Abstract
Purpose
To evaluate the diagnostic accuracy of a second look narrow-band imaging (NBI) cystoscopy in the follow-up of patients with NMIBC as compared to a second white light cystoscopy (WLI).
Patients and methods
From August 2013 to October 2014, 600 patients with history of non-muscle invasive bladder cancer (NMIBC), who presented for follow-up cystoscopy at an academic outpatient clinic, were randomized to flexible WLI-cystoscopy plus second look NBI-cystoscopy (n = 300) or flexible WLI-cystoscopy plus second look WLI-cystoscopy (n = 300) in the same session. We analysed the detection rate of bladder tumours in second look cystoscopy as primary endpoint. In addition, we evaluated recurrence rates before study enrolment and after transurethral resection (TUR-BT) in each group.
Results
In 600 patients with a history of NMIBC, 78 out of 300 patients (26%) with WLI–NBI-cystoscopy and 70 out of 300 patients (23%) with WLI–WLI-cystoscopy were diagnosed with cancer recurrence (p = 0.507). Overall, WLI–NBI detected 404 and WLI–WLI 234 lesions, respectively. The second look cystoscopy detected 57 additional cancer lesions: 45 tumours in 18 patients with WLI–NBI and 12 tumours in 9 patients with WLI–WLI (p = 0.035). After initial examination without tumour detection an improvement was determined by the second cystoscopy in 3 patients (75 vs. 78 pat.) with WLI–NBI and in only one patient (69 vs. 70 pat.) with WLI–WLI (p = 0.137). Second look cystoscopy did not influence the detection of carcinoma in situ in both groups (p = 0.120). After TUR-BT the median recurrence-free survival was 4 months in 57 recurring patients (73%) in the group with WLI–NBI- and 6 months in 56 patients (80%) with WLI–WLI-cystoscopy (p = 0.373), respectively.
Conclusion
Our study showed no differences in per-patient tumour detection between WLI and NBI. Although NBI has significant benefits for detecting individual lesions overlooked by WLI-cystoscopy, this did not positively affect recurrence-free survival after transurethral resection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Urothelial cell cancer of the bladder is a common disease with a worldwide incidence of 9/100,000 men and 2.2/100,000 women [1, 2]. At primary diagnosis, about 80% of cases present as non-muscle invasive bladder cancer (NMIBC) including pTa and pT1 disease as well as carcinoma in situ (CIS). Despite transurethral resection, patients have a high probability of recurrence between 53% in the first year and 78% in year 5 [3,4,5,6,7]. Flexible white light cystoscopy (WLI) is the current gold standard for primary diagnosis and follow-up of NMIBC-patients. It remains a matter of debate if the high recurrence rate is due to overlooking CIS or small papillary tumours using WLI-technique [8,9,10]. To improve the diagnostic and therapeutic approach of NMIBC fluorescence endoscopic imaging techniques (photodynamic diagnosis = PDD) have been introduced including the use of 5-aminolevulinic acid (5-ALA) and hexaminolevulinate (HAL) [11, 12]. Fluorescence-guided biopsy and resection increase the sensitivity especially for the detection of CIS and there is evidence for reduction of recurrence rates after TUR-BT [13, 14]. Narrow-band imaging (NBI) is another novel endoscopic technique. NBI uses two bandwidths of illumination, 415 nm (blue) and 540 nm (green), reducing the amount of red light. This increases the contrast in the superficial tissue layers, allowing the differentiation of microvascular mucosal and submucosal structures without prior instillation of dyes. After encouraging results using NBI in gastroenterologic endoscopy several reports have demonstrated improvement of tumour detection rate in NBI-cystoscopy as well [15,16,17,18,19,20,21].
The aim of the current study was to prospectively analyse the impact of a second-look NBI-cystoscopy after WLI-cystoscopy in comparison with a second look WLI-cystoscopy in the follow-up of patients with NMIBC in an urological outpatient setting.
Patients and methods
The study was conducted as a single-center study in the outpatient clinic “Praxisklinik Urologie Rhein Ruhr” (PURR) in Mülheim, Germany, which is a cooperation of five urologists. Ethical approval was obtained from the ethics committee of the local medical association (Ärztekammer Nordrhein, Nr. 2013488). Patients with recurrent non-muscle invasive transitional cell carcinoma of the bladder, stage ≤ pT1, who presented for follow-up cystoscopy, were included in the study after oral and written information and all participants signed a written consent form. Relevant comorbidities, high-risk urothelial carcinoma and age were no exclusion criteria.
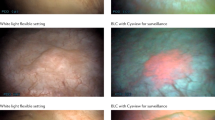
Between August 2013 and October 2014, patients were randomized to flexible WLI-cystoscopy plus second look WLI-cystoscopy or flexible WLI-cystoscopy plus second look NBI-cystoscopy in the same session (Fig. 1). Cystoscopy was performed with a flexible instrument using a chip on the tip technology (Olympus©, Shinjuku, Japan). During the first WLI-cystoscopy the tumour recurrence, the number of detected tumours and the need for TUR-BT was documented: afterwards the monitor was switched off for 10 s and a second look cystoscopy was performed by the same urologist (Fig. 2). Indication for TUR-BT was set in the case of tumour recurrence. In individual cases of multimorbid elderly patients diagnosed with a clinically singular pTa low-grade tumour, TUR-BT was postponed by 3 months followed by further diagnostic cystoscopy.
Due to the fact that PURR is an outpatient clinic, indicated surgeries were performed in four cooperating hospitals and the results of follow-up cystoscopy were communicated by written medical reports. TUR-BT was performed using WLI-technique.
SPSS 25 was used for statistical analysis: Mann–Whitney U test (median and range for continuous variables) and Chi-squared (percentage for categorical variables) analysis were employed to compare perioperative and postoperative data with statistical significance at p < 0.05.
The study was supported by Olympus® with an unrestricted grant.
Results
From August 2013 to October 2014, a total of 600 patients with a history of NMIBC were allocated to a WLI–NBI- and WLI–WLI-cystoscopy in a 1:1 ratio (Fig. 2). Tumour recurrence was found in 78 of 300 (26%) patients using WLI–NBI-cystoscopy and in 70 of 300 (23%) patients in the WLI–WLI-group (Table 1). Overall, 638 individual tumours (404 vs. 234 tumours in WLI–NBI vs. WLI–WLI) were detected (p = 0.098). Second look cystoscopy detected 57 additional cancer lesions: 45 tumours in 18 patients in the WLI–NBI- and 12 tumours in 9 patients in the WLI–WLI-group (p = 0.035). The median number of tumours in second look cystoscopy for these 27 patients was 2 vs. 1 tumour in WLI–NBI vs. WLI–WLI, respectively. After initial examination without tumour detection a per-patient improvement was determined by the second look cystoscopy in 3 patients (75 vs. 78 pat.) with WLI–NBI and in only one patient (69 vs. 70 pat.) with WLI–WLI (p = 0.137). The baseline characteristics of the patients are shown in Table 1. There were no significant differences between the two groups in age (p = 0.969), sex (p = 0.078), worst stage before study enrolment (p = 0.448), worst grade before study enrolment (p = 0.849), stage in TUR-BT (p = 0.235) and recurrence-free survival after TUR-BT (p = 0.373). In 78 patients in the WLI–NBI- and 70 patients in the WLI–WLI group the histopathological analysis of the subsequent TUR-BT showed the following results: 68 (87%) pTa, 6 (8%) pTis, 2 (3%) pT1, 1 (1%) pT2 and 1 (1%) PUNLMP in the NBI-WLI- and 65 (93%) pTa, 1 (1%) pTis, 1 (1%) pT1, 0 pT2 and 3 (4%) PUNLMP in the WLI–WLI-group (p = 0.235). With 17% vs. 6% high-grade tumours, TUR-BT detected significantly more aggressive tumours in the WLI–NBI- than in the WLI–WLI-group (p = 0.042). Second look cystoscopy did not influence detection of additional carcinoma in situ (CIS) in both groups (p = 0.120). In the WLI–NBI-group, there were six patients with CIS while the initial examination already detected four lesions. In the WLI–WLI-group only one patient with CIS was detected during the first examination and no further lesion was detected by second look cystoscopy. Subgroup analysis of patients with previous CIS showed only one patient with recurrence of carcinoma in situ in the WLI–NBI-group and no CIS recurrence in the WLI–WLI-group. The subgroup analysis of patients with previous pT1G3 showed in the WLI–WLI-group 3 patients with more tumours in the second cystoscopy, but only with pTa low-grade disease. In the WLI–NBI-group, two patients with previous T1G3 were detected with a higher number of pTa low-grade tumours. CIS was detected in one patient and the recurrence of pT1G3 in one patient, but no stage shift was observed due to the second cystoscopy. In nine patients of the WLI–NBI-group, an area conspicuous in WLI-cystoscopy was not classified as a tumour due to lack of vascularization in the NBI mode. Thus, TUR-BT could be spared.
In a total follow-up of 48 months, median recurrence-free survival after TUR-BT was 4 months in 57 patients (73%) in the WLI–NBI-group and 6 months in 56 patients (80%) following WLI–WLI-cystoscopy (p = 0.373), respectively.
Discussion
Although approximately 10 years have passed since the introduction of NBI in urology, the additional benefit at the time of follow-up cystoscopy of patients with NMIBC has not been investigated. The invention of a new visualization technique in cystoscopy faces two challenges: (1) it should improve diagnostic accuracy in the detection of bladder cancer; (2) the implementation of the technique in the transurethral resection is able to reduce the risk of recurrence and/or progression. Various studies have shown an improvement in the detection rate of bladder tumours using NBI, but it remains unclear whether the increased detection rate is due to the second thorough inspection of the bladder alone. Therefore, in our study all patients with history of bladder cancer were first examined by WLI-cystoscopy and then again in one group by WLI-cystoscopy and in the other group by NBI-cystoscopy. Our results again showed a significant benefit for NBI in the detection of additional bladder tumours overlooked by WLI cystoscopy. The second NBI-cystoscopy (WLI–NBI) detected 45 additional tumours in 18 patients and the second WLI-cystoscopy (WLI–WLI) 12 tumours in 9 patients (p = 0.035); this resulted in a diagnostic improvement in 23% of patients in the WLI–NBI- and 12% in the WLI–WLI-group. However, at the patient level no significant improvement was observed, as it was also noted in our smaller series. [22]. After initial examination without tumour detection an improvement was determined by the second look cystoscopy in 3 patients (75 vs. 78 pat.) with WLI–NBI and only one patient (69 vs. 70 pat.) with WLI–WLI (p = 0.137).
Herr et al. showed in 427 patients with NMIBC a higher detection rate of bladder tumours using NBI-cystoscopy and better visualization of carcinoma in situ [17]. In comparison to WLI–WLI-cystoscopy, our analysis showed no statistical significance for the detection of CIS using NBI. In the WLI–NBI-group there were 6 patients with CIS while the initial examination already detected 4 lesions (p = 0.120). Pooling data of a meta-analysis of seven studies including a total of 1040 patients demonstrated an additional detection rate with a random-effect estimate of 17% of patients (patient-level) with NMIBC, an additional detection rate with a random-effect estimate of 24% of tumours (tumour-level) and an additional detection rate of carcinoma in situ on the tumour-level with a random-effect estimate of 28% through the use of NBI [23]. Similar results were found in a Chinese analysis of 179 patients at risk for NMIBC, in which 59 additional tumours in 44 of 143 patients (30.8%) with bladder cancer were detected [24]. Herr et al. demonstrated in a correlation of cystoscopy with histology of 150 papillary tumours of the bladder that WLI-cystoscopy correctly predicted the histology in 93% of low-grade tumours and in combination with urinary cytology in 92% of high-grade tumours [25]. Due to the high potential for tumour progression, the identification of patients with high-risk tumours is particularly relevant in outpatient care.
In small papillary tumours, in combination with a negative or low-grade urinary cytology, tumour progression is unlikely. Therefore, in the case of a negative or low-grade urinary cytology, a detection error for these patients is not associated with tumour progression. Hernández et al. showed that “active surveillance” is safe for recurrent NMIBC. In 64 patients with previous NMIBC (stage pTa, pT1a; grade 1–2, size < 1 cm, number of tumours < 5) after 10.3 months of observation, 93.5% of the patients had not progressed in stage, 83.8% had not progressed in grade, and none of the patients experienced progression to muscle-invasive disease [26].
However, it remains unclear whether the use of NBI has an impact on the recurrence-free survival of patients. In our study, the median recurrence-free survival after transurethral resection (TUR-BT) was 4 months in 57 patients (73%) in the WLI–NBI group and 6 months in 56 patients (80%) after WLI–WLI cystoscopy with no statistical significance between the two groups after a total follow-up of 48 months (p = 0.373). With 17% vs. 6% high-grade tumours, TUR-BT detected significantly more aggressive tumours in the WLI–NBI- than in WLI–WLI-group (p = 0.042). A limitation of our study is the fact that NBI-cystoscopy was only used in follow-up cystoscopy and TUR-BT was performed in various cooperating hospitals. A recent analysis of 135 patients with NMIBC comparing TUR-BT using WLI- vs. NBI-resection of the tumours demonstrated a lower recurrence rate of 21.1% in the NBI- versus 39.7% in the WLI-group [27]. A meta-analysis of six randomized trials with 1084 patients also showed a reduction in the risk of recurrence using NBI in TUR-BT after 3 months, 1 year and 2 years [28]. On the contrary, a multicentre trial of The Clinical Research Office of the Endourological Society (CROES) demonstrated in 965 patients randomized in WLI-assisted TUR-BT and NBI-assisted TUR-BT a similar overall recurrence rate of bladder cancer within 1 year in both groups. However, NBI-assisted TUR-BT significantly reduced the likelihood of disease recurrence in low-risk patients (27.3% WLI vs. 5.6% NBI) [29]. This advantage may not be obvious in high-risk patients due to aggressive tumour biology or implantation of floating cancer cells during transurethral resection of primary tumour [30]. Therefore, in the case of high-risk tumour, complete tumour detection and resection in combination with additional intravesical chemo-/immunotherapy is essential for the patient´s prognosis.
In our outpatient clinic, follow-up care for high-risk patients (Ta/T1 high grade/CIS) is provided as a standard operating procedure using cystoscopy in combination with urinary cytology. In case of recurrence of a high-risk patient, positive urinary cytology and suspicion of CIS, PDD-guided TUR-BT should be performed as a standard procedure by the cooperating hospitals. In high-risk patients without detrusor muscle in the TUR-BT specimen, a second resection 2–6 weeks after the first resection is recommended.
For the detection of malignant tumours, particularly for CIS, it has been confirmed that fluorescence-guided biopsy and resection are more sensitive than conventional procedures [13, 31]. The meta-analysis of 14 RCTs evaluating PDD-cystoscopy with ALA or HAL demonstrated reduced recurrence rates [14], but the value of PDD-guided TUR-BT for the improvement of outcome in relation to progression rate remains to be demonstrated. A meta-analysis by Lee et al. compared the therapeutic results of PDD–TUR and NBI–TUR in addition to WLI–TUR: all cancers resected using 5-ALA-based PDD, HAL-based PDD, or NBI recurred at a lower recurrence rate than those resected using WLI-cystoscopy. No difference in progression rate was observed between cancers resected by all methods investigated [32].
Conclusion
In summary, the benefit of a second-look cystoscopy at time of NMIBC follow-up is limited. Although NBI has significant benefits for detecting individual lesions overlooked by WLI-cystoscopy, this did not translate to reduced recurrence-free survival after WLI–TUR-BT. Obviously, in addition to complete tumour resection, tumour biology seems to be of particular importance for the further course of the disease.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386. https://doi.org/10.1002/ijc.29210
Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Brenner H, Dicker DJ, Chimed-Orchir O, Dandona R, Dandona L, Fleming T, Forouzanfar MH, Hancock J, Hay RJ, Hunter-Merrill R, Huynh C, Hosgood HD, Johnson CO, Jonas JB, Khubchandani J, Kumar GA, Kutz M, Lan Q, Larson HJ, Liang X, Lim SS, Lopez AD, MacIntyre MF, Marczak L, Marquez N, Mokdad AH, Pinho C, Pourmalek F, Salomon JA, Sanabria JR, Sandar L, Sartorius B, Schwartz SM, Shackelford KA, Shibuya K, Stanaway J, Steiner C, Sun J, Takahashi K, Vollset SE, Vos T, Wagner JA, Wang H, Westerman R, Zeeb H, Zoeckler L, Abd-Allah F, Ahmed MB, Alabed S, Alam NK, Aldhahri SF, Alem G, Alemayohu MA, Ali R, Al-Raddadi R, Amare A, Amoako Y, Artaman A, Asayesh H, Atnafu N, Awasthi A, Saleem HB, Barac A, Bedi N, Bensenor I, Berhane A, Bernabe E, Betsu B, Binagwaho A, Boneya D, Campos-Nonato I, Castaneda-Orjuela C, Catala-Lopez F, Chiang P, Chibueze C, Chitheer A, Choi JY, Cowie B, Damtew S, das Neves J, Dey S, Dharmaratne S, Dhillon P, Ding E, Driscoll T, Ekwueme D, Endries AY, Farvid M, Farzadfar F, Fernandes J, Fischer F, Gebru A, Gopalani S, Hailu A, Horino M, Horita N, Husseini A, Huybrechts I, Inoue M, Islami F, Jakovljevic M, James S, Javanbakht M, Jee SH, Kasaeian A, Kedir MS, Khader YS, Khang YH, Kim D, Leigh J, Linn S, Lunevicius R, El Razek HMA, Malekzadeh R, Malta DC, Marcenes W, Markos D, Melaku YA, Meles KG, Mendoza W, Mengiste DT, Meretoja TJ, Miller TR, Mohammad KA, Mohammadi A, Mohammed S, Moradi-Lakeh M, Nagel G, Nand D, Le Nguyen Q, Nolte S, Ogbo FA, Oladimeji KE, Oren E, Pa M, Park EK, Pereira DM, Plass D, Qorbani M, Radfar A, Rafay A, Rahman M, Rana SM, Soreide K, Satpathy M, Sawhney M, Sepanlou SG, Shaikh MA, She J, Shiue I, Shore HR, Shrime MG, So S, Soneji S, Stathopoulou V, Stroumpoulis K, Sufiyan MB, Sykes BL, Tabares-Seisdedos R, Tadese F, Tedla BA, Tessema GA, Thakur JS, Tran BX, Ukwaja KN, Uzochukwu BSC, Vlassov VV, Weiderpass E, Wubshet Terefe M, Yebyo HG, Yimam HH, Yonemoto N, Younis MZ, Yu C, Zaidi Z, Zaki MES, Zenebe ZM, Murray CJL, Naghavi M (2017) Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990–2015: a systematic analysis for the global burden of disease study. JAMA Oncol 3(4):524–548. https://doi.org/10.1001/jamaoncol.2016.5688
Morgan TM, Keegan KA, Clark PE (2011) Bladder cancer. Curr Opin Oncol 23(3):275–282. https://doi.org/10.1097/CCO.0b013e3283446a11
Babjuk M, Bohle A, Burger M, Capoun O, Cohen D, Comperat EM, Hernandez V, Kaasinen E, Palou J, Roupret M, van Rhijn BW, Shariat SF, Soukup V, Sylvester RJ, Zigeuner R (2017) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol 71(3):447–461. https://doi.org/10.1016/j.eururo.2016.05.041
Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, Newling DW, Kurth K (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49(3):466–465. https://doi.org/10.1016/j.eururo.2005.12.031(discussion 475–467)
Simon M, Bosset PO, Rouanne M, Benhamou S, Radulescu C, Molinie V, Neuzillet Y, Paoletti X, Lebret T (2019) Multiple recurrences and risk of disease progression in patients with primary low-grade (TaG1) non-muscle-invasive bladder cancer and with low and intermediate EORTC-risk score. PLoS One 14(2):e0211721. https://doi.org/10.1371/journal.pone.0211721
Kim HS, Jeong CW, Kwak C, Kim HH, Ku JH (2018) Novel nomograms to predict recurrence and progression in primary non-muscle-invasive bladder cancer: validation of predictive efficacy in comparison with European Organization of Research and Treatment of Cancer scoring system. World J Urol. https://doi.org/10.1007/s00345-018-2581-3
Brausi M, Collette L, Kurth K, van der Meijden AP, Oosterlinck W, Witjes JA, Newling D, Bouffioux C, Sylvester RJ (2002) Variability in the recurrence rate at first follow-up cystoscopy after TUR in stage Ta T1 transitional cell carcinoma of the bladder: a combined analysis of seven EORTC studies. Eur Urol 41(5):523–531
Jocham D, Stepp H, Waidelich R (2008) Photodynamic diagnosis in urology: state-of-the-art. Eur Urol 53(6):1138–1148. https://doi.org/10.1016/j.eururo.2007.11.048
Rink M, Babjuk M, Catto JW, Jichlinski P, Shariat SF, Stenzl A, Stepp H, Zaak D, Witjes JA (2013) Hexyl aminolevulinate-guided fluorescence cystoscopy in the diagnosis and follow-up of patients with non-muscle-invasive bladder cancer: a critical review of the current literature. Eur Urol 64(4):624–638. https://doi.org/10.1016/j.eururo.2013.07.007
Babjuk M, Soukup V, Petrik R, Jirsa M, Dvoracek J (2005) 5-aminolaevulinic acid-induced fluorescence cystoscopy during transurethral resection reduces the risk of recurrence in stage Ta/T1 bladder cancer. BJU Int 96(6):798–802. https://doi.org/10.1111/j.1464-410X.2004.05715.x
Witjes JA, Douglass J (2007) The role of hexaminolevulinate fluorescence cystoscopy in bladder cancer. Nat Clin Pract Urol 4(10):542–549. https://doi.org/10.1038/ncpuro0917
Kausch I, Sommerauer M, Montorsi F, Stenzl A, Jacqmin D, Jichlinski P, Jocham D, Ziegler A, Vonthein R (2010) Photodynamic diagnosis in non-muscle-invasive bladder cancer: a systematic review and cumulative analysis of prospective studies. Eur Urol 57(4):595–606. https://doi.org/10.1016/j.eururo.2009.11.041
Chou R, Selph S, Buckley DI, Fu R, Griffin JC, Grusing S, Gore JL (2017) Comparative effectiveness of fluorescent versus white light cystoscopy for initial diagnosis or surveillance of bladder cancer on clinical outcomes: systematic review and meta-analysis. J Urol 197(3 Pt 1):548–558. https://doi.org/10.1016/j.juro.2016.10.061
Chiu HM, Chang CY, Chen CC, Lee YC, Wu MS, Lin JT, Shun CT, Wang HP (2007) A prospective comparative study of narrow-band imaging, chromoendoscopy, and conventional colonoscopy in the diagnosis of colorectal neoplasia. Gut 56(3):373–379. https://doi.org/10.1136/gut.2006.099614
Kara MA, Peters FP, Fockens P, ten Kate FJ, Bergman JJ (2006) Endoscopic video-autofluorescence imaging followed by narrow band imaging for detecting early neoplasia in Barrett’s esophagus. Gastrointest Endosc 64(2):176–185. https://doi.org/10.1016/j.gie.2005.11.050
Herr HW, Donat SM (2008) A comparison of white-light cystoscopy and narrow-band imaging cystoscopy to detect bladder tumour recurrences. BJU Int 102(9):1111–1114. https://doi.org/10.1111/j.1464-410X.2008.07846.x
Bryan RT, Billingham LJ, Wallace DM (2008) Narrow-band imaging flexible cystoscopy in the detection of recurrent urothelial cancer of the bladder. BJU Int 101(6):702–705. https://doi.org/10.1111/j.1464-410x.2007.07317.x(discussion 705-706)
Naselli A, Introini C, Timossi L, Spina B, Fontana V, Pezzi R, Germinale F, Bertolotto F, Puppo P (2012) A randomized prospective trial to assess the impact of transurethral resection in narrow band imaging modality on non-muscle-invasive bladder cancer recurrence. Eur Urol 61(5):908–913. https://doi.org/10.1016/j.eururo.2012.01.018
Kim SB, Yoon SG, Tae J, Kim JY, Shim JS, Kang SG, Cheon J, Lee JG, Kim JJ, Kang SH (2018) Detection and recurrence rate of transurethral resection of bladder tumors by narrow-band imaging: prospective, randomized comparison with white light cystoscopy. Investig Clin Urol 59(2):98–105. https://doi.org/10.4111/icu.2018.59.2.98
Drejer D, Beji S, Oezeke R, Nielsen AM, Hoyer S, Bjerklund Johansen TE, Lam GW, Jensen JB (2017) Comparison of white light, photodynamic diagnosis, and narrow-band imaging in detection of carcinoma in situ or flat dysplasia at transurethral resection of the bladder: the DaBlaCa-8 study. Urology 102:138–142. https://doi.org/10.1016/j.urology.2016.11.032
Hirner L, Stagge E, Rubben H, Schenck M, Eisenhardt A (2016) Narrow band imaging-assisted cystoscopy in bladder tumor follow-up: can more tumors be identified? Der Urologe Ausg A 55(3):370–375. https://doi.org/10.1007/s00120-015-3942-9
Li K, Lin T, Fan X, Duan Y, Huang J (2013) Diagnosis of narrow-band imaging in non-muscle-invasive bladder cancer: a systematic review and meta-analysis. Int J Urol 20(6):602–609. https://doi.org/10.1111/j.1442-2042.2012.03211.x
Chen G, Wang B, Li H, Ma X, Shi T, Zhang X (2013) Applying narrow-band imaging in complement with white-light imaging cystoscopy in the detection of urothelial carcinoma of the bladder. Urol Oncol 31(4):475–479. https://doi.org/10.1016/j.urolonc.2011.02.009
Herr HW (2001) Does cystoscopy correlate with the histology of recurrent papillary tumours of the bladder? BJU Int 88(7):683–685
Hernandez V, Alvarez M, de la Pena E, Amaruch N, Martin MD, de la Morena JM, Gomez V, Llorente C (2009) Safety of active surveillance program for recurrent nonmuscle-invasive bladder carcinoma. Urology 73(6):1306–1310. https://doi.org/10.1016/j.urology.2008.12.061
Kobatake K, Mita K, Ohara S, Kato M (2015) Advantage of transurethral resection with narrow band imaging for non-muscle invasive bladder cancer. Oncol Lett 10(2):1097–1102. https://doi.org/10.3892/ol.2015.3280
Kang W, Cui Z, Chen Q, Zhang D, Zhang H, Jin X (2017) Narrow band imaging-assisted transurethral resection reduces the recurrence risk of non-muscle invasive bladder cancer: a systematic review and meta-analysis. Oncotarget 8(14):23880–23890. https://doi.org/10.18632/oncotarget.13054
Naito S, Algaba F, Babjuk M, Bryan RT, Sun YH, Valiquette L, de la Rosette J (2016) The Clinical research office of the endourological society (CROES) multicentre randomised trial of narrow band imaging-assisted transurethral resection of bladder tumour (TURBT) versus conventional white light imaging-assisted TURBT in primary non-muscle-invasive bladder cancer patients: trial protocol and 1-year results. Eur Urol 70(3):506–515. https://doi.org/10.1016/j.eururo.2016.03.053
Cauberg EC, Mamoulakis C, de la Rosette JJ, de Reijke TM (2011) Narrow band imaging-assisted transurethral resection for non-muscle invasive bladder cancer significantly reduces residual tumour rate. World J Urol 29(4):503–509. https://doi.org/10.1007/s00345-011-0659-2
Mowatt G, N’Dow J, Vale L, Nabi G, Boachie C, Cook JA, Fraser C, Griffiths TR (2011) Photodynamic diagnosis of bladder cancer compared with white light cystoscopy: systematic review and meta-analysis. Int J Technol Assess Health Care 27(1):3–10. https://doi.org/10.1017/s0266462310001364
Lee JY, Cho KS, Kang DH, Jung HD, Kwon JK, Oh CK, Ham WS, Choi YD (2015) A network meta-analysis of therapeutic outcomes after new image technology-assisted transurethral resection for non-muscle invasive bladder cancer: 5-aminolaevulinic acid fluorescence vs hexylaminolevulinate fluorescence vs narrow band imaging. BMC Cancer 15:566. https://doi.org/10.1186/s12885-015-1571-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study was supported by a grant of Olympus, Germany.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tschirdewahn, S., Harke, N.N., Hirner, L. et al. Narrow-band imaging assisted cystoscopy in the follow-up of patients with transitional cell carcinoma of the bladder: a randomized study in comparison with white light cystoscopy. World J Urol 38, 1509–1515 (2020). https://doi.org/10.1007/s00345-019-02926-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02926-0