Abstract
Purpose
In this retrospective study, we compared the diagnostic value of 68Gallium prostate-specific membrane antigen positron emission tomography computed tomography ([68Ga]PSMA PET/CT) in primary staging of patients with high-risk prostate cancer (PCa), in comparison to CT, magnetic resonance imaging (MRI), and bone scans, and we explored its overall impact on patients’ management plan.
Procedures
Patients with pathological confirmation of PCa with high-risk disease were included in this study. Information on patient demographics, clinical and histopathological findings with Gleason score and initial prostate specific antigen PSA levels, and radiological findings for CT, MRI, bone scan, and [68Ga]PSMA PET/CT were retrieved. We stratified the concordance and discordance of each imaging modality on per-patient and per-lesion-site bases.
Results
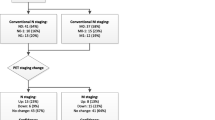
Twenty-one patients with high-risk disease were included in this study. [68Ga]PSMA PET/CT revealed a significantly higher concordance rate (90 %) compared to the concordance rates of bone scan (75 %), MRI (73 %), and CT (60 %). [68Ga]PSMA PET/CT had a similar accuracy to MRI in detecting prostate lesions but a higher accuracy for suspicious pelvic lymph nodes (95.2 % vs. 80 %). It also superseded CT scan in detecting suspicious pelvic lymph nodes (95.2 % vs. 75 %) and extra-pelvic lymph nodes (100 % vs. 75 %), as well as bone lesions via bone scan (100 % vs. 62.5 %). [68Ga]PSMA PET/CT changed the management in 11 patients (52 %).
Conclusions
[68Ga]PSMA PET/CT is an invaluable imaging modality in the assessment of primary high-risk PCa with great potential for the detection of lymph node spread and bone metastases that would impact the management plan.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most common solid malignancy in men and the third leading cause of cancer-related death in Western Europe and the USA [1, 2]. Diagnosis of PCa is mainly performed by histopathology following prostate biopsy, after which patients are stratified into distinct risk groups (low-, intermediate-, and high-risk) according to serum prostate-specific antigen (PSA) levels and Gleason scores [3].
Given that metastatic spread is unlikely in patients with low-risk PCa, current guidelines from the European Association of Urology and the National Comprehensive Cancer Network recommend that intermediate- and high-risk patients undergo x-ray computed tomography (CT) or magnetic resonance imaging (MRI) of the lower abdomen accompanied by bone scintigraphy [4, 5]. More recently, positron emission tomography (PET) probes that target prostate-specific membrane antigen (PSMA, also known as glutamate carboxypeptidase-2) for imaging PCa has gained increased interest and has shown great promise for improving the management of patients with PCa.
Although [68Ga]PSMA PET/CT was only recently introduced to clinical practice, several reports have demonstrated a clear superiority in terms of sensitivity, specificity, and diagnostic accuracy in large numbers of patients with recurrent PCa compared to conventional imaging for detection of biochemical recurrence [6,7,8]. Not only has [68Ga]PSMA become a valuable diagnostic agent in detecting recurrent PCa, but it has also become an invaluable tool in the assessment of response to therapy [9].
Despite this clear superiority of [68Ga]PSMA PET/CT in recurrent PCa, its potential role in primary staging of patients with intermediate- and high-risk PCa has been explored in only a small number of studies [10, 11]. In this study, we compare the diagnostic value of [68Ga]PSMA PET/CT in primary staging of patients with PCa, in comparison to CT, MRI, and bone scans, and we explore its overall impact on the management plan.
Methods
Study Population and Data Analysis
[68Ga]PSMA PET/CT has been offered at the King Hussein Cancer Center (KHCC) to patients with intermediate- and high-risk PCa for primary staging purposes, particularly if they have equivocal findings on conventional imaging. Between January 2015 and January 2018, a total of 35 patients received [68Ga]PSMA PET/CT for primary staging purposes. All patients gave informed consent to undergo [68Ga]PSMA PET/CT.
This study was approved by the Institutional Review Board (IRB) at our center. After going through patients’ online medical records, patients who have pathological confirmation of PCa (including a Gleason score), with high-risk disease according to D’Amico criteria [12], and those who had their full workup done at our center and without any prior medical or surgical treatments were included in this study. Twenty-one patients met these inclusion criteria. With regard to D’Amico criteria, the highest value among the variables was considered for risk stratification purposes (e.g., if a patient had Gleason score of seven and an initial PSA (iPSA) level of 35 ng/ml, the patient was classified as high-risk).
Using a pre-designed case report form, we retrieved the following information: patient demographics; clinical and histopathological findings with Gleason score and iPSA levels; and radiological findings for CT, MRI, bone scan, and [68Ga]PSMA PET/CT stratified according to T, N, and M categories. Treatment plans before and after [68Ga]PSMA PET/CT results were recorded as per the multi-disciplinary committee (MDC) decisions.
The role of [68Ga]PSMA PET/CT in treatment was then analyzed in relation to initial clinical and radiological findings, along with MDC decisions and follow-up radiological and clinical data. A subsequent analysis stratified concordance and discordance of each imaging modality on a per-patient basis (taking into account the overall staging) and a per-lesion-site basis (involving five main regions: prostate gland (PG), pelvic lymph nodes, extra-pelvic lymph nodes, bone lesions, and soft tissue lesions—namely liver and lung).
PSMA Ligand and [68Ga]PSMA PET/CT Imaging
[68Ga]PSMA-11 was radiolabeled with Ga-683+ from a Ge-68/Ga-68 generator system (ITG Isotope Technologies Garching GmbH, München, Germany) using a manual synthesis module. PET/CT scan was obtained with intravenous administration of [68Ga]PSMA (3 MBq/kg). Directly prior to the PET/CT scan, patients were asked to empty their bladder to minimize tracer accumulation. Standard whole-body [68Ga]PSMA PET/CT images extending from the vertex to toes were obtained 60 min after administration of radioisotope. Sometimes, additional images extending from upper abdominal quadrant to the mid-thighs (3 h delay images) were performed upon the request of a nuclear medicine physician after the assessment of early imaging, particularly if there were suspicious low- or moderate-levels of radiotracer uptake in suspicious lesions or questionable variant (likely-physiologic) radiotracer uptake, in order to exclude genuine lesions (such as focal uptake in ureters or bowels). Delayed imaging was acquired in nine patients from our cohort.
Axial, sagittal, and coronal PET reconstruction were interpreted with and without attenuation correction. Corresponding CT images without intravenous (IV) contrast were also acquired in a Biograph™ mCT flow 64 slices CT, reconstructed in axial, sagittal, and coronal planes, and reviewed alongside the PET images. The CT images were used for attenuation correction and anatomical correlation of the PET images. Patients’ weights were measured routinely before IV administration of radioisotope.
Image Interpretation
CT and MRI scans were interpreted by a radiologist at KHCC. Bone scans and [68Ga]PSMA PET/CT were each interpreted by a consensus read of two nuclear medicine physicians. Maximum intensity projection (MIP) images were evaluated with different intensity scales, after which images were displayed side-by-side. CT was used to determine the location of different lesions. A PET-positive lesion was identified as such when the [68Ga]PSMA uptake was visually above background and not corresponding to sites of physiologic distribution. We used the syngo TrueD software via the Multimodality Workstation (Siemens Healthcare) for calculation of SUVmax. SUVmax was determined by manually placing a region of interest (ROI) using the Ellipsoid Isocontour tool over the primary tumor site as well as the most prominent lymph nodes and bone or soft tissue lesions. This was done on trans-axial images by an experienced nuclear medicine physician.
Physiological uptake areas were the lacrimal and salivary glands, liver, spleen, intestines as well as the urinary tract. A volume of about 30 cm3 of normal liver parenchyma, mostly from the inferior aspect of right liver lobe at a distance from any vascular structures, was used to calculate SUVmax of the liver, and this was taken as reference. SUVmax of any liver lesions was compared to normal liver parenchyma to confirm or exclude metastases.
All anomalous findings suggestive of PCa based on the clinical and imaging characteristics were considered pathologic unless another explanation for the increased uptake could be given, in which case the findings would be described as anomalous, but not pathologic [13]. CT-positive criteria for lymph nodes include an increase in the short axis diameter (more than 8 mm), an increase in contrast enhancement, or loss of fatty hilum. Bone metastases were identified by suspicious sclerotic or lytic lesions in bone window scale, and visceral metastases were detected by suspicious hypo- or hyperdense lesions in the specified organ.
Statistical Analysis
Patients’ characteristics and disease information were summarized by counts and percentages. Comparisons of findings and impressions out of [68Ga]PSMA PET/CT image and CT, MRI, and bone scan were performed using McNemar’s test. Kappa statistics were reported to show the concordance and discordance between results. Differences in iPSA and Gleason Score according to all images were done using Fisher’s exact test. A significance criterion of p ≤ 0.05 was used in the analysis. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
Twenty-one patients met the inclusion criteria and were included in the study (Table 1). The median age is 66.1 years (range, 54.3–80.6), 20 patients have high-risk disease (95 %), median PSA level is 38 ng/ml (range, 0.6–exceeding 100), histopathology was adenocarcinoma in all patients, with a Gleason score of 6 in one patient (5 %), seven in six patients (28 %), eight in five patients (24 %), and nine in nine patients (43 %). All patients underwent [68Ga]PSMA PET/CT scan (100 %) and at least one other imaging modality as follows: a total of 20 patients underwent CT scan (95 %), 15 patients underwent pelvic MRI scan (71 %), and 16 underwent bone scan (76 %). Twelve patients (57 %) received all four modalities as part of initial tumor staging.
Median SUVmax for the primary tumor was 11.3 (range, 2.5–65). This was evaluated in comparison to liver uptake, where the median SUVmax was 6.47 (range, 2.94–11). Eleven patients had associated PSMA-avid lymph nodes, median SUVmax for those was 17.4 (range, 3.7–49).
Per-Patient Analysis
Taking into account the patient’s overall stage after performing all necessary imaging, and taking into account the histopathological diagnosis, we analyzed the rate of concordance of each imaging modality with the final patient stage (Table 2). [68Ga]PSMA PET/CT revealed the highest congruence with a concordance rate of 90 %, significantly higher than the concordance rates of bone scan (75 %, p = 0.020), MRI (73 %, p = 0.021), and CT (60 %, p = 0.008).
Per-Lesion-Site Analysis
We compared [68Ga]PSMA PET/CT with MRI in the accuracy of detecting PG tumors and pelvic nodal spread. [68Ga]PSMA PET/CT showed a diagnostic accuracy and sensitivity close to that of MRI in detecting suspicious lesions within the PG (85.7 % vs. 86.7 %, p = 0.999) and a higher accuracy in detecting suspicious pelvic lymph nodes (95.2 % vs. 80 %, p = 0.001) as shown in Table 3. Sensitivity and specificity were both higher with [68Ga]PSMA PET/CT compared to MRI in detecting suspicious pelvic lymph nodes (92.3 % vs. 75 %, and 100 % vs. 85.7 %, respectively).
[68Ga]PSMA PET/CT also superseded CT scan in its diagnostic utility and overall accuracy in detecting suspicious pelvic lymph nodes (95.2 % vs. 75 %) as well as extra-pelvic lymph nodes (100 % vs. 75 %, p = 0.00001).
[68Ga]PSMA PET/CT proved to be even more sensitive than bone scan (100 % vs. 62.5 %) in detecting suspicious bone lesions, with better specificity (91.7 % vs. 87.5 %), NPV (100 vs. 70 %), and overall accuracy (95.2 % vs. 75 %, p = 0.0196).
Overall Change in Management
In line with all the information presented thus far, [68Ga]PSMA PET/CT changed the management in 11/21 patients (52 %). Seven patients were upstaged due to the following reasons: detection of bone lesions in a negative bone scan (n = 3), revealing pelvic lymph nodes (n = 1), and detecting pelvic with extra-pelvic lymph nodes (n = 3) that were otherwise undetectable by other modalities (example shown in Fig. 1). Treatment was thus shifted from local radiation or chemotherapy to systemic hormonal therapy in those patients.
[68Ga]PSMA PET/CT detects pelvic and extra-pelvic lymph nodes missed by MRI and CT scans: A 72-year-old patient with PSA 74 ng/ml, Gleason score 4+3, and a suspicious sternal lesion on bone scan with negative MRI and abdominopelvic CT scan. a MIP image of [68Ga]PSMA PET/CT showed abnormal increased PSMA uptake in the prostate cancer (red arrow) and multiple extra pelvic PSMA-avid lesions in the abdomen and chest (blue arrows). Axial CT scan (left) and [68Ga]PSMA PET/CT (right) at the level of b chest and c abdomen showed these PSMA avid subcentimetric lymph node metastases (blue arrows).
Four patients were down-staged due to the exclusion of the following: liver metastases (n = 1), bone metastases (n = 1), pelvic LNs (n = 1), and extra-pelvic LNs (n = 1). Treatment plan changed in line with their new stage and ranged between active surveillance, radical prostatectomy, and radiation therapy with hormonal treatment, depending on extent of disease.
Factors Affecting Concordance Between Imaging Modalities
We further stratified findings according to iPSA level and Gleason score to identify if such factors contributed to any discrepant findings among the imaging modalities. Comparing findings from patients with iPSA ≤ 20 ng/ml and those with iPSA > 20 ng/ml, we found no significant difference between the two groups in the overall accuracy of [68Ga]PSMA PET/CT (p = 0.098), bone scan, or MRI (p = 1), but there was a significant difference between the two groups in CT scan accuracy (p = 0.009), with a greater accuracy in patients with iPSA > 20 ng/ml. On a per-lesion-site basis, there was no significant difference between both groups in the detection of [68Ga]PSMA PET/CT for PG lesions (p = 0.245), pelvic lymph nodes (p = 0.294), extra-pelvic lymph nodes (p = 1), and bone lesions (p = 0.136). The same goes for MRI in the detection of PG lesions (p = 0.385) and pelvic lymph nodes (p = 0.495), as well as CT in the detection of extra-pelvic lymph nodes (p = 0.312).
As for the Gleason score, we grouped patients with scores of six and seven together in one group and those with scores of eight and nine in another group. Among the two groups, there was no significant difference in the overall accuracy of [68Ga]PSMA PET/CT (p = 0.533), bone scan (p = 0.642), MRI (p = 1), or CT scan (p = 0.397). On a per-lesion-site basis, there was no significant difference between both groups in the detection of [68Ga]PSMA PET/CT for PG lesions (p = 0.521), pelvic and extra-pelvic lymph nodes (p = 1) as well as bone lesions (p = 0.583). The same goes for MRI in the detection of PG lesions (p = 0.486) and pelvic lymph nodes (p = 1), as well as CT in the detection of extra-pelvic lymph nodes (p = 0.278).
Discussion
Accurate primary staging of patients with high-risk PCa is very crucial, given the high propensity for metastases and the overall high burden of disease. Among conventional imaging, MRI has shown its reliability in primary staging of PCa and is indispensable in current practice guidelines. Despite this, many deficiencies still exist in conventional morphologic imaging.
Over the past few years, PSMA has been gaining momentum in both, diagnosis as well as treatment of PCa, given that PCa cells express PSMA on their surface membrane [9, 14, 15]. PSMA is a type II transmembrane protein and an ideal target for molecular imaging of PCa owing to its biological characteristics. Such characteristics include considerable (100-fold to 1000-fold) overexpression on the cell membrane of nearly all PCa cells compared with normal non-target cells, and increased expression in advanced-stage and castration-resistant PCa [9]. Furthermore, internalization and endosomal recycling of PSMA after binding to its ligand results in increased deposition of conjugated [68Ga]PSMA into the cell with subsequent improvement of imaging.
[68Ga]PSMA PET/CT is thus a novel imaging modality that has been gaining more approval in the diagnosis of primary and relapsed PCa, with very encouraging preliminary results on its use in primary staging of patients with PCa [10, 11]. [68Ga]PSMA PET/CT has also been reported to improve radiotherapy management in patients with PCa with potential for more individualized therapy planning [16, 17]. In our study, we evaluate the potential of [68Ga]PSMA PET/CT for primary staging of patients with PCa in comparison to conventional imaging modalities, namely MRI, CT, and bone scans.
Our study is a retrospective cohort study that includes a homogenous cohort of patients with PCa undergoing initial staging with conventional imaging modalities along with [68Ga]PSMA PET/CT. While many papers have been published on the role of [68Ga]PSMA PET/CT in the diagnosis of early biochemically-relapsed PCa, only a handful of studies targeted its use in primary staging prior to any therapy [18]. Our findings are thus of relevance in clinical practice. In addition, this is the first study of its kind conducted in Jordan as well as the Middle East, and is one of the few studies investigating the impact of this imaging modality on clinical management.
MRI is the standard imaging modality used to detect cancer in the PG, to define the T-status of the tumor, and to detect spread in pelvic lymph nodes, while CT is reserved for pelvic and extra-pelvic nodal spread, and the bone scan is usually used for the detection of bone metastases given its high sensitivity. [68Ga]PSMA PET/CT was compared with each of these modalities in their specific detection sites (Table 3). As we have shown in this study, [68Ga]PSMA PET/CT almost outperformed all three imaging modalities used as standard of care, both on a per-patient basis and a per-lesion-site basis. The only exception was MRI with a slightly better sensitivity and accuracy in the detection of primary tumor in the PG. We did not investigate in this population the role of [68Ga]PSMA PET/CT in defining the T-status of the tumor, as this is mainly provided with MRI which has excellent soft tissue contrast resolution for this particular purpose. [68Ga]PSMA PET/CT may be used as an adjunct modality in guiding tumor biopsy, but this needs to be further investigated in well-designed clinical trials specific for this purpose.
By comparing these imaging modalities together, taking into account that 57 % (n = 11) of patients had undergone all four scans, we firstly analyzed the concordance of each modality with the final overall stage agreed upon at the MDC meetings as well as upon follow-up imaging and lab findings. Any discordance (whether false upstaging or false downstaging) was noted. [68Ga]PSMA PET/CT significantly superseded all other modalities with an accuracy of 90 % (Table 2).
There were only two cases where [68Ga]PSMA PET/CT findings were discordant with overall staging. In one patient, [68Ga]PSMA PET/CT had missed pelvic lymph nodes that were otherwise detected by MRI as prominent (with size of 8 mm) and staged as T3N1. The MDC decision was to proceed with radical prostatectomy and pelvic lymph node dissection (PLND), and that provided histopathological confirmation of pelvic lymph node metastasis. In this particular case, [68Ga]PSMA PET/CT may have been susceptible to the micrometastatic size of tumor deposits. This is in line with the findings of Budäus, et al. [19] who reported intranodal tumor deposit detection at a median size of 13.6 mm (vs. 4.3 mm for undetected lymph node metastases). Van Leeuwen et al. [20] observed intense radiotracer uptake in 60 % of lymph node metastases measuring 2 to 4.9 mm based on histopathology. They conclude that almost all false negative lymph node metastases were less than 5 mm in diameter (median 2.7 mm). In our case, however, the lymph nodes were slightly larger (8 mm), which is explainable by the appearance of the halo in PET/ CT. This halo artifact is mostly attributable to the high contrast between the radioactivity signal within the urinary bladder and the low signal of the surrounding background.
In the other case, [68Ga]PSMA PET/CT falsely up-staged the patient by detecting suspicious bone metastasis in the ribs. Bone scan was not performed in this patient. The MDC decision was to go for radical prostatectomy with PLND and follow-up on the suspicious bone lesions. Subsequent PSA levels were undetectable. A recent report [21] shows a similar occurrence in two elderly male patients recently diagnosed with high-risk PCa, in whom there was an increased [68Ga]PSMA uptake in rib fractures, characteristically placed as “pearls on a string”. Other studies report that benign bone disease like fibrous dysplasia [22] and Paget’s disease [23, 24] can occasionally exhibit increased radiotracer uptake. Such findings must be taken into account when reporting [68Ga]PSMA PET/CT findings.
Another round of analysis stratified the findings into five main sites as previously outlined, and each modality was assessed with regard to its detection accuracy at these sites. Even though individual lesion confirmation by histopathology was not possible given the ethical and practical limitations, the delineation of each lesion-site as true or false positive/negative was made based on follow-up imaging if performed, any subsequent histopathological confirmation (in the case of PLND or biopsies) and follow-up PSA levels to rule out any metastasis when such serum levels become undetectable. Other than the previous two discordant cases, [68Ga]PSMA PET/CT had missed lung metastasis in one patient which were detected by CT scan and later confirmed histopathologically following lung biopsy. With regard to detecting PCa in its primary location, [68Ga]PSMA PET/CT was non-specific in three cases (SUVmax values were 2.5, 3.28, and 3.5), and these were deemed as false-negative in the per-lesion-site analysis.
Bone scan and [68Ga]PSMA PET/CT were congruent in 10 of 14 cases (71 %) in detecting or ruling out bone lesions. In three of the remaining four cases, bone scan falsely missed bone lesions that were PSMA-avid on [68Ga]PSMA PET/CT and were thus considered bone metastases (an example is shown in Fig. 2). In the fourth case, bone scan showed irregularly-increased radiotracer uptake in the lumbar spine and metastasis could not be ruled out, while [68Ga]PSMA PET/CT was negative in this patient.
[68Ga]PSMA PET/CT rules out mediastinal lymph nodes and detects bone metastases missed by bone scan: A 64-year-old patient with PSA 14 ng/ml, Gleason score 4+5, and a CT scan with prominent mediastinal lymph nodes. a MIP image of [68Ga]PSMA PET/CT did not show abnormal PSMA uptake in the mediastinum, but there was a concerning focus in the right chest wall (red arrow). b Transaxial CT (top), PET (middle), and PET/CT (bottom) for the same patient—there was a prominent right upper para-tracheal lymph node on CT scan (red arrow) but without abnormal PSMA uptake on PET and fused images. c PET and PET/CT at the level of the chest demonstrated PSMA-avid lesion in the coracoid process of the right scapula (blue arrows) with corresponding subtle sclerosis on CT images (red arrow), suggesting bone metastases. Another two rib lesions were also suspected (not shown). d Bone scan was negative for suspicious bone metastases.
Only two patients had lung or liver metastasis. One of these patients had liver lesions confirmed by both CT and [68Ga]PSMA PET/CT scans, and this same patient had false-positive lesions identified in the lungs by CT but confirmed as negative by [68Ga]PSMA PET/CT, with later PSA values reaching undetectable levels. The other patient had a CT scan that correctly identified the presence of lung metastases, with a false-negative [68Ga]PSMA PET/CT as previously discussed. Two other patients had false-positive lesions detected by CT scan (once in the liver and another in the lungs), [68Ga]PSMA PET/CT did not show any uptake and later PSA levels post-treatment went undetectable, hence supporting the [68Ga]PSMA PET/CT findings.
It is worth noting that in nine patients, 3-h delayed images were acquired as previously mentioned. An improvement in the target-to-background ratio was noticed over time; however, proper staging and stratification of our patients could already be performed based on the findings of standard imaging (1 h post-injection). In two patients in particular, tinier PSMA-avid lymph nodes were detected in the 3-h delayed images, but these lesions had no impact on the staging status of these patients.
New PSMA ligands have been recently introduced and studied, such as F-18-labeled PET tracers, with the capacity of improving the PSMA imaging landscape. [18F]PSMA-1007 has been shown to have comparable performance with [68Ga]PSMA-11, but its longer half-life, superior energy characteristics, and non-urinary excretion overcome some of the limitations of Ga-68-labeled PSMA-targeted tracers [25]. This allows for a more improved imaging of the prostate region, potentially improving primary staging and the detection of local recurrence. In addition, combination of PET with MRI is quite an intriguing approach, not only for primary staging and detection of local recurrence in PCa, but also for employing the principle of radiomics. The same holds true for the introduction of digital PET allowing for an improved resolution and even dynamic imaging. However, the amount of existing clinical data is sparse and it remains to be shown that this potential superiority indeed impacts patient management.
Our study is limited by virtue of its retrospective nature as well as the small number of patients examined in this study. In many cases, a comparison of imaging modalities with a significant difference could not be warranted given the limited sample size, and this highlights the need for prospective studies with adequate numbers of patients to achieve statistical significance. The majority of patients with PCa seen in our center present with relapse, and we have only started performing [68Ga]PSMA PET/CT for initial staging and restaging of patients with PCa as early as 2015. It is also worth noting that the MRI scans performed are pelvic MRI, with occasional lumbosacral MRI scans done in specific patients. Hence bone metastasis were not evaluated via MRI scans given that not all patients were offered this option. Finally, and as previously mentioned, pathologic confirmation for bone and lymph node metastasis in relevant cases was not always possible (only two patients underwent PLND as was previously described), and a reference standard was not used for an endpoint decision. Instead, evaluation of all clinical and radiological findings at our MDC conferences was used as the main reference point.
Conclusions
In conclusion, [68Ga]PSMA PET/CT seems to be an invaluable imaging modality in the assessment of primary high-risk PCa with great potential for the detection of lymph node spread and bone metastases that would impact the management plan. Further prospective studies with larger cohorts are recommended in order to fully include [68Ga]PSMA PET/CT in clinical practice guidelines for the assessment of patients with primary PCa.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, Mason M, Matveev V, Wiegel T, Zattoni F, Mottet N, European Association of Urology (2014) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent—update 2013. Eur Urol 65:124–137
Fitzmaurice C, Dicker D, Pain A et al (2015) The global burden of cancer 2013. JAMA Oncol 1:505–527
European Association of Urology. Guidelines on prostate cancer. http://uroweb.org/guideline/prostatecancer/
Maurer T, Eiber M, Schwaiger M, Gschwend JE (2016) Current use of PSMA-PET in prostate cancer management. Nat Rev Urol 13:226–235
Afshar-Oromieh A, Avtzi E, Giesel FL, Holland-Letz T, Linhart HG, Eder M, Eisenhut M, Boxler S, Hadaschik BA, Kratochwil C, Weichert W, Kopka K, Debus J, Haberkorn U (2015) The diagnostic value of PET/CT imaging with the 68Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging 42:197–209
Eiber M, Maurer T, Souvatzoglou M, Beer AJ, Ruffani A, Haller B, Graner FP, Kubler H, Haberhorn U, Eisenhut M, Wester HJ, Gschwend JE, Schwaiger M (2015) Evaluation of hybrid 68Ga-PSMA ligand PET/CT in 248 patients with biochemical recurrence after radical prostatectomy. J Nucl Med 56:668–674
Ceci F, Uprimny C, Nilica B, Geraldo L, Kendler D, Kroiss A, Bektic J, Horninger W, Lukas P, Decristoforo C, Castellucci P, Fanti S, Virgolini IJ (2015) 68Ga-PSMA PET/CT for restaging recurrent prostate cancer: which factors are associated with PET/CT detection rate? Eur J Nucl Med Mol Imaging 42:1284–1294
Eder M, Schäfer M, Bauder-Wüst U, Hull WE, Wängler C, Mier W, Haberkorn U, Eisenhut M (2012) 68Ga-complex lipophilicity and the targeting property of a urea-based PSMA inhibitor for PET imaging. Bioconjug Chem 23:688–697
von Eyben FE, Picchio M, von Eyben R, Rhee H, Bauman G (2016) 68Ga-labeled prostate-specific membrane antigen ligand positron emission tomography/computed tomography for prostate cancer: a systematic review and meta-analysis. Eur Urol Focus. https://doi.org/10.1016/j.euf.2016.11.002
Corfield J, Perera M, Bolton D, Lawrentschuk N (2018) 68Ga-prostate specific membrane antigen (PSMA) positron emission tomography (PET) for primary staging of high-risk prostate cancer: a systematic review. World J Urol 36:519–527
D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, Tomaszewski JE, Renshaw AA, Kaplan I, Beard CJ, Wein A (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280:969–974
Fanti S, Minozzi S, Morigi JJ, Giesel F, Ceci F, Uprimny C, Hofman MS, Eiber M, Schwarzenbock S, Castellucci P, Bellisario C, Chauvie S, Bergesio F, Emmett L, Haberkorn U, Virgolini I, Schwaiger M, Hicks RJ, Krause BJ, Chiti A (2017) Development of standardized image interpretation for 68Ga-PSMA PET/CT to detect prostate cancer recurrent lesions. Eur J Nucl Med Mol Imaging 44:1622–1635
Wright GL Jr, Grob BM, Haley C et al (1996) Upregulation of prostate-specific membrane antigen after androgen deprivation therapy. Urol 48:326–334
Silver DA, Pelicer I, Fair WR et al (1997) Prostate specific membrane antigen expression in normal and malignant human tissues. Clin Cancer Res 3:81–85
Dewes S, Schiller K, Sauter K, Eiber M, Maurer T, Schwaiger M, Gschwend JE, Combs SE, Habl G (2016) Integration of 68Ga-PSMA-PET imaging in planning of primary definitive radiotherapy in prostate cancer: a retrospective study. Radiat Oncol 11:73. https://doi.org/10.1186/s13014-016-0646-2
Sterzing F, Kratochwil C, Fiedler H, Katayama S, Habl G, Kopka K, Afshar-Oromieh A, Debus J, Haberkorn U, Giesel FL (2016) 68Ga-PSMA-11 PET/CT: a new technique with high potential for the radiotherapeutic management of prostate cancer patients. Eur J Nucl Med Mol Imaging 43:34–41
Virgolini I, Decristoforo C, Haug A et al (2017) Current status of theranostics in prostate cancer. Eur J Nucl Med Mol Imaging 45:471–495
Budäus L, Leyh-Bannurah SR, Salomon G, Michl U, Heinzer H, Huland H, Graefen M, Steuber T, Rosenbaum C (2016) Initial experience of 68Ga-PSMA PET/CT imaging in high-risk prostate cancer patients prior to radical prostatectomy. Eur Urol 69:393–396
van Leeuwen PJ, Emmett L, Ho B, Delprado W, Ting F, Nguyen Q, Stricker PD (2017) Prospective evaluation of 68gallium-prostate-specific membrane antigen positron emission tomography/computed tomography for preoperative lymph node staging in prostate cancer. BJU Int 119:209–215
Jochumsen MR, Dias AH, Bouchelouche K (2018) Benign traumatic rib fracture: a potential pitfall on 68Ga-prostate-specific membrane antigen PET/CT for prostate cancer. Clin Nucl Med 43:38–40
De Coster L, Sciot R, Everaerts W et al (2017) Fibrous dysplasia mimicking bone metastasis on 68GA-PSMA PET/MRI. Eur J Nucl Med Mol Imaging 44:1607–1608
Artigas C, Alexiou J, Garcia C, Wimana Z, Otte FX, Gil T, van Velthoven R, Flamen P (2016) Paget bone disease demonstrated on 68Ga-PSMA ligand PET/ CT. Eur J Nucl Med Mol Imaging 43:195–196
Bourgeois S, Gykiere P, Goethals L, Everaert H, de Geeter FW (2016) Aspecific uptake of 68GA-PSMA in Paget disease of the bone. Clin Nucl Med 41:877–878
Giesel FL, Hadaschik B, Cardinale J, Radtke J, Vinsensia M, Lehnert W, Kesch C, Tolstov Y, Singer S, Grabe N, Duensing S, Schäfer M, Neels OC, Mier W, Haberkorn U, Kopka K, Kratochwil C (2017) F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. Eur J Nucl Med Mol Imaging 44:678–688
Acknowledgments
Authors would like to acknowledge and thank the Office of Scientific and Academic Research (OSAR) at KHCC, particularly Mrs. Dalia Al-Rimawi for her work on the statistical analyses of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Hirmas, N., Al-Ibraheem, A., Herrmann, K. et al. [68Ga]PSMA PET/CT Improves Initial Staging and Management Plan of Patients with High-Risk Prostate Cancer. Mol Imaging Biol 21, 574–581 (2019). https://doi.org/10.1007/s11307-018-1278-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-018-1278-8