Abstract
Purpose
Testosterone supplement treatment (TST) is a classic therapy for hypogonadal men with type 2 diabetes mellitus (T2DM), but the effects of TST in different studies are inconsistent. We conducted this meta-analysis to evaluate the precise role of TST in hypogonadal men with T2DM.
Methods
PubMed, Embase, Cochrane Library and Web of Science were searched to identify qualified randomized controlled trials (RCTs). Pooled mean differences (MDs) with 95% confidence intervals (CIs) were calculated to measure the specific effects of TST. Trial sequential analysis was performed to verify the pooled results.
Results
A total of eight RCTs were enrolled in our meta-analysis, including 596 hypogonadal participants with T2DM. Compared with comparators, TST can significantly improve glycemic control by reducing homeostatic model assessment of insulin resistance (MD − 0.79, 95% CI − 1.23 to − 0.34), fasting glucose (MD − 0.98, 95% CI − 1.13 to − 0.54), fasting insulin (MD − 2.47, 95% CI − 3.99 to − 0.95) and HbA1c% (MD − 0.45, 95% CI − 0.73 to − 0.16). In addition, TST can result in a decline in cholesterol (MD − 0.29, 95% CI − 0.38 to − 0.19) and triglyceride (MD − 0.37, 95% CI − 0.59 to − 0.15).
Conclusion
Our results indicated that TST can improve glycemic control and decrease TC and TG in hypogonadal patients with T2DM. We recommend TST during the anti-diabetic therapy in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to Endocrine Society Clinical Practice Guideline in 2010, male hypogonadism was defined as “a clinical syndrome that results from failure of the testis to produce physiological levels of testosterone (androgen deficiency) and a normal number of spermatozoa due to disruption of one or more levels of the hypothalamic–pituitary–testicular axis” [1]. Diagnosis of male hypogonadism requires both the persistent clinical symptoms and androgen deficiency [2]. Hypogonadism can significantly affect patients’ multiple organ functions and quality of life, and has become a great challenge to the world. In men aged between 40–79, the incidence of hypogonadism varied from 2.1 to 5.7%, according to an epidemiological study in America [3]. Many factors were reported associated with male hypogonadism, including obesity, comorbidities and poor health status [2, 4]. Recently, various studies have demonstrated the association between type 2 diabetes mellitus (T2DM) and hypogonadism [5,6,7,8,9,10,11,12]. A meta-analysis in 2010 revealed the association between T2DM and lower total serum testosterone levels by a multiple regression model adjusting for age and body mass index [13]. The specific mechanism of lower testosterone in T2DM patients is not clear. Any impairment in the hypothalamic–pituitary–testicular axis may lead to lower serum testosterone.
Considering the low testosterone level and clinical symptoms in hypogonadal men, prescriptions for testosterone replacement therapy (TST) have increased significantly in the past few years [2]. TST may present several benefits including growth of muscle mass and strength, increased bone density, improvement in metabolic control, psychological and sexual parameters in hypogonadal patients [14,15,16,17,18]. The effects of TST on hypogonadal patients with T2DM were studied in various trials [19,20,21,22,23,24,25,26,27,28], including changes in glycometabolism, lipid parameters, blood pressure, body fat percentages, BMI indexes, the Aging Males’ Symptoms (AMS) scale, and International Index of Erectile Function (IIEF) scores. However, some studies demonstrated contradictory results. For instance, with regard to glycometabolism, several studies demonstrated that TST can result in a significant reduction in HOMA-IR [20, 26, 28], FSG [19, 20, 26, 28], FSI [20, 26] and HbA1c% [19, 21, 26, 27] in hypogonadal patients with T2DM. However, the other data did not show significant decrease of these indicators in TST groups.
In terms of lipid parameters, TST was reported associated with decrease in TC [21, 24, 27, 28], TG [26], serum HDL levels [21], serum LDL levels [21], and increase in serum HDL levels [26]. Other studies did not show a significant improvement in lipid metabolism. Meta-analysis as a powerful tool can provide more reliable results than a single study, especially in explaining controversial conclusions. We performed this meta-analysis to evaluate the precise role of TST in hypogonadal men with T2DM.
Materials and methods
This meta-analysis was strictly reported according to the PRISMA (Preferred reporting items for systematic review and meta-analyses) statement [29] (Table S1).
Search strategy and quality assessment
Databases including PubMed, Embase, Cochrane Library and Web of Science were searched to identify qualified trials published up to January 2018. The combination of the following search items was used: “testosterone”, “androgen”, “diabetes mellitus”, “TST”, “TRT”, “hypogonadism” and “randomized controlled trial”. In addition to electronic search original papers, reference lists of the original articles and reviews were evaluated manually to obtain more eligible studies. Besides, if the research results were unclear or more data were needed, we would contact the corresponding author and participating trialists to get desired information.
Studies involved in this meta-analysis should fulfill the following criteria: (1) English publications; (2) randomized controlled studies; (3) researches associated with the effects of TST in hypogonadal patients with T2DM. To maintain the quality of this meta-analysis, the major exclusion criteria were listed as follows: (1) no clear definitions of the diagnosis of the late-onset hypogonadism and T2DM, population, amount and serving method of testosterone or the outcome assessment; (2) without placebo groups or no treatment groups; (3) insufficient data for estimating a mean difference (MD) with 95% confidence interval (CI); (4) duplicates of previous publication.
Moreover, all included RCTs were evaluated according to the 25-item CONSORT checklists, which focus on reporting how the trials were designed, analyzed, and interpreted (Table S2). The quality of the included RCTs was scored by assessing how many of the 25 items were reported. The number of reported items is positively associated with the quality of a RCT. A research with high quality will report all 25 criteria [30].
Data extraction
Two investigators reviewed the identified studies independently to determine whether an individual article could be included. Uncertain data were reassessed and solved by a discussion. All data were recorded in a standardized form and the following basic characteristics from each study were extracted: first author’s name, year of publication, country, ethnicity, testosterone cut-off point, diabetes duration, testosterone regimen, medications on comparators, mean age, HbA1c% and total serum testosterone level. The aforementioned data are detailed in Table 1. The primary outcomes were extracted as follows: homeostatic model assessment of insulin resistance (HOMA-IR), fasting plasma glucose (FSG), fasting serum insulin (FSI), HbA1c, total cholesterol (TC), triglyceride (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL), body fat, BMI index, systolic and diastolic blood pressure (SBP and DBP), AMS and international index of erectile function (IIEF). The outcomes mentioned above were listed in Table 2.
Trial sequential analysis
Random errors in a meta-analysis can mislead findings [31, 32]. TSA was performed in this meta-analysis to control the risk of random error to obtain a more comprehensive assessment of analyses [33,34,35,36]. The cumulative Z-curve was constructed at first. Next, crossing of Z = 1.96 (P = 0.05) or the monitoring boundaries was assessed. When the cumulative Z-curve crossed by the monitoring boundaries, the result was considered firm. In our study, a power of 80% (20% risk of a type II error) and 5% risk of a type I error was set in TSA. Moreover, 20% relative risk increase was predetermined according to the required information size and 95% CI was provided. The software (TSA, version 0.9; Copenhagen Trial Unit, Copenhagen, Denmark, 2011) was used in the current trial sequential analysis.
Statistical analysis
Data were presented as mean and standard deviation (SD). If only standard error or from the 95% confidence interval of the mean difference (MD) was available, SD value will be transformed. If only median and range were given, a forum described previously was used to estimate mean and SD: Mean ≈ Median; SD ≈ Norm IQR = (P75–P25)*0.7413 (IQR: inter-quartile range, P75: 75th percentile, P25: 25th percentile) [37].
Sensitivity analysis was conducted by repeating the meta-analysis while omitting one single study each time. Heterogeneity was assessed by Higgins I2 statistic and Cochrane Q test. A fixed-effect model was applied if the heterogeneity was not significant (p > 0.05 or I2 < 50%). Otherwise, a random-effect model was utilized. The inverse variance method was applied in a fixed-effect model and the DerSimonian–Laird method was utilized in a random-effect model [38, 39]. Pooled MDs with the corresponding 95% CIs were calculated through above methods. A pooled MD value lower than 0 indicated that TST was associated with decrease of specific parameters, and the result was considered significant if the 95% CI did not include 0. Publication bias was evaluated by Egger’s linear regression test with a funnel plot. The statistics were analyzed by Stata version 12 (StataCorp LP, College Station, TX, USA).
Results
Characteristics of the enrolled studies
The study selection process was shown in Fig. 1. Finally, a total of eight RCTs including 596 hypogonadal participants with T2DM met the inclusion criteria and were enrolled in our meta-analysis [19,20,21, 23, 24, 26,27,28]. Noticeably, hypogonadism was diagnosed according to different norms in these studies and was defined as at least three sexual symptoms and total testosterone (TT) < 11 nmol/L [26, 27] or TT < 12 nmol/L [21, 24, 25, 28] or TT < 15 nmol/L [19] or free testosterone (FT) < 225 pmol/L [20, 23]. The primary testosterone regimen varied from the enrolled studies. Oral testosterone, testosterone gel by intradermal injection, testosterone by deep intramuscular injection were utilized in one [19], two [26, 27] and five [20, 21, 23, 26, 28] studies, respectively. In addition, testosterone was given at various doses and schedules in these studies. Among the eight RCTs, six trials were double-blind, placebo-controlled studies [20, 21, 23,24,25, 27, 28], while the other two were single-blind, no treatment controlled studies [19, 26]. Six articles focused on Caucasian [19,20,21, 24,25,26, 28], one focused on Asian [23] and the last one is a multi-ethnicity study [27]. The basic characteristics of the involved trials were listed in Table 1.
The effects on glycometabolism
A total of eight studies have reported the glycol-metabolic effects of TST. Among them, three trials demonstrated a reduction in HOMA-IR [20, 26, 28], four showed a decrease in FSG [19, 20, 26, 28], two manifested a decrease in FSI [20, 26] and four reported a decline in HbA1c% [19, 21, 26, 27]. The rest data were not significant between the TST and comparator groups.
Our meta-analyses results showed that, compared with comparators, TST can significantly improve glycemic control, and reduce HOMA-IR (MD: − 0.79, 95% CI: − 1.23 to − 0.34) (Fig. 2a), FSG (MD: − 0.98, 95% CI: − 1.13 to − 0.54) (Fig. 2b), FSI (MD: − 2.47, 95% CI: − 3.99 to − 0.95) (Fig. 2c) and HbA1c% (MD: − 0.45, 95% CI: − 0.73 to − 0.16) (Fig. 2d).
The effects on lipid parameters
All of the enrolled trials have demonstrated the influence of lipid metabolism by TST. Among the total eight RCTs, four articles have reported a decrease in TC [21, 24, 27, 28], one demonstrated an increase in serum HDL levels and a reduction in serum LDL levels [21], one showed an increase in serum HDL levels and a decrease in TG [26]. The rest data all showed non-significant changes about lipid parameters.
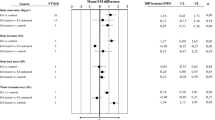
According to our meta-analyses, TST can result in a decline in TC (MD: − 0.29, 95% CI: − 0.38 to − 0.19) (Fig. 3a) and TG (MD: − 0.37, 95% CI: − 0.59 to − 0.15) (Fig. 3b). No significant differences were found in other lipid outcomes including HDL levels (MD: 0.01, 95% CI: − 1.03 to 1.04) (Fig. 3c) and LDL levels (MD: − 0.06, 95% CI: − 0.14 to 0.02) (Fig. 3d).
The effects on blood pressure, body fat percentages and BMI indexes
Blood pressure, body fat percentage and BMI indexes were reported in seven [19, 21, 23,24,25,26,27,28], three [19, 27, 28] and seven [19,20,21, 23,24,25, 27, 28] articles, respectively. According to existing trials, our meta-analyses suggested that TST cannot influence systolic (MD 0.13, 95% CI − 0.53 to 1.80) (Fig. 4a) or diastolic blood pressure (MD 0.01, 95% CI − 1.03 to 1.04) (Fig. 4b), body fat% (MD − 0.33, 95% CI − 0.92 to 0.26) (Fig. 4c) and BMI indexes (MD 0.29, 95% CI − 0.84 to 1.41) (Fig. 4d).
The effects on AMS and IIEF scores
Only two studies reported the AMS and IIEF scores in hypogonadal men with T2DM [22, 24]. Both trials showed a non-significant reduction in AMS in TST groups. For erectile function, two studies showed contradictory results. Hackett et al. demonstrated a significant increase in IIEF scores [24] while Gianatti et al. showed a significant decrease in IIEF scores [22].
Our meta-analyses showed a non-significant decrease in AMS (MD − 1.09, 95% CI − 3.85 to 1.67) and a non-significant increase in IIEF scores (MD 0.31, 95% CI − 6.06 to 6.68). More eligible studies were needed to clarify the effect on sexual function and AMS score.
Adverse events
No differences in adverse events were found between TST and placebo groups. The incidences of serious adverse events in TST groups were 9% [21], 1% [24], 7% [27] in three studies, whereas the other five studies did not report serious adverse events. Cardiovascular-related events were reported in two trials (TST group vs placebo group: 3 vs 3 [21] and 3 vs 7 [27]), and one study showed a trend for cardiovascular events to occur more frequently in the placebo group [27]. Compared with comparators, three studies [20, 21, 27] reported significant increases in hematocrit and one trial [21] reported an increase in PSA after TST.
Trial sequential analysis results
TSA results showed sufficient evidence that TST can reduce HOMA-IR (Fig. 5a), FSG (Fig. 5b), FSI (Fig. 5c), TC (Fig. 5e) and TG (Fig. 5f). However, analysis in HbA1c% showed a negative result (Fig. 5d), suggesting that potential inaccuracy might exist.
Sensitivity analysis
We performed sensitivity analyses to evaluate the influence of individual study on the pooled MDs. Our results demonstrated no alterations in pooled MDs after any study was excluded (Figure S3), indicating that no individual trial could significantly affect the pooled MDs. Accordingly, sensitivity analysis showed that our results were dependable.
Publication bias
Results of Egger’s tests showed no potential publication bias existed in all analyses (HOMA-IR P = 0.452; FSG P = 0.536; FSI P = 0.707; HbA1c P = 0.764; TC P = 1.000; TG P = 0.536; HDL P = 0.711; LDL P = 0.548; SBP P = 1.000; DBP P = 0.764; body fat P = 0.296; BMI P = 0.764). Moreover, evidence of obvious asymmetrical were not found in the funnel plots (Figure S4).
Discussion
A large amount of studies has reported the association between T2DM and hypogonadism. The morbidity of hypogonadism in patients with T2DM is higher than general population, which might be aroused from the activation of the insulin signaling pathway. Meanwhile, after TST, hypogonadal patients showed a marked increase in the expression of the major genes responsible for glucose transport mediating insulin signaling (IR-b, IRS-1, AKT-2, and GLUT4) [20]. According to the guidelines of European Association of Urology in 2017, TST is recommended for symptomatic hypogonadal men who are not considering parenthood. There are a number of potential clinical benefits with TST, including improvements in glycemic control, insulin resistance, muscle strength, increased lean mass, libido and erectile function [2, 40,41,42].
Our results showed that TST can significantly improve glucose control (by reducing HOMA-IR, FSG, FSI and HbA1c), which is consistent with several previous published studies [19,20,21, 26,27,28]. Noticeably, although TST can result in significant reduction in HbA1c% in meta-analysis, TSA results suggested potential random errors existed. In addition, a total of six studies calculated HOMA-IR in our meta-analysis. Among them, three used HOMA2 model [21, 25, 26], a more stringent computer-based equation in assessing insulin resistance. The model can better reflect human physiology and accounts for hepatic and peripheral glucose resistance. Subgroup analyses demonstrated that testosterone supplement therapy could decrease HOMA-IR assessed by HOMA1 model (MD − 1.11, 95% CI − 1.44 to − 0.77). However, the effect was not significant in HOMA2 based studies (MD − 0.51, 95% CI − 1.26 to 0.25). Factors which are captured by HOMA2 might be important causes for non-significant decrease in HOMA-IR in TRT groups. More studies were needed to clarify the influence on HbA1c% and HOMA-IR (assessed by HOMA2 model) by TST.
In terms of lipid parameters, TST can decrease the TC and TG levels in serum according to the current meta-analysis. Besides, results of TSA also showed a firm association between TST and reduction of TC and TG. However, although two trials demonstrated increase in serum HDL levels [21, 26] and one study showed a reduction in serum LDL level [21]. Our meta-analysis demonstrated no significant association between TST and changes of these parameters.
Several studies have demonstrated that serum testosterone concentrations are lower in men with poorly controlled T2DM than in healthy men. Unfortunately, little RCTs focused on the effect of TST in poorly controlled T2DM male patients [43]. Trials enrolled in this meta-analysis all had well controlled HbA1c% baselines (ranging from 6.9 to 7.5%), and the effects of TST in men with poorly controlled T2DM are still unknown. Further researches were needed to clarify the role of TST in these patients.
Metabolic syndrome (MetS) is a clustering of several conditions including abdominal (central) obesity, hypertension, elevated FSG, high TG and low HDL levels. The syndrome is associated with an increased risk of developing T2DM and male hypogonadism. An abundance of studies has shown that men with metabolic syndrome (MetS) have lower plasma testosterone levels [44]. Several RCTs and meta-analyses also demonstrated positive metabolic effects of TST on MetS patients, especially combined with hypogonadism [44,45,46,47]. Hypogonadal male patients with MetS without established T2DM can also benefit from testosterone treatment by a reduction of insulin resistance [46, 47].
In this meta-analysis, we have several advantages: (1) The sample size is larger than any single study, which made our results convinced. (2) The Egger’s tests showed no publication bias. (3) Sensitivity analyses showed there were no low-quality studies. (4) TSA was conducted for the first time in this study to estimate whether our results were sufficient. In addition, we compared the current meta-analysis with previous meta-analysis by Cai et al. which included five RCTs [48]. The cumulative Z-curve did not cross the trial sequential monitoring boundary and the total size of cases and controls were less than the estimated information size in the previous five RCTs, suggesting potential random errors existed. After including another three RCTs, the cumulative Z-curve crossed the monitoring boundaries, indicating that our results were based on firm evidence.
Despite the overall sufficient statistical evidence generated through this analysis, some limitations should also be emphasized. (1) Most populations included in our analysis were Caucasians, and other ethnicities, for example, the Asian and African will be required in future research to comprehensively evaluate the role of TST in hypogonadal patients with T2DM. (2) Only two or three RCTs analyzed body fat, AMS and IIEF scores, and more RCTs were needed to investigate the effect of TST on sexual function. (3) Adjusted estimates could not be performed in our analysis due to insufficient data for the adjustment by other covariates such as age and lifestyle. (4) In our meta-analysis, primary testosterone regimens were different in various included studies, which might induce potential inaccuracy. (5) Although TSA results showed that TST has a firm improvement in glucose control and reduction in TC and TG, more studies of high quality are required to offer more detailed individual data.
Conclusion
According to our meta-analysis, TST can improve glycemic control, and decrease TC and TG in hypogonadal patients with T2DM. We recommend TST during the anti-diabetic therapy in these patients. In addition, more RCTs of high quality are needed to explore other effects of TRT in hypogonadal men with T2DM.
References
Bhasin S, Cunningham GR, Hayes FJ, Matsumoto AM, Snyder PJ, Swerdloff RS, Montori VM (2010) Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 95:2536–2559. https://doi.org/10.1210/jc.2009-2354
Wang C, Nieschlag E, Swerdloff R, Behre HM, Hellstrom WJ, Gooren LJ, Kaufman JM, Legros JJ, Lunenfeld B, Morales A, Morley JE, Schulman C, Thompson IM, Weidner W, Wu FC (2009) Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl 30:1–9. https://doi.org/10.2164/jandrol.108.006486
Hall SA, Esche GR, Araujo AB, Travison TG, Clark RV, Williams RE, McKinlay JB (2008) Correlates of low testosterone and symptomatic androgen deficiency in a population-based sample. J Clin Endocrinol Metab 93:3870–3877. https://doi.org/10.1210/jc.2008-0021
Traish AM, Miner MM, Morgentaler A, Zitzmann M (2011) Testosterone deficiency. Am J Med 124:578–587. https://doi.org/10.1016/j.amjmed.2010.12.027
Li Y, Zhang M, Liu X, Cui W, Rampersad S, Li F, Lin Z, Yang P, Li H, Sheng C, Cheng X, Qu S (2017) Correlates and prevalence of hypogonadism in patients with early- and late-onset type 2 diabetes. Andrology 5:739–743. https://doi.org/10.1111/andr.12360
Corona G, Sforza A, Maggi M (2017) Testosterone replacement therapy: long-term safety and efficacy. World J Mens Health 35:65–76. https://doi.org/10.5534/wjmh.2017.35.2.65
Ng Tang Fui M, Hoermann R, Cheung AS, Gianatti EJ, Zajac JD, Grossmann M (2013) Obesity and age as dominant correlates of low testosterone in men irrespective of diabetes status. Andrology 1:906–912. https://doi.org/10.1111/j.2047-2927.2013.00124.x
Rezvani MR, Saadatjou SA, Sorouri S, Hassanpour Fard M (2012) Comparison of serum free testosterone, luteinizing hormone and follicle stimulating hormone levels in diabetics and non-diabetics men- a case-control study. J Res Health Sci 12:98–100
Rovira-Llopis S, Banuls C, de Maranon AM, Diaz-Morales N, Jover A, Garzon S, Rocha M, Victor VM, Hernandez-Mijares A (2017) Low testosterone levels are related to oxidative stress, mitochondrial dysfunction and altered subclinical atherosclerotic markers in type 2 diabetic male patients. Free Radic Biol Med 108:155–162. https://doi.org/10.1016/j.freeradbiomed.2017.03.029
Atlantis E, Fahey P, Martin S, O’Loughlin P, Taylor AW, Adams RJ, Shi Z, Wittert G (2016) Predictive value of serum testosterone for type 2 diabetes risk assessment in men. BMC Endocr Disord 16:26. https://doi.org/10.1186/s12902-016-0109-7
Xia JW, Tan SJ, Zhang XL, Jun T, Sun XK, Ling W (2015) Correlation of serum testosterone with insulin resistance in elderly male type 2 diabetes mellitus patients with osteoporosis. J Diabetes Investig 6:548–552. https://doi.org/10.1111/jdi.12291
Daka B, Langer RD, Larsson CA, Rosen T, Jansson PA, Rastam L, Lindblad U (2015) Low concentrations of serum testosterone predict acute myocardial infarction in men with type 2 diabetes mellitus. BMC Endocr Disord 15:35. https://doi.org/10.1186/s12902-015-0034-1
Corona G, Monami M, Rastrelli G, Aversa A, Sforza A, Lenzi A, Forti G, Mannucci E, Maggi M (2011) Type 2 diabetes mellitus and testosterone: a meta-analysis study. Int J Androl 34:528–540. https://doi.org/10.1111/j.1365-2605.2010.01117.x
Sheffield-Moore M (2000) Androgens and the control of skeletal muscle protein synthesis. Ann Med 32:181–186
Corona G, Rastrelli G, Morgentaler A, Sforza A, Mannucci E, Maggi M (2017) Meta-analysis of results of testosterone therapy on sexual function based on international index of erectile function scores. Eur Urol 72:1000–1011. https://doi.org/10.1016/j.eururo.2017.03.032
Nian Y, Ding M, Hu S, He H, Cheng S, Yi L, Li Y, Wang Y (2017) Testosterone replacement therapy improves health-related quality of life for patients with late-onset hypogonadism: a meta-analysis of randomized controlled trials. Andrologia. https://doi.org/10.1111/and.12630
Tracz MJ, Sideras K, Bolona ER, Haddad RM, Kennedy CC, Uraga MV, Caples SM, Erwin PJ, Montori VM (2006) Testosterone use in men and its effects on bone health. A systematic review and meta-analysis of randomized placebo-controlled trials. J Clin Endocrinol Metab 91:2011–2016. https://doi.org/10.1210/jc.2006-0036
Li HJ (2014) More attention should be paid to the treatment of male infertility with drugs–testosterone: to use it or not? Asian J Androl 16:270–273. https://doi.org/10.4103/1008-682x.122343
Boyanov MA, Boneva Z, Christov VG (2003) Testosterone supplementation in men with type 2 diabetes, visceral obesity and partial androgen deficiency. Aging Male 6:1–7
Dhindsa S, Ghanim H, Batra M, Kuhadiya ND, Abuaysheh S, Sandhu S, Green K, Makdissi A, Hejna J, Chaudhuri A, Punyanitya M, Dandona P (2016) Insulin resistance and inflammation in hypogonadotropic hypogonadism and their reduction after testosterone replacement in men with type 2 diabetes. Diabetes Care 39:82–91. https://doi.org/10.2337/dc15-1518
Gianatti EJ, Dupuis P, Hoermann R, Strauss BJ, Wentworth JM, Zajac JD, Grossmann M (2014) Effect of testosterone treatment on glucose metabolism in men with type 2 diabetes: a randomized controlled trial. Diabetes Care 37:2098–2107. https://doi.org/10.2337/dc13-2845
Gianatti EJ, Dupuis P, Hoermann R, Zajac JD, Grossmann M (2014) Effect of testosterone treatment on constitutional and sexual symptoms in men with type 2 diabetes in a randomized, placebo-controlled clinical trial. J Clin Endocrinol Metab 99:3821–3828. https://doi.org/10.1210/jc.2014-1872
Gopal RA, Bothra N, Acharya SV, Ganesh HK, Bandgar TR, Menon PS, Shah NS (2010) Treatment of hypogonadism with testosterone in patients with type 2 diabetes mellitus. Endocr Pract 16:570–576. https://doi.org/10.4158/ep09355
Hackett G, Cole N, Bhartia M, Kennedy D, Raju J, Wilkinson P (2013) Testosterone replacement therapy with long-acting testosterone undecanoate improves sexual function and quality-of-life parameters vs. placebo in a population of men with type 2 diabetes. J Sex Med 10:1612–1627. https://doi.org/10.1111/jsm.12146
Hackett G, Cole N, Bhartia M, Kennedy D, Raju J, Wilkinson P (2014) Testosterone replacement therapy improves metabolic parameters in hypogonadal men with type 2 diabetes but not in men with coexisting depression: the BLAST study. J Sex Med 11:840–856. https://doi.org/10.1111/jsm.12404
Heufelder AE, Saad F, Bunck MC, Gooren L (2009) Fifty-two-week treatment with diet and exercise plus transdermal testosterone reverses the metabolic syndrome and improves glycemic control in men with newly diagnosed type 2 diabetes and subnormal plasma testosterone. J Androl 30:726–733. https://doi.org/10.2164/jandrol.108.007005
Jones TH, Arver S, Behre HM, Buvat J, Meuleman E, Moncada I, Morales AM, Volterrani M, Yellowlees A, Howell JD, Channer KS (2011) Testosterone replacement in hypogonadal men with type 2 diabetes and/or metabolic syndrome (the TIMES2 study). Diabetes Care 34:828–837. https://doi.org/10.2337/dc10-1233
Kapoor D, Goodwin E, Channer KS, Jones TH (2006) Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol 154:899–906. https://doi.org/10.1530/eje.1.02166
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(264–269):w264
Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 340:c869. https://doi.org/10.1136/bmj.c869
Pogue JM, Yusuf S (1997) Cumulating evidence from randomized trials: utilizing sequential monitoring boundaries for cumulative meta-analysis. Control Clin Trials 18:580–593 (discussion 661–586)
Pogue J, Yusuf S (1998) Overcoming the limitations of current meta-analysis of randomised controlled trials. Lancet 351:47–52. https://doi.org/10.1016/s0140-6736(97)08461-4
Thorlund K, Devereaux PJ, Wetterslev J, Guyatt G, Ioannidis JP, Thabane L, Gluud LL, Als-Nielsen B, Gluud C (2009) Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int J Epidemiol 38:276–286. https://doi.org/10.1093/ije/dyn179
Zhang J, Xiao L, Qin Z, Xu A, Zhao K, Liang C, Miao C, Zhu J, Chen W, Hua Y, Liu Y, Zhang C, Yu Y, Su S, Wang Z (2016) Association between germline homeobox B13 (HOXB13) G84E allele and prostate cancer susceptibility: a meta-analysis and trial sequential analysis. Oncotarget 7:67101–67110. https://doi.org/10.18632/oncotarget.11937
Li X, Shen M, Cai H, Liu K, Liu Y, Huang Z, Liang C, Deng X, Ye J, Zou Q, Li J (2016) Association between manganese superoxide dismutase (MnSOD) polymorphism and prostate cancer susceptibility: a meta-analysis. Int J Biol Markers 31:e422–e430. https://doi.org/10.5301/jbm.5000188
Chen P, Li X, Sang L, Huang J (2017) Perioperative intravenous glucocorticoids can decrease postoperative nausea and vomiting and pain in total joint arthroplasty: a meta-analysis and trial sequence analysis. Medicine 96:e6382. https://doi.org/10.1097/md.0000000000006382
Yang L, Wang G, Du Y, Ji B, Zheng Z (2014) Remote ischemic preconditioning reduces cardiac troponin I release in cardiac surgery: a meta-analysis. J Cardiothorac Vasc Anesth 28:682–689. https://doi.org/10.1053/j.jvca.2013.05.035
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
DerSimonian R, Kacker R (2007) Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 28:105–114. https://doi.org/10.1016/j.cct.2006.04.004
Marin P, Krotkiewski M, Bjorntorp P (1992) Androgen treatment of middle-aged, obese men: effects on metabolism, muscle and adipose tissues. Eur J Med 1:329–336
Tuck SP, Francis RM (2009) Testosterone, bone and osteoporosis. Front Horm Res 37:123–132. https://doi.org/10.1159/000176049
Brinkmann AO (2011) Molecular mechanisms of androgen action–a historical perspective. Methods Mol Biol 776:3–24. https://doi.org/10.1007/978-1-61779-243-4_1
Kim KS, Kang SH, Kim MJ, Kim SK, Kim YL, Park WK, Park SW, Cho YW (2014) Low serum testosterone concentrations in hospitalized men with poorly controlled type 2 diabetes. Endocrinol Metab 29:574–578. https://doi.org/10.3803/EnM.2014.29.4.574
Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F, Lenzi A, Forti G, Mannucci E, Maggi M (2011) Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med 8:272–283. https://doi.org/10.1111/j.1743-6109.2010.01991.x
Grossmann M, Hoermann R, Wittert G, Yeap BB (2015) Effects of testosterone treatment on glucose metabolism and symptoms in men with type 2 diabetes and the metabolic syndrome: a systematic review and meta-analysis of randomized controlled clinical trials. Clin Endocrinol 83:344–351. https://doi.org/10.1111/cen.12664
Kalinchenko SY, Tishova YA, Mskhalaya GJ, Gooren LJ, Giltay EJ, Saad F (2010) Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: the double-blinded placebo-controlled Moscow study. Clin Endocrinol 73:602–612. https://doi.org/10.1111/j.1365-2265.2010.03845.x
Aversa A, Bruzziches R, Francomano D, Rosano G, Isidori AM, Lenzi A, Spera G (2010) Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 24-month, randomized, double-blind, placebo-controlled study. J Sex Med 7:3495–3503. https://doi.org/10.1111/j.1743-6109.2010.01931.x
Cai X, Tian Y, Wu T, Cao CX, Li H, Wang KJ (2014) Metabolic effects of testosterone replacement therapy on hypogonadal men with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Asian J Androl 16:146–152. https://doi.org/10.4103/1008-682x.122346
Acknowledgements
This work is supported by the grant from National Natural Science Foundation of China (81370698 and 81671488) and Beijing Natural Science Foundation (Grant No. 7162152).
Funding
This study was funded by National Natural Science Foundation of China (81370698 and 81671488) and Beijing Natural Science Foundation (Grant No. 7162152).
Author information
Authors and Affiliations
Contributions
HJL project development and manuscript writing. JZZ data collection and manuscript writing. BY data collection and data analysis. WHX data collection. XL data analysis.
Corresponding author
Ethics declarations
Conflict of interest
Hongjun Li has received research grants from National Natural Science Foundation of China (81370698 and 81671488) and Beijing Natural Science Foundation (Grant No. 7162152).
Research involving Human Participants and/or Animals
Human participants For this type of study formal consent is not required. Animals This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
345_2018_2256_MOESM3_ESM.tif
Sensitivity of each included study in this meta-analysis. A-L indicated sensitivity analyses of HOMA-IR, FSG, FSI, HbA1c, TC, TG, HDL, LDL, SBP, DBP, body fat and BMI indexes, respectively. 3 (TIFF 1159 kb)
345_2018_2256_MOESM4_ESM.tif
Begg’s funnel plots of the publication bias. A-L indicated funnel plots of HOMA-IR, FSG, FSI, HbA1c, TC, TG, HDL, LDL, SBP, DBP, body fat and BMI indexes, respectively. 4 (TIFF 573 kb)
Rights and permissions
About this article
Cite this article
Zhang, J., Yang, B., Xiao, W. et al. Effects of testosterone supplement treatment in hypogonadal adult males with T2DM: a meta-analysis and systematic review. World J Urol 36, 1315–1326 (2018). https://doi.org/10.1007/s00345-018-2256-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2256-0