Abstract
Purpose
To investigate whether hexaminolevulinate-based (HAL) bladder tumor resection (TURBT) impacts on outcomes of patients with primary non-muscle-invasive bladder cancer (NMIBC) who were eventually treated with radical cystectomy (RC).
Methods
A total of 131 consecutive patients exhibiting NMIBC at primary diagnosis were retrospectively investigated whether they had undergone any HAL-guided TURBT prior to RC. Uni- and multivariable analyses were used to evaluate the impact of HAL-TURBT on cancer-specific (CSS) and overall survival (OS). The median follow-up was 38 months (IQR 13–56).
Results
Of the 131 patients, 69 (52.7%) were managed with HAL- and 62 (47.3%) with white light (WL)-TURBT only prior to RC. HAL-TURBT was associated with a higher number of TURBTs prior to RC (p = 0.002) and administration of intravesical chemotherapy (p = 0.043). A trend towards a higher rate of tumor-associated immune cell infiltrates in RC specimens (p = 0.07) and a lower utilization rate of post-operative systemic chemotherapy (p = 0.10) was noted for patients who were treated with HAL-TURBT. The 5-year CSS/OS was 90.9%/74.5% for the HAL-group and 73.8%/55.8% for the WL-group (p = 0.042/0.038). In multivariable analysis, lymph node tumor involvement (p = 0.007), positive surgical margins (p = 0.001) and performance of WL-TURBT only (p = 0.040) were independent predictors for cancer-specific death.
Conclusions
The present data suggest that the resection of NMIBC under HAL exerts a beneficial impact on outcomes of patients who will need to undergo RC during their course of disease. This finding may be due to improved risk stratification as the resection under HAL may allow more patients to be treated timely and adequately.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bladder cancer (BC) is the 11th commonest malignancy worldwide with up to 80% of patients presenting with non-muscle invasive bladder cancer (NMIBC) at primary diagnosis (PD) [1]. Transurethral bladder tumor resection (TURBT) and intravesical instillation therapy represent the mainstay of treatment for NMIBC [2]. Despite the initially high cure rates, the long-term risk of disease recurrence and progression in NMIBC remains considerable [3]. Therefore, patients with NMIBC at high or very high risk of progression can be offered upfront radical cystectomy (RC) according to recent guidelines [1, 2].
In the past, cystoscopy and TURBT have been performed only under white-light (WL) conditions. The development of photodynamic diagnosis (PDD) for BC has improved the tumor detection rates during these procedures [4]. Hexaminolevulinic acid (HAL) is a hexyl ester of 5-aminolevulinic acid (ALA) and approved for PDD of the bladder [5, 6]. It improves the visibility of cancerous lesions through prompting intracellular accumulation of photoactive porphyrines, especially within neoplastic urothelial cells [7]. In a meta-analysis of randomized trials, HAL-based TURBT displayed superiority over WL-based TURBT by increasing the detection rates of Ta–T1 and carcinoma in situ (CIS) lesions by 20% and 40%, respectively [8]. Based on the new International Bladder Cancer Group (IBCG) criteria for NMIBC progression, another meta-analysis of randomized trials reported significantly lower disease progression rates for HAL compared to WL-TURBT [9]. Furthermore, the largest randomized trial on HAL to date reported that the long-term risk of undergoing RC was reduced by 44% for patients treated with HAL- versus WL-TURBT [10].
Critical determinants for survival after RC include tumor stage, lymph node status, soft-tissue surgical margins (STSMs) and the presence of lymphovascular invasion (LVI) [11]. In general, survival rates after RC for NMIBC are superior to those performed for muscle-invasive bladder cancer (MIBC) [12]. Yet, in the literature, a history of disease progression from NMIBC to MIBC was found to be associated with a lower CSS when compared to patients treated with RC for primary MIBC [13]. Therefore, we aimed to investigate the prognostic value of HAL- vs. WL-based TURBT on survival of patients who initially presented with NMIBC and required RC during their course of disease.
Patients and methods
Patients
In this retrospective observational analysis, approved by the Local Ethics Committee Tübingen, the clinical and histopathologic records of 131 consecutive patients who were diagnosed with NMIBC at primary diagnosis (PD) and were treated with RC with curative intent between 2004 and 2013 were reviewed. The indication for the use of HAL at TURBT was constant during study period. Generally, for patients referred primarily to our department during the investigated period, every TURBT for suspected BC was conducted under HAL. HAL-TURBT was also utilized in our department for second resection when the last TURBT was conducted more than 8 weeks ago. All 131 patients were cystectomized in our center and the indication for cystectomy was constant during study period. Indication for primary cystectomy in NMIBC was multifocal (≥ 3 lesions) T1 high-grade bladder cancer and extensive NMIBC of any grade and stage not amenable to endoscopic and instillation therapy. In addition, patients with persistent or progressive disease following BCG instillation therapy and progression to MIBC were recommended to undergo RC.
We assessed various clinical and histopathologic parameters: age at RC, gender, Eastern Cooperative Oncology Group (ECOG) performance status (PS) at RC, number of TURBTs prior to RC, time interval between the first and last TURBT, time between last TURBT and RC, tumor multifocality at PD, presence of CIS at PD, clinical and histopathologic tumor stage at PD and RC, tumor grade at PD and RC, lymph node tumor involvement, STSMs, LVI, tumor size at RC, hydronephrosis at RC, histological entity of BC (urothelial vs. non-urothelial), presence of tumor-associated immune cell infiltrates (TAICs) in RC specimens, administration of intravesical immuno- and/or chemotherapy and receipt of post-operative systemic chemotherapy. Clinical tumor stage at RC considers the highest tumor stage prior to RC irrespective of whether detected on histopathological analysis at any TURBT or at cross-sectional imaging prior to RC.
Histologic assessment
The histopathologic assessment was performed in the Tubingen pathology department and was based on the TNM classification approved by the AJCC [14]. The histopathologic macro- and microscopic examination of cystectomy specimens included cross-sectioning of the entire specimen with immunohistochemical staining to identify BC [15].
Follow-up
Generally, patients were seen post-operatively at least every 3–4 months for the first year, semiannually for the second and third years, and annually thereafter. Besides history, clinical examination and standard laboratory tests, cross-sectional imaging, endoscopy and urinary cytology were done at regular intervals to detect recurrence. Recurrence was defined as any visible tumor in the surgical bed, in distant organs or in the remnant urothelium [16]. The median follow-up after RC was 38 months (IQR 13–56). Cancer-specific survival (CSS) and overall survival (OS) were measured from the date of RC to (cancer-specific) death or last follow-up, respectively, as determined by patient charts.
Statistical analysis and model development
For univariable analysis, the Fisher Exact/χ2 test was used for nominal data and t test for scaled parameters. Values are given as mean, median and interquartile range (IQR). Kaplan–Meier plots were used to estimate CSS and OS. Uni- and multivariable Cox-proportional hazard analyses were carried out to evaluate risk factors for cancer-specific death. p values are two sided with p < 0.05 considered significant. Statistical analysis was performed with JMP® 12.0 (Cary, NC, USA).
Results
Of the 131 patients, 69 (52.7%) were managed with at least one HAL- and 62 (47.3%) with WL-TURBT only prior to RC. HAL-TURBT was associated with a higher number of TURBTs before RC (p = 0.002) and a higher rate of administration of intravesical chemotherapy (p = 0.043). A trend towards a higher rate of TAICs in RC specimens (p = 0.07) and a lower utilization rate of palliative systemic chemotherapy after RC (p = 0.10) was noted for patients who were treated with HAL-TURBT (see Table 1). In the HAL-group, the median number of HAL-based TURBTs was 1.7 (median 1, IQR 1–2).
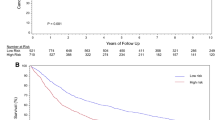
The 5-year CSS was 90.9% for patients treated with HAL-TURBT and 73.8% for patients with WL-TURBT (p = 0.042; see Fig. 1). The 5-year OS was 74.5% for HAL- and 55.8% for WL-TURBT (p = 0.038; see Fig. 2). In univariable Cox-regression analysis, advanced histopathologic tumor stage, lymph node tumor involvement, positive STSMs, lymphovascular invasion (all p < 0.001) and performance of WL-guided TURBT only (p = 0.039) prior to RC were risk factors for inferior CSS. In multivariable analysis, lymph node tumor involvement (p = 0.005), positive STSMs (p = 0.001) and absence of HAL-TURBT (p = 0.031) were independent prognosticators for increased cancer-specific mortality (see Table 2).
Cancer-specific survival of patients with primary NMIBC who were treated with at least one HAL- (blue line) vs. WL-guided only TUR-B (red line) and underwent radical cystectomy during the course of disease (Leg.: HAL hexaminolevulinate, NMIBC non-muscle invasive bladder cancer, TURBT transurethral bladder tumor resection, WL white light)
Overall survival of patients with primary NMIBC who were treated with at least one HAL- (blue line) vs. WL-guided only TURBT (red line) and underwent radical cystectomy during the course of disease (Leg.: HAL hexaminolevulinate, NMIBC non-muscle invasive bladder cancer, TURBT transurethral bladder tumor resection, WL white light)
Discussion
In this study, we found that patients with NMIBC at PD who were eventually treated with RC during their course of disease exhibited superior survival if they had undergone at least one HAL-TURBT prior to surgery compared to those who underwent only WL-based procedures. In addition, patients in the HAL-group exhibited higher rates of TURBT and intravesical chemotherapy albeit the clinical and histopathologic parameters were not significantly different at PD and RC between both groups.
HAL-based TURBT has been confirmed to increase the detection rate of malignant lesions in the bladder, especially CIS [8]. This correlates with evidence that HAL-based TURBT significantly reduces recurrence rates in patients with primary or recurrent NMIBC [5]. Moreover, a beneficial effect of HAL-TURBT on progression in both NMIBC and MIBC was reported in recent studies [5, 9, 17, 18]. Accordingly, the EAU guidelines emphasize the use of HAL especially in patients with positive urinary cytology or expected high-risk disease [2].
Advanced histopathologic tumor and nodal stage, positive STSMs and LVI have been confirmed as independent prognostic factors for inferior survival after RC [11, 19]. Likewise, in the present study, univariable and multivariable analyses confirmed advanced stage, positive lymph nodes, positive STSMs and LVI to be associated with lower CSS. This concordance underlines the reproducibility and validity of our analysis compared to larger series [11]. Taking a closer look into the literature, lymph node positivity and positive resection margins exhibit the highest prognostic potential compared to tumor stage and lymphovascular invasion. In fact, patients with locally advanced but node-negative disease with concurrent lymphovascular invasion (≥ pT3a pN0 LVI) show markedly improved survival rates compared to those with any positive lymph nodes (pTany pN + LV any; [11]. Moreover, those with positive STSMs exhibit the worst survival rates which are often associated rapid progression after RC. In other words, the adverse prognostic potential of lymph node positivity and positive soft-tissue surgical margins is higher than that of tumor stage and lymphovascular invasion. This puts into perspective the finding that pT-stage and LVI were not found to be independently associated with CSS when tested in the final model against HAL-TURBT.
Furthermore, the rate of stage cT3 disease (28.2%) for this specific cohort of patients with primary NMIBC is comparable to the results of larger series [20]. It has to be taken into consideration that radiological imaging prior to RC was usually conducted after the last TURBT which may be prone to staging inaccuracies because of TURBT-related tissue artefacts. At the time our patients were treated, the role of neoadjuvant chemotherapy for cT3 stage was controversially in our country. In addition, the EAU guidelines have upgraded the recommendation of adjuvant chemotherapy [1] based on the results of recent randomized trials [21]. Moreover, the overall rate of lymph node-positive disease at RC in this specific cohort is comparable to other series [11, 20]. In terms of the rate of positive soft-tissue surgical margins, our rates are in accordance with the results of contemporary randomized studies on the use of RC in patients with ≥ T1G3 bladder cancer (8–9%; [22]). Moreover, a total of 14 patients (10.7%) had pT4a–b disease which is associated with a considerably higher risk of positive STSMs.
Interestingly, we found that the performance of WL-TURBT only during the course of disease was an independent risk factor for inferior CSS. Therefore, the question derives how HAL-TURBT may have exerted such a strong beneficial impact of survival outcomes in this cohort. In the present study, the HAL and WL cohorts were comparable in terms of their patient characteristics and histopathologic parameters both at PD and RC. The median time interval between the first TURBT and RC was not significantly different between both groups. By contrast, the median number of performed TURBTs per patient was higher in the HAL-group. This might also explain the fact that the number of patients receiving intravesical chemotherapy was about twofold higher in the HAL compared to the WL cohort. Theoretically, a possible explanation for these findings may be that the use of HAL-TURBT resulted in improved tumor detection and completeness of resection that also translated into improved risk stratification and optimized management with chemoinstillation.
Progression of NMIBC to MIBC was shown to be associated with inferior cancer-related outcomes after RC compared with primary MIBC [13]. We did not find a significant difference in the various histopathologic determinants for survival at PD and after RC between both groups which does not allow to draw the conclusion that HAL-TURBT may have delayed histopathologic progression of NMIBC to MIBC. Although the use of intravesical chemoinstillation was more frequent in the HAL cohort, a large randomized trial has shown intravesical chemoinstilation to be associated with improved intravesical recurrence-free but not progression-free survival in intermediate- to high-risk NMIBC patients [23]. Therefore, it is unlikely that chemoinstillation can reduce risk of progression translating into lower T- and N-stage and thus improved CSS after RC. However, while the number of TURBT was significantly higher in the HAL-cohort the time interval between primary diagnosis and last TURBT as well as the time interval between last TURBT and RC were similar. This underscores that the “density of treatment” was much higher in the HAL cohort which may also have exerted a beneficial therapeutic impact on outcomes. Nonetheless, since progression to MIBC at RC was noted to a similar extent in both groups, the role of HAL-TURBT deserves further attention with regard to its possible molecular effects on tumor and immune cells.
The presence of TAICs in specimens has been reported as a beneficial prognostic factor in various solid tumors, including BC [24,25,26,27]. The higher rate of TAICs in RC specimens in the HAL-group raises the question about the cytotoxic or immunogenic activities of HAL. In fact, the cytotoxicity of photosensitizers has been investigated in various studies in the last years [28]. Zenzen et al. investigated the cytotoxic and mutagenic effect of the 5-aminolevulinic acid hexylester (h-ALA) on tumor and fibroblast cell lines, and found h-ALA to display a favorable selective cytotoxic effect on tumor cells [29]. Ekroll et al. investigated the destructive effect of the photodynamic therapy using HAL-mediated photodynamic therapy (PDT) on bladder urothelial carcinoma cell lines in the rat. They detected a noticeable increase of cellular apoptosis and proposed modifications of the PDT protocol for adjustment of the light wavelengths to increase the rate of apoptosis [30].
There are limitations of our study that have to be taken into account in the interpretation of results. First, the results have to be interpreted cautiously with consideration of its retrospective nature and the number of the included patients. We admit that our cohort is rather a heterogenous group of high-risk patients. Second, although the indication for the use of HAL for patients treated with TURBT in our hospital was constant during this period, a confounding bias may exist with regard to those patients who were treated once, several times or exclusively in external hospitals with TURBT at any time point during the course of their disease. In this regard, we cannot adjust for the in-hospital policy of external hospitals in terms of the use of HAL during the investigated time period. Thus, we cannot extrapolate the magnitude of bias for this specific aspect. In terms of recurrence and progression rates, we acknowledge that our database does not capture data on the effects of instillation therapy since intravesical instillation therapy is usually conducted in Germany by office urologists. Since intravesical recurrence-free survival is improved with HAL [5, 6, 8], it can be assumed that resection under HAL improves the quality and completeness of the procedure which may translate into improved outcomes reflected by standard clinical and histopathological parameters. In addition, possible molecular mechanisms of how HAL may have influenced bladder cancer cell proliferation remain hypothesis generating. In addition, external validation and data from larger series are also necessary to verify these findings.
In summary, this analysis suggests that patients who have undergone bladder tumor resection with HAL exhibit improved outcomes even when they progress to disease stages which require RC for definitive treatment compared to patients who undergo WL-based procedures only prior to RC. This may be due to improved risk stratification as the detection and resection of BC under HAL may allow more patients to be treated timely and adequately. Albeit these data warrants further validation, they are supportive of results of recent studies on the beneficial long-term impact of HAL-based TURBT in patients with BC.
References
Witjes JA, Comperat E, Cowan NC, De Santis M, Gakis G, Lebret T, Ribal MJ, Van der Heijden AG, Sherif A, European Association of U (2014) EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol 65:778–792
Babjuk M, Bohle A, Burger M, Capoun O, Cohen D, Comperat EM, Hernandez V, Kaasinen E, Palou J, Roupret M, van Rhijn BW, Shariat SF, Soukup V, Sylvester RJ, Zigeuner R (2017) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol 71:447–461
Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, Newling DW, Kurth K (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49:465–466
Stenzl A, Eder I, Kostron H, Klocker H, Bartsch G (1996) Electromotive diffusion (EMD) and photodynamic therapy with delta-aminolaevulinic acid (delta-ALA) for superficial bladder cancer. J Photochem Photobiol 36:233–236
Grossman HB, Stenzl A, Fradet Y, Mynderse LA, Kriegmair M, Witjes JA, Soloway MS, Karl A, Burger M (2012) Long-term decrease in bladder cancer recurrence with hexaminolevulinate enabled fluorescence cystoscopy. J Urol 188:58–62
Stenzl A, Burger M, Fradet Y, Mynderse LA, Soloway MS, Witjes JA, Kriegmair M, Karl A, Shen Y, Grossman HB (2010) Hexaminolevulinate guided fluorescence cystoscopy reduces recurrence in patients with nonmuscle invasive bladder cancer. J Urol 184:1907–1913
Fotinos N, Campo MA, Popowycz F, Gurny R, Lange N (2006) 5-Aminolevulinic acid derivatives in photomedicine: characteristics, application and perspectives. Photochem Photobiol 82:994–1015
Burger M, Grossman HB, Droller M, Schmidbauer J, Hermann G, Dragoescu O, Ray E, Fradet Y, Karl A, Burgues JP, Witjes JA, Stenzl A, Jichlinski P, Jocham D (2013) Photodynamic diagnosis of non-muscle-invasive bladder cancer with hexaminolevulinate cystoscopy: a meta-analysis of detection and recurrence based on raw data. Eur Urol 64:846–854
Gakis G, Fahmy O (2016) Systematic review and meta-analysis on the impact of hexaminolevulinate- versus white-light guided transurethral bladder tumor resection on progression in non-muscle invasive bladder cancer. Bladder Cancer 2:293–300
Malmstrom PU, Hedelin H, Thomas YK, Thompson GJ, Durrant H, Furniss J (2009) Fluorescence-guided transurethral resection of bladder cancer using hexaminolevulinate: analysis of health economic impact in Sweden. Scand J Urol Nephrol 43:192–198
Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, Skinner E, Bochner B, Thangathurai D, Mikhail M, Raghavan D, Skinner DG (2001) Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1054 patients. J Clin Oncol 19:666–675
Hautmann RE, de Petriconi RC, Pfeiffer C, Volkmer BG (2012) Radical cystectomy for urothelial carcinoma of the bladder without neoadjuvant or adjuvant therapy: long-term results in 1100 patients. Eur Urol 61:1039–1047
van den Bosch S, Alfred Witjes J (2011) Long-term cancer-specific survival in patients with high-risk, non-muscle-invasive bladder cancer and tumour progression: a systematic review. Eur Urol 60:493–500
Sobin LH, Wittekind C (2002) TNM classification of malignant tumors, 6th edn. Wiley, New York
Shim JW, Cho KS, Choi YD, Park YW, Lee DW, Han WS, Shim SI, Kim HJ, Cho NH (2008) Diagnostic algorithm for papillary urothelial tumors in the urinary bladder. Virchows Arch 452:353–362
Gakis G, Black PC, Bochner BH, Boorjian SA, Stenzl A, Thalmann GN, Kassouf W (2017) Systematic review on the fate of the remnant urothelium after radical cystectomy. Eur Urol 71:545–557
Gakis G, Ngamsri T, Rausch S, Mischinger J, Todenhofer T, Schwentner C, Schmid MA, Hassan FA, Renninger M, Stenzl A (2015) Fluorescence-guided bladder tumour resection: impact on survival after radical cystectomy. World J Urol 33:1429–1437
Karaolides T, Skolarikos A, Bourdoumis A, Konandreas A, Mygdalis V, Thanos A, Deliveliotis C (2012) Hexaminolevulinate-induced fluorescence versus white light during transurethral resection of noninvasive bladder tumor: does it reduce recurrences? Urology 80:354–359
Gakis G, Efstathiou J, Lerner SP, Cookson MS, Keegan KA, Guru KA, Shipley WU, Heidenreich A, Schoenberg MP, Sagaloswky AI, Soloway MS, Stenzl A, International Consultation on Urologic Disease-European Association of Urology Consultation on Bladder C (2013) ICUD-EAU International Consultation on Bladder Cancer 2012: Radical cystectomy and bladder preservation for muscle-invasive urothelial carcinoma of the bladder. Eur Urol 63:45–57
Parker WP, Smelser W, Lee EK, Habermann EB, Thapa P, Zaid HB, Frank I, Griebling TL, Tollefson MK, Thompson RH, Holzbeierlein JM, Karnes RJ, Boorjian SA (2017) Utilization and outcomes of radical cystectomy for high-grade non-muscle-invasive bladder cancer in elderly patients. Clin Genitourin Cancer. https://doi.org/10.1016/j.clgc.2017.07.011
Sternberg CN, Skoneczna I, Kerst JM et al (2015) Immediate versus deferred chemotherapy after radical cystectomy in patients with pT3-pT4 or N + M0 urothelial carcinoma of the bladder (EORTC 30994): an intergroup, open-label, randomised phase 3 trial. Lancet Oncol 16:76–86
Gschwend JE, Heck MM, Lehmann J, Rubben H, Albers P, Wolff JM, Frohneberg D, de Geeter P, Heidenreich A, Kalble T, Stockle M, Schnoller T, Stenzl A, Muller M, Truss M, Roth S, Liehr UB, Leissner J, Bregenzer T, Retz M (2019) Extended versus limited lymph node dissection in bladder cancer patients undergoing radical cystectomy: survival results from a prospective, randomized trial. Eur Urol 75:604–611
Sylvester RJ, Brausi MA, Kirkels WJ, Hoeltl W, Calais Da Silva F, Powell PH, Prescott S, Kirkali Z, van de Beek C, Gorlia T, de Reijke TM, Group EG-UTC (2010) Long-term efficacy results of EORTC genito-urinary group randomized phase 3 study 30911 comparing intravesical instillations of epirubicin, bacillus Calmette-Guerin, and bacillus Calmette-Guerin plus isoniazid in patients with intermediate- and high-risk stage Ta T1 urothelial carcinoma of the bladder. Eur Urol 57:766–773
Yu A, Mansure JJ, Solanki S, Siemens DR, Koti M, Dias ABT, Burnier MM, Brimo F, Kassouf W (2018) Presence of lymphocytic infiltrate cytotoxic T lymphocyte CD3+ , CD8+ , and immunoscore as prognostic marker in patients after radical cystectomy. PLoS One 13:e0205746
Pichler R, Gruenbacher G, Culig Z, Brunner A, Fuchs D, Fritz J, Gander H, Rahm A, Thurnher M (2017) Intratumoral Th2 predisposition combines with an increased Th1 functional phenotype in clinical response to intravesical BCG in bladder cancer. Cancer Immunol Immunother 66:427–440
Jarosch A, Sommer U, Bogner A, Reissfelder C, Weitz J, Krause M, Folprecht G, Baretton GB, Aust DE (2018) Neoadjuvant radiochemotherapy decreases the total amount of tumor infiltrating lymphocytes, but increases the number of CD8+/Granzyme B+ (GrzB) cytotoxic T-cells in rectal cancer. Oncoimmunology 7:e1393133
Blando J, Sharma A, Higa MG, Zhao H, Vence L, Yadav SS, Kim J, Sepulveda AM, Sharp M, Maitra A, Wargo J, Tetzlaff M, Broaddus R, Katz MHG, Varadhachary GR, Overman M, Wang H, Yee C, Bernatchez C, Iacobuzio-Donahue C, Basu S, Allison JP, Sharma P (2019) Comparison of immune infiltrates in melanoma and pancreatic cancer highlights VISTA as a potential target in pancreatic cancer. Proc Nati Acad Sci USA 25:25. https://doi.org/10.1073/pnas.1811067116
Halkiotis K, Yova D, Pantelias G (1999) In vitro evaluation of the genotoxic and clastogenic potential of photodynamic therapy. Mutagenesis 14:193–198
Zenzen V, Zankl H (2004) In vitro evaluation of the cytotoxic and mutagenic potential of the 5-aminolevulinic acid hexylester-mediated photodynamic therapy. Mutat Res 561:91–100
Ekroll IK, Gederaas OA, Helander L, Hjelde A, Melo TB, Johnsson A (2011) Photo induced hexylaminolevulinate destruction of rat bladder cells AY-27. Photochem Photobiol Sci 10:1072–1079
Author information
Authors and Affiliations
Contributions
MR and OF manuscript writing. TS, FH and AS project development. MAS data collection. GG project development, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
G. Gakis: receipt of speaker honoraria and travel grants from IPSEN, Ettlingen, Germany. All other authors have nothing to disclose in relation with the content of the manuscript.
Ethical approval
The study was approved by the local ethics committee of the university of Tübingen (Approval number: 417/2010A).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Renninger, M., Fahmy, O., Schubert, T. et al. The prognostic impact of hexaminolevulinate-based bladder tumor resection in patients with primary non-muscle invasive bladder cancer treated with radical cystectomy. World J Urol 38, 397–406 (2020). https://doi.org/10.1007/s00345-019-02780-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02780-0