrence of transient incontinence was the total operation time. A longer operation time seemed to cause postoperative transient incontinence more often, as well as delays in the recovery from this complication [29]. We consider that a long operation time is associated with urethral sphincter damage due to its compression, stretching, and tearing by the resectoscope during the operation. In the present study, the operative time was significantly longer for HoLEP compared to ThuLEP (p < 0.05). Bladder mucosal injury is often associated with the use of mechanical morcellation. Although all patients underwent continuous double bladder irrigation to maintain safe bladder distension during the operation, bladder mucosal injury was not avoided successfully in every patient. We attributed this finding to a technical problem. In the future, we will consider improving the operation technique to avoid injuries to the bladder wall.
ThuLEP is characterized by blunt mechanical enucleation of the adenoma [8], while ThuVEP exploits tissue vaporization to achieve prostate incision and enucleation [17]. One main advantage of ThuLEP is that tissue specimens could be reserved for pathologic examination, which avoids the risk of missing an opportunity for prostate cancer diagnosis. However, in the present study, no prostate cancer was found, nor did histopathological examination produce a high rate of malignancies. On the one hand, most prostate cancers are present in peripheral zones, and transurethral prostatectomy is executed in the transitional zone. On the other hand, to avoid the small risk of not identifying a clinically significant prostate cancer, patients were given adequate preoperative examinations even biopsy, and prostate cancer was strictly and carefully excluded in our trial.
Both HoLEP and ThuLEP ensure complete adenoma removal similar to OP, ensuring excellent and long-term functional results and a low recurrence rate [8, 16]. However, there are still some differences. HoLEP is an energy-based enucleating transurethral procedure where the plane is created by application of energy [21]. The pulsed nature of holmium:YAG includes a “scar-free” feature on the prostatic surface and makes the plane of enucleation easy to develop and follow, providing superior visibility with precise incision and dissection [23]. Moreover, patients undergoing surgical deobstruction for BPH frequently require management of concomitant pathological conditions such as bladder stones or stricture ablation, and the pulsed nature of the holmium laser allows it to be utilized for stone fragmentation as well as soft tissue applications. From a technical standpoint, HoLEP is a more versatile endoscopic tool compared with ThuLEP [25]. ThuLEP is a blunt dissection following the plane over prostatic capsule that is entitled anatomical enucleation. It is an excellent energy source for anatomical enucleation as it provides a clear and bloodless incision through prostatic tissue necessary in the initial steps of the operation when incision at 5 and 7 o’clock of bladder neck is performed. In addition, it has a narrow penetration depth protecting pericapsular tissue from unnecessary energy exposure [20]. It also offers maximum hemostasis necessary for punctual coagulation of penetrating capsular vessels during enucleation [8]. Due to the reduced surface of coagulation, ThuLEP is believed to lead to significantly less irritative symptoms than HoLEP.
This article does have limitations. The sample size was relatively small, and the study was performed in a single center; thus, multicenter and large-scale studies are warranted to further confirm the efficacy and safety of ThuLEP. Moreover, the follow-up time was not long enough, even though the results seem promising. Extended follow-up outcomes are needed to determine the exact role of ThuLEP for the surgical management of large-volume prostate. Finally, erectile and sexual functions need to be compared after these two surgeries. This issue needs to be addressed in further studies.
Conclusion
This RCT confirms that both HoLEP and ThuLEP are comparable treatment modalities in terms of perioperative complications and functional outcome parameters for large prostates (> 80 ml) during an 18-month follow-up period. However, to draw final conclusions, an extended follow-up is needed to assess the true long-term durability.
References
Becker B, Herrmann TRW, Gross AJ, Netsch C (2018) Thulium vapoenucleation of the prostate versus holmium laser enucleation of the prostate for the treatment of large volume prostates: preliminary 6-month safety and efficacy results of a prospective randomized trial. World J Urol 36(10):1663–1671. https://doi.org/10.1007/s00345-018-2321-8
Naspro R, Suardi N, Salonia A, Scattoni V, Guazzoni G, Colombo R, Cestari A, Briganti A, Mazzoccoli B, Rigatti P, Montorsi F (2006) Holmium laser enucleation of the prostate versus open prostatectomy for prostates > 70 g: 24-month follow-up. Eur Urol 50(3):563–568. https://doi.org/10.1016/j.eururo.2006.04.003
Cornu JN, Ahyai S, Bachmann A, de la Rosette J, Gilling P, Gratzke C, McVary K, Novara G, Woo H, Madersbacher S (2015) A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 67(6):1066–1096. https://doi.org/10.1016/j.eururo.2014.06.017
Yang Z, Wang X, Liu T (2013) Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology 81(2):396–400. https://doi.org/10.1016/j.urology.2012.08.069
Elshal AM, Elkoushy MA, El-Nahas AR, Shoma AM, Nabeeh A, Carrier S, Elhilali MM (2015) GreenLight laser (XPS) photoselective vapo-enucleation versus holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic hyperplasia: a randomized controlled study. J Urol 193(3):927–934. https://doi.org/10.1016/j.juro.2014.09.097
Wu G, Hong Z, Li C, Bian C, Huang S, Wu D (2016) A comparative study of diode laser and plasmakinetic in transurethral enucleation of the prostate for treating large volume benign prostatic hyperplasia: a randomized clinical trial with 12-month follow-up. Lasers Med Sci 31(4):599–604. https://doi.org/10.1007/s10103-016-1883-1
Bach T, Wendt-Nordahl G, Michel MS, Herrmann TR, Gross AJ (2009) Feasibility and efficacy of Thulium:YAG laser enucleation (VapoEnucleation) of the prostate. World J Urol 27(4):541–545. https://doi.org/10.1007/s00345-008-0370-0
Herrmann TR, Bach T, Imkamp F, Georgiou A, Burchardt M, Oelke M, Gross AJ (2010) Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol 28(1):45–51. https://doi.org/10.1007/s00345-009-0503-0
Gravas S, Bachmann A, Reich O, Roehrborn CG, Gilling PJ, De La Rosette J (2011) Critical review of lasers in benign prostatic hyperplasia (BPH). BJU Int 107(7):1030–1043. https://doi.org/10.1111/j.1464-410X.2010.09954.x
Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, Zhang YN (2008) Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol 53(2):382–389. https://doi.org/10.1016/j.eururo.2007.05.019
Saredi G, Pacchetti A, Pirola GM, Martorana E, Berti L, Scroppo FI, Marconi AM (2016) Impact of thulium laser enucleation of the prostate on erectile, ejaculatory and urinary functions. Urol Int 97(4):397–401. https://doi.org/10.1159/000446829
Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR (1998) Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol 12(5):457–459. https://doi.org/10.1089/end.1998.12.457
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Mamoulakis C, Efthimiou I, Kazoulis S, Christoulakis I, Sofras F (2011) The modified Clavien classification system: a standardized platform for reporting complications in transurethral resection of the prostate. World J Urol 29(2):205–210. https://doi.org/10.1007/s00345-010-0566-y
Reich O, Gratzke C, Stief CG (2006) Techniques and long-term results of surgical procedures for BPH. Eur urol 49(6):970–978. https://doi.org/10.1016/j.eururo.2005.12.072(discussion 978)
Elkoushy MA, Elhilali MM (2016) Management of benign prostatic hyperplasia larger than 100 ml: simple open enucleation versus transurethral laser prostatectomy. Curr Urol Rep 17(6):44. https://doi.org/10.1007/s11934-016-0601-7
Bach T, Netsch C, Haecker A, Michel MS, Herrmann TR, Gross AJ (2010) Thulium:YAG laser enucleation (VapoEnucleation) of the prostate: safety and durability during intermediate-term follow-up. World J Urol 28(1):39–43. https://doi.org/10.1007/s00345-009-0461-6
Becker B, Orywal AK, Gross AJ, Netsch C (2019) Thulium vapoenucleation of the prostate (ThuVEP) for prostates larger than 85 ml: long-term durability of the procedure. Lasers Med Sci. https://doi.org/10.1007/s10103-019-02760-1
Bach T, Huck N, Wezel F, Hacker A, Gross AJ, Michel MS (2010) 70 vs 120 W thulium:yttrium-aluminium-garnet 2 microm continuous-wave laser for the treatment of benign prostatic hyperplasia: a systematic ex vivo evaluation. BJU Int 106(3):368–372. https://doi.org/10.1111/j.1464-410X.2009.09059.x
Netsch C, Bach T, Pohlmann L, Herrmann T, Gross AJ (2012) Comparison of 120-200 W 2 mum thulium:yttrium–aluminum–garnet vapoenucleation of the prostate. J Endourol 26(3):224–229. https://doi.org/10.1089/end.2011.0173
Kyriazis I, Swiniarski PP, Jutzi S, Wolters M, Netsch C, Burchardt M, Liatsikos E, Xia S, Bach T, Gross AJ, Herrmann TR (2015) Transurethral anatomical enucleation of the prostate with Tm:YAG support (ThuLEP): review of the literature on a novel surgical approach in the management of benign prostatic enlargement. World J Urol 33(4):525–530. https://doi.org/10.1007/s00345-015-1529-0
Netsch C, Becker B, Tiburtius C, Moritz C, Becci AV, Herrmann TRW, Gross AJ (2017) A prospective, randomized trial comparing thulium vapoenucleation with holmium laser enucleation of the prostate for the treatment of symptomatic benign prostatic obstruction: perioperative safety and efficacy. World J Urol 35(12):1913–1921. https://doi.org/10.1007/s00345-017-2071-z
Zhang F, Shao Q, Herrmann TR, Tian Y, Zhang Y (2012) Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology 79(4):869–874. https://doi.org/10.1016/j.urology.2011.12.018
Tinmouth WW, Habib E, Kim SC, Kuo RL, Paterson RF, Terry CL, Elhilali M, Lingeman JE (2005) Change in serum prostate specific antigen concentration after holmium laser enucleation of the prostate: a marker for completeness of adenoma resection? J Endourol 19(5):550–554. https://doi.org/10.1089/end.2005.19.550
Pirola GM, Saredi G, Codas Duarte R, Bernard L, Pacchetti A, Berti L, Martorana E, Carcano G, Badet L, Fassi-Fehri H (2018) Holmium laser versus thulium laser enucleation of the prostate: a matched-pair analysis from two centers. Ther Adv Urol 10(8):223–233. https://doi.org/10.1177/1756287218779784
Placer J, Salvador C, Planas J, Trilla E, Lorente D, Celma A, Lopez MA, Morote J (2015) Effects of holmium laser enucleation of the prostate on sexual function. J Endourol 29(3):332–339. https://doi.org/10.1089/end.2014.0502
Briganti A, Naspro R, Gallina A, Salonia A, Vavassori I, Hurle R, Scattoni E, Rigatti P, Montorsi F (2006) Impact on sexual function of holmium laser enucleation versus transurethral resection of the prostate: results of a prospective, 2-center, randomized trial. J Urol 175(5):1817–1821. https://doi.org/10.1016/s0022-5347(05)00983-3
Carmignani L, Bozzini G, Macchi A, Maruccia S, Picozzi S, Casellato S (2015) Sexual outcome of patients undergoing thulium laser enucleation of the prostate for benign prostatic hyperplasia. Asian J Androl 17(5):802–806. https://doi.org/10.4103/1008-682X.139255
Nam JK, Kim HW, Lee DH, Han JY, Lee JZ, Park SW (2015) Risk factors for transient urinary incontinence after holmium laser enucleation of the prostate. World J Men’s Health 33(2):88–94. https://doi.org/10.5534/wjmh.2015.33.2.88
Acknowledgements
The authors would like to thank all the staff at Xiangya Hospital of Central South University for their support in generating this manuscript. The authors would like to give particular thanks to the 116 patients who agreed to this study and completed the follow-up survey. Finally, the authors would like to thank National Natural Science Foundation of China for its support.
Funding
This research was funded by National Natural Science Foundation of China 81770758 (to L.W.).
Author information
Authors and Affiliations
Contributions
JZ and LW contribute to conception and design. ZO, WH, RW, MM and LC contribute to acquisition of data. XP and ZO contribute to analysis of data. JZ contributes to drafting the article. JZ, XZ, RX, SJ, LQ and LW contribute to revising it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants/or animals were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional Review Board approval for this study was obtained from the Ethical Committee of Xiangya Hospital Central South University on 31 January 2016.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, J., Ou, Z., Zhang, X. et al. Holmium laser enucleation of the prostate versus thulium laser enucleation of the prostate for the treatment of large-volume prostates > 80 ml: 18-month follow-up results. World J Urol 38, 1555–1562 (2020). https://doi.org/10.1007/s00345-019-02945-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02945-x