Abstract
Purpose
According to the current guidelines, computed tomography (CT) and bone scintigraphy (BS) are optional in intermediate-risk and recommended in high-risk prostate cancer (PCa). We wonder whether it is time for these examinations to be dismissed, evaluating their staging accuracy in a large cohort of radical prostatectomy (RP) patients.
Methods
To evaluate the ability of CT to predict lymph node involvement (LNI), we included 1091 patients treated with RP and pelvic lymph node dissection, previously staged with abdomino-pelvic CT. As for bone metastases, we included 1145 PCa patients deemed fit for surgery, previously staged with Tc-99m methylene diphosphonate planar BS.
Results
CT scan showed a sensitivity and specificity in predicting LNI of 8.8 and 98 %; subgroup analysis disclosed a significant association only for the high-risk subgroup of 334 patients (P 0.009) with a sensitivity of 11.8 % and positive predictive value (PPV) of 44.4 %. However, logistic multivariate regression analysis including preoperative risk factors excluded any additional predictive ability of CT even in the high-risk group (P 0.40). These data are confirmed by ROC curve analysis, showing a low AUC of 54 % for CT, compared with 69 % for Partin tables and 80 % for Briganti nomogram. BS showed some positivity in 74 cases, only four of whom progressed, while 49 patients with negative BS progressed during their follow-up, six of them immediately after surgery.
Conclusions
According to our opinion, the role of CT and BS should be restricted to selected high-risk patients, while clinical predictive nomograms should be adopted for the surgical planning.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most common cancer in men and the second most common cause of death from tumors in the male population [1]. With the beginning of the PSA era, the early diagnosis of PCa has been made possible, widening the opportunities for local radical therapies such as RP or radiation therapy (RT). However, the scenario changes when PCa spreads to the lymph nodes or to the bone, becoming a systemic disease: In these cases, the opportunity window for a radical therapy is lost, although surgery and radiotherapy are progressively achieving a role in selected N + PCa patients [2–4]. A correct staging is therefore essential to properly focus the disease we are dealing with, and consequentially to decide the most appropriate treatment. Nowadays, computed tomography (CT) and bone scintigraphy (BS) are the imaging examinations commonly used in PCa for staging nodal and bone involvement, respectively. According to the current guidelines, these examinations are optional in intermediate-risk and recommended in high-risk PCa [5, 6]. However, their use has been questioned by several studies reporting a limited staging ability for both the procedures. In particular, BS is deeply influenced by PSA level and Gleason score [7], while the accuracy of CT scan has been shown to be really poor, even in those patients with a very high risk of nodal metastases [8]. Recently, whole-body magnetic resonance imaging (MRI) was shown to be more sensitive and specific than the combination of BS, targeted radiographs and abdomino-pelvic CT [9, 10], suggesting an “all-in-one” staging approach. Preoperative clinical models, such as Partin [11] or Briganti nomograms [12], have been adopted in the preoperative risk assessment of PCa for lymph node involvement (LNI), and showed possibly more appropriate and accurate than CT itself to decide for the need of pelvic lymph node dissection (PLND). All these things considered, we wonder whether it is time for BS and CT to be dismissed, or if they still have a role in the PCa staging. We tried to find an answer by evaluating their accuracy as staging examinations in a large cohort of RP patients.
Materials and methods
Patient population
Under institutional review board supervision, data from men who underwent RP between 1999 and 2012 with at least 2-year follow-up available (PSA records and clinical visits) at thirteen Italian Urology Departments located in Piedmont and Aosta Valley Italian regions were combined into the EUREKA-1 database. EUREKA-1 is an observational, multicentric, retrospectively derived dataset promoted by the CHIC project (sponsored by the European Union, 7th Framework Program, grant agreement no. 600841); it was approved by the Ethical Committee of FPO-IRCCS Cancer Center of Candiolo in July 2013 and amended in November 2014; data collected in EUREKA-1 included socio-demographic parameters, clinical tumor characteristics, surgery features, pathology, therapies, clinical and PSA follow-ups, and clinical outcomes.
To evaluate the ability of CT to predict LNI, we included 1091 patients treated with RP and PLND. All the patients were staged before surgery with abdomino-pelvic contrast-enhanced CT scan; CT was considered positive for LNI if at least one node had a short-axis diameter ≥10 mm [8]. CT technology greatly varied during the 14-year-long period under study. The CT devices used were: Philips Tomoscan AV (single detector row), Elscint Twin (2 slices), Philips Brilliance (6 slices), Toshiba Aquilion (16 slices), Philips Brilliance (40 slices), Philips Brilliance (64 slices), GE Discovery (64 slices), with slice thickness ranging in between 7 and 2 mm.
Following RP and PLND, the resected nodes were deemed positive for LNI if PCa metastases were found at the pathology examination (i.e., macro-metastases ≥2 mm or micro-metastases <2 mm [13]); finally, pathologic results were compared with CT findings.
Besides, patients were stratified according to the D’Amico clinical (preoperative) risk classification in low-, intermediate- and high-risk groups [14].
As for bone metastases, we included 1145 PCa patients scheduled for surgery, staged with planar total-body Tc-99m methylene diphosphonate BS. Most of the patients with positive or equivocal findings underwent targeted X-rays or MRI for confirmation. We looked only for false-positive and false-negative rates, considering that all patients successively underwent surgery.
Standard follow-up included PSA dosage and DRE every 3 months for 2 years, every 6 months until the fifth year and annually thereafter. Patients with clinical and/or serological suspect of bone metastasis at follow-up (i.e., fast severe arousal of post-prostatectomy PSA or clinical symptoms) underwent BS (and/or CT and/or MRI looking for osteoblastic metastases or secondary fractures) for radiologic confirmation.
Statistical analysis
Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were tested, and related P values were calculated with Chi-square test. Discrimination accuracy was assessed using the C-statistics of the ROC area under the curve (AUC). The overall accuracy of Partin and Briganti nomograms for LNI was assessed too. Univariate and multivariate logistic regression analyses tested the relationships between CT findings and LNI. Covariates consisted of preoperative PSA, clinical stage and bioptic Gleason score.
P values were considered statistically significant if <0.05. All statistical analyses were performed using SAS Foundation 9.3 (SAS Institute, Cary, NC, USA).
Results
The characteristics of the 1091 CT-staged patients are listed in Table 1. Overall, LNI was detected in 102 patients (9.3 %). CT scan was suggestive of LNI in 29 patients (2.7 %); of them, only 9 (31 %) had histologically proven LNI at PLND. False positives were found in 20 patients and false negatives in 93. Sensitivity (Se), specificity (Sp), PPV and NPV in predicting LNI for the whole cohort were 8.8, 98.0, 31.0 and 91.2 %, respectively.
Subgroup analysis disclosed a significant association only for the high-risk subgroup of 334 patients (P 0.009) with a Se 11.8 %, Sp 96.2 %, PPV 44.4 % and NPV 81.0 % (Table 2).
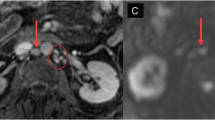
Of consequence, we further compared the CT predictive ability with clinical risk factors in the high-risk group only. Logistic multivariate regression analysis including CT finding and PSA value, bioptic Gleason score and clinical staging left out any significant additional predictive ability of CT (P value of 0.40; see Table 3). These data were further confirmed by AUC analysis of the ROC curves in the high-risk group, showing a low overall accuracy of 54 % for CT, compared with 69 % for Partin tables and 80 % for Briganti nomogram (Fig. 1).
Regarding BS, patients’ features are given in Table 4. BS was performed in 1145 patients (192 low-risk, 567 intermediate-risk and 386 high-risk), deemed fit for surgery after clinical and/or further radiologic examinations (targeted X-rays or MRI). Among them, BS showed some positivity in 74 cases; only four of them developed bone metastases successively, after an average of 27.5 months from surgery (PPV 5.4 %). Finally, 49 patients with negative scintigraphy developed bone metastases during their follow-up (NPV 95.4 %), six of them within 6 months after surgery.
Discussion
Historically, abdomino-pelvic CT scan and BS played an important role as staging procedures in PCa patients, to rule out any extra-prostatic presence of disease. As the risk of nodal or bone metastases has been associated with bad clinical features such as elevated PSA, high clinical stage and poor tumor differentiation, CT and BS use has been confined to the cases at higher risk, namely some of the intermediate-risk and all of the high-risk PCa [5, 7, 11–15]. In the last years, however, their role has been strongly questioned, as a poor staging ability has been demonstrated for both procedures [7–10, 16, 17]. Nevertheless, despite the criticism of the scientific community, the last EAU guidelines still recommend both CT and scintigraphy performance for selected groups of PCa patients [5]. Following the lead of previous studies [7, 8, 16], we therefore decided to assess the usefulness of these examinations as predictors of LNI/bone metastases in our retrospective series of patients collected in the Eureka-1 database.
In 2008, a comprehensive meta-analysis on 1024 patients warned about the poor performance of presurgical CT in the detection of lymph node metastases: Pooled sensitivity and specificity were 0.42 and 0.82, respectively. The authors discredited the use of CT, concluding that it misrepresented the true nodal metastases involvement, thus misdirecting the therapeutic strategies offered to the patient [16]. Another study focusing on patients at high-risk of locally advanced disease had already shown a low accuracy of CT even in this high-risk group, with consequences on the correct treatment choice [17]. More recently, Briganti et al. [8] evaluated a single-center, homogeneous series of 1541 patients undergoing RP and extended PLND, all preoperatively staged with CT scan. Including only patients who received a standardized anatomically defined PLND, their study overcame the false-negative results due to a limited PLND. According to their results, sensitivity, specificity and accuracy of CT scan were 13, 96 and 54.6 %, respectively. Again, their conclusions deposed against the use of CT scan to decide on the need for, or extent of PLND in patients with PCa. In our analysis, the performance of CT was confirmed to be very poor, with low sensitivity and accuracy of 11.8 and 54 % even in the high-risk group.
The limited sensitivity of CT is due to its inability in detecting micro-metastases: A threshold of 10 mm in the short-axis nodal diameter for oval nodes and 8 mm for round nodes are used as criteria for the diagnosis of lymph node metastases [18], but such accuracy is obviously far inadequate to detect smaller metastases. On the contrary, the risk of false positives due to reactive lymph nodes needs to be taken into account, considering the 20 false-positive cases in our series.
To overcome the limitations of the available imaging techniques, several nomograms or predictive models have been proposed to assess the risk of LNI, such as Briganti or Partin tools [11, 12]. Both these nomograms have shown a very high accuracy for the LNI prediction (up to 88 %), and they are currently an important input for the decision-making process driving the choice to perform PLND. It has already been suggested that such preoperative clinical models should completely replace the imaging procedures in the assessment of the risk of LNI [8]. Interestingly, our study confirmed in the high-risk cohort a good discrimination accuracy for Briganti nomogram (80 %), but not so high for Partin model (69 %).
Maybe, the imaging predictive capability will improve with the progressive replacement of CT by multiparametric MRI, which is the gold standard for prostate imaging, and of planar BS with the more specific SPECT–CT BS [19]. However, CT and MRI performances are currently similarly poor compared with histologic diagnosis [20], even if soon iron oxide particles should enhance the detection of enlarged lymph nodes [10, 21]. Up to date, choline PET and PET–CT have also provided low sensitivity (49.2 %) in the detection of lymph node metastases prior to surgery in PCa patients [22].
As for bone metastases detection, the sensitivity of BS completed with targeted X-rays has been shown to be 86 %, with a 98 % specificity [10]. According to a recently developed prognostic tool, staging bone scans might be considered only for patients with a biopsy Gleason score >7, or with a PSA > 10 ng/ml and palpable disease (cT2/T3) prior to treatment. Such an approach would avoid the use of staging bone scans in about 81 % of the patients with a NPV of 99.6 % [23]. On the basis of these results, the recent guidelines recommend bone scan in asymptomatic patients only if the PSA level >10 ng/ml or Gleason score ≥8 or clinical stage ≥T3, namely the intermediate- and high-risk situation [5, 6]. However, even if the indications are restricted accordingly, a considerable number of performed bone scans are unnecessary. In our analysis, we could not evaluate the sensitivity and specificity of bone scan, as our cohort was composed of patients deemed fit to undergo RP, and so excluding all the patients positive to bone scan and treated primarily with medical therapy, i.e., androgen deprivation therapy. Nevertheless, we thought interesting to report the low accuracy of BS in our series, where 74 cases initially found positive were successively cleared for surgery, whereas six cases already harboring bone metastases were not detected.
Our study does have several limitations, mainly due to the selection criteria of our database, the heterogeneousness of the cohort and the retrospective nature of our data.
The main issue is inherent to our database, consisting in a population of men having been deemed fit for surgery; this criterion introduces substantial selection bias (i.e., men found to harbor metastatic disease and not eligible for RP, or who underwent primary RT instead of RP); this trouble is more relevant for BS than for CT, and so data collected on RP patients are inadequate to perform a proper evaluation of the accuracy of BS. A second limitation regarding bone scan is the lack of histologic confirmation from bone biopsy specimens; nevertheless, the long follow-up of our series allowed us to assess which patients harbored bone metastases not discovered during the preoperatory staging. Furthermore, the staging imaging procedures were performed by different physicians and with different equipments without any central review. One final limitation is related to the PLND template, which was not anatomically defined as recently recommended [8]: after all, the recommendations about the extension of PLND have changed several times in the last 15 years. PLND extension and template varied significantly between the participating urology divisions, while no statistical trend was identified in the mean number of nodes resected according to preoperatory D’Amico risk class (14 vs. 12.5 vs. 13.5 nodes in low-, intermediate- and high-risk classes, respectively). On the other hand, our retrospective data provide a snapshot about the usefulness of PCa staging examinations in a vast region of Italy over a 15-year period.
According to our findings, these examinations have only a minor effect on the correct diagnostic and therapeutic strategy. Of consequence, we advise to stage patients with CT just if they belong to high-risk category (i.e., PSA > 20 ng/ml or GS ≥ 8 or clinical stage ≥cT2c) and no functional MRI or CT–PET scan is available; this result is in agreement with AUA recommendations recently reported by Risko et al. [24].
Besides, bone scan too may be considered useful in the high-risk group only, so to decrease in lower-risk classes the incidence of misleading false-positive examinations, which can hamper or delay the choice of a radical therapy. In addition, a negative impact of a widespread use of these radiologic examinations on healthcare costs should be taken into account.
Conclusions
Our study confirms the poor accuracy of CT scan and BS as staging examinations for PCa. Their role should be restricted to selected high-risk cases, whereas their avoidance as routine examinations would simplify the diagnostic work-flow and save resources and money for the National Health Systems. As previously suggested in the literature, clinical predictive nomograms about lymph node involvement are more reliable to plan the best surgical therapeutic strategy.
References
DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL et al (2014) Cancer treatment and survivorship statistics, 2014. CA Cancer J Clin 64(4):252–271
Oderda M, Joniau S, Spahn M, Gontero P (2012) Debulking surgery in the setting of very high-risk prostate cancer scenarios. BJU Int 110(6 Pt B):E192–E198
Garibaldi E, Cattari G, Gabriele D, Delmastro E, Carau B, Cutaia C et al (2013) A personalized treatment with image-guided intensity modulated radiotherapy for high-very high risk and metastatic prostate cancer patients: preliminary results. Trends Cancer Res 9:33–42
Bresciani S, Garibaldi E, Cattari G, Maggio A, Di Dia A, Delmastro E et al (2013) Dose to organs at risk in the upper abdomen in patients treated with extended fields by helical tomotherapy: a dosimetric and clinical preliminary study. Radiat Oncol 8:247
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, European Association of Urology et al (2014) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol 65(1):124–137
Mohler JL, Kantoff PW, Armstrong AJ, Bahnson RR, Cohen M, D’Amico AV, National Comprehensive Cancer Network et al (2014) Prostate cancer, version 2.2014. J Natl Compr Cancer Netw 12(5):686–718
Zacho HD, Barsi T, Mortensen JC, Mogensen MK, Bertelsen H, Josephsen N et al (2014) Prospective multicenter study of bone scintigraphy in consecutive patients with newly diagnosed prostate cancer. Clin Nucl Med 39(1):26–31
Briganti A, Abdollah F, Nini A, Suardi N, Gallina A, Capitanio U et al (2012) Performance characteristics of computed tomography in detecting lymph node metastases in contemporary patients with prostate cancer treated with extended pelvic lymph node dissection. Eur Urol 61(6):1132–1138
Pasoglou V, Larbi A, Collette L, Annet L, Jamar F, Machiels J-P et al (2014) One-step TNM staging of high-risk prostate cancer using magnetic resonance imaging (MRI): toward an upfront simplified ‘all-in-one’ imaging approach? Prostate 74(5):469–477
Lecouvet FE, El Mouedden J, Collette L, Coche E, Danse E, Jamar F et al (2012) Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace Tc 99m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer? Eur Urol 62(1):68–75
Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD (2001) Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology 58(6):843–848
Briganti A, Larcher A, Abdollah F, Capitanio U, Gallina A, Suardi N et al (2012) Updated nomogram predicting lymph node invasion in patients with prostate cancer undergoing extended pelvic lymph node dissection: the essential importance of percentage of positive cores. Eur Urol 61(3):480–487
Isebaert S, Haustermans K, Van den Bergh L, Joniau S, Dirix P, Oyen R et al (2013) Identification and characterization of nodal metastases in prostate cancer patients at high risk for lymph node involvement. Acta Oncol 52(7):1336–1344
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA et al (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280(11):969–974
Haese A, Epstein JI, Huland H, Partin AW (2002) Validation of a biopsy-based pathologic algorithm for predicting lymph node metastases in patients with clinically localized prostate carcinoma. Cancer 95(5):1016–1021
Hövels AM, Heesakkers RAM, Adang EM, Jager GJ, Strum S, Hoogeveen YL et al (2008) The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis. Clin Radiol 63(4):387–395
Borley N, Fabrin K, Sriprasad S, Mondaini N, Thompson P, Muir G et al (2003) Laparoscopic pelvic lymph node dissection allows significantly more accurate staging in ‘high-risk’ prostate cancer compared to MRI or CT. Scand J Urol Nephrol 37(5):382–386
Jager GJ, Barentsz JO, Oosterhof GO, Witjes JA, Ruijs SJ (1996) Pelvic adenopathy in prostatic and urinary bladder carcinoma: MR imaging with a three-dimensional TI-weighted magnetization-prepared-rapid gradient-echo sequence. AJR Am J Roentgenol 167(6):1503–1507
McLoughlin LC, O’Kelly F, O’Brien C, Sheikh M, Feeney J, Torreggiani W et al (2014) The improved accuracy of planar bone scintigraphy by adding single photon emission computed tomography (SPECT-CT) to detect skeletal metastases from prostate cancer. Ir J Med Sci. doi:10.1007/s11845-014-1228-7
Giannarini G, Petralia G, Thoeny HC (2012) Potential and limitations of diffusion-weighted magnetic resonance imaging in kidney, prostate, and bladder cancer including pelvic lymph node staging: a critical analysis of the literature. Eur Urol 61(2):326–340
Dickinson L, Ahmed HU, Allen C, Barentsz JO, Carey B, Futterer JJ et al (2011) Magnetic resonance imaging for the detection, localisation, and characterisation of prostate cancer: recommendations from a European consensus meeting. Eur Urol 59(4):477–494
Evangelista L, Guttilla A, Zattoni F, Muzzio PC, Zattoni F (2013) Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate- to high-risk prostate cancer: a systematic literature review and meta-analysis. Eur Urol 63(6):1040–1048
Briganti A, Passoni N, Ferrari M, Capitanio U, Suardi N, Gallina A et al (2010) When to perform bone scan in patients with newly diagnosed prostate cancer: external validation of the currently available guidelines and proposal of a novel risk stratification tool. Eur Urol 57(4):551–558
Risko R, Merdan S, Womble PR, Barnett C, Ye Z, Linsell SM et al (2014) Clinical predictors and recommendations for staging computed tomography scan among men with prostate cancer. Urology 84(6):1329–1334
Authors’ contributions
Gabriele D involved in project development, data collection and data management. Collura D, Fiorito C, Porpiglia F, Terrone C and Zacchero M involved in data collection. Oderda M and Stura I involved in data management. Guiot C and Gabriele P involved in project development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical standard
EUREKA-1 study was approved by the Ethical Committee of FPO-IRCCS Cancer Center of Candiolo in July 2013 and amended in November 2014.
Rights and permissions
About this article
Cite this article
Gabriele, D., Collura, D., Oderda, M. et al. Is there still a role for computed tomography and bone scintigraphy in prostate cancer staging? An analysis from the EUREKA-1 database. World J Urol 34, 517–523 (2016). https://doi.org/10.1007/s00345-015-1669-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1669-2