Abstract
Objective
To verify whether the combination of transcutaneous electrical neural stimulation (TENS) with oxybutynin in the treatment of women with overactive bladder (OAB) would be more effective than isolated treatments.
Methods
We randomized 75 women with OAB, in three groups: GI—30 min TENS, twice a week; GII—daily slow release 10 mg oxybutynin; and GIII—TENS + oxybutynin (multimodal); all for 12 weeks. Patients were evaluated with validated questionnaires International Consultation on Incontinence-Short Form (ICIQ-SF), International Consultation on Incontinence-OAB (ICIQ-OAB), Symptom bother, and 3-day Voiding diary at weeks 0, 12, and 24.
Results
The groups were similar before treatment. After treatment, all groups significantly improved in OAB symptoms and quality of life (QoL). At week 12, ICIQ-OAB scores were 5.9, 4.6, and 2.9, in groups I, II, and III, respectively, p = 0.01. At week 24, GI and GIII kept the scores of the end of treatment (week 12), while GII increased ICIQ-OAB from 4.6 to 9.2, p = 0.0001, ICIQ-SF from 9.8 to 13.3, p = 0.0006, and Symptom bother score from 3.4 to 7.0, p = 0.0001.
Conclusions
The multimodal treatment was more effective and TENS alone or in association presented longer lasting results for improvement of clinical symptoms of OAB and QoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the International Continence Society (ICS), the clinical diagnosis of overactive bladder (OAB) is based on symptoms of urinary urgency, with or without urgency incontinence, accompanied by increased urinary frequency and nocturia in the absence of pathological or metabolic factors that would explain these symptoms [1].
The goal of treatment is to decrease the daytime and nighttime urinary frequency, increase voided volume, and decrease episodes of urgency and urgency incontinence, by relaxing the bladder muscle, resulting in improved quality of life (QoL) [2]. Transcutaneous electrical neural stimulation (TENS) is a safe and effective alternative for the treatment of OAB, and its efficacy is well documented in the literature [3].
Studies have demonstrated the potential efficacy of combination of treatments [4], which led to the aim of this study, verifying in a prospective randomized study whether the combination of posterior tibial TENS with oxybutynin in the treatment of women with OAB would be more effective than isolated treatments.
Methods
The study was conducted between August 2008 and May 2010. The project was approved by the local Ethics Committee in Research, Protocol #625/2007 and informed consent was obtained by all participants.
Women included in the study presented with clinical complaints of OAB: urinary frequency, nocturia, and/or urgency incontinence with negative urinalysis and urine culture. We excluded patients who had previous treatment, residual urine, cognitive and psychiatric deficits, pregnancy, glaucoma, stress urinary incontinence, any pelvic organ prolapse quantification system (POP-Q) ≥ grade II, neurogenic OAB, those using anticholinergic drugs, calcium antagonists, β-antagonists, and dopamine antagonists.
In the initial evaluation of the study (week 0), a complete evaluation included age, race, comorbidities, medications, urinary disorders, and validated questionnaires: “International Consultation on Incontinence-Short Form” (ICIQ-SF) to assess incontinence and the “International Consultation on Incontinence-OAB” (ICIQ-OAB) to evaluate the symptoms of OAB (urinary frequency, nocturia, urinary urgency, and urinary incontinence). An analog scale from 0 to 10 quantified the impact of each symptom in the patients’ QoL (Symptom bother). Then, the patients completed a Voiding diary for 3 days, which objectively informed the daytime and nighttime urinary frequency, urgency, nocturia, and urinary incontinence episodes.
After initial assessment, the patients were divided randomly into three groups using online randomization (http://www.graphpad.com/quickcalcs/randomize1/) and each group received the following treatment:
TENS group
Electrical stimulation of posterior tibial nerve using a device manufactured by Neurodyn Portable®, being one surface electrode placed behind the medial malleolus (negative) and another placed 10 cm above the first one (Supplementary fig. 1). The regulation was established at 10 Hz frequency, pulse width of 250 μs. The intensity was adjusted to the highest level possible, but never able to cause pain to the patient. The treatment lasted 12 weeks, performed twice a week, each session was 30 min long.
Oxybutynin group
Slow release oxybutynin 10 mg, once daily for 12 weeks. The choice of medication was due to the easier purchase and lower cost representing the most accessible anticholinergic medicine.
Multimodal group
Association of TENS and oxybutynin (multimodal treatment), the same offered to TENS and Oxybutynin Groups, for 12 weeks.
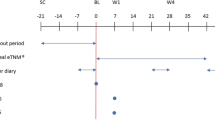
All patients were reevaluated twice with the same tools used in the initial assessment: ICIQ-SF, ICIQ-OAB, Symptom bother, and Voiding diary at the end of 12 weeks of treatment (week 12) and after 12 weeks of treatment cessation (week 24) at 6 months of study follow-up.
The primary end points were ICIQ-SF, ICIQ-OAB, and Symptom bother scores. Exploratory end points included Voiding diary variables.
For statistical evaluation, we used the Fisher exact test to compare proportions and the Kruskal–Wallis test to compare continuous or rankable measures among the three groups. To compare proportions among groups over time, the method of generalized estimation equation (GEE) was used. The ANOVA was used for repeated measures and Tukey’s test for multiple comparisons. The two-sided level of statistical significance considered was p < 0.05. The software used was SAS System for Windows (Statistical Analysis System), version 9.2. SAS Institute Inc., 2002–2008, Cary, NC, USA.
Results
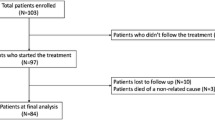
Based on a priori power calculation, a total of 75 women with clinical symptoms of OAB were randomized into 3 groups (25 in each). Patients who failed to comply with the 12 weeks of treatment (Week 12) and/or did not attend the reassessment after treatment (Week 24) at 6 months follow-up were excluded from analysis.
At the end of the study, data from 58 patients were analyzed, 18 in TENS Group, 19 in Oxybutynin Group, and 21 in Multimodal Group (Supplementary fig. 2). Even after dropout, 80 % sample power was kept (post hoc analysis).
Regarding demographics, patients’ mean and range ages were 56.9 (33–77), 57.7 (34–79), and 60.1 (33–77), in the TENS, Oxybutynin, and Multimodal Groups, respectively, p = 0.76. Analyzing the percentage of patients with urinary incontinence and nocturia before treatment, we found no significant difference among groups, p = 0.46 and p = 0.50, respectively. Also, at baseline, there were no significant differences among groups in terms of ICIQ-SF, ICIQ-OAB, and Symptom bother (Table 1).
ICIQ-SF
During initial assessment (week 0), the ICIQ-SF average score was 16.3 in TENS Group, 17.1 in Oxybutynin Group, and 16.9 in Multimodal Group, p = 0.88.
In the evaluation at 12 weeks of treatment (week 12), all groups had a reduction in episodes of incontinence, represented by the ICIQ-SF decreased score (7.2 in TENS Group, 9.8 in Oxybutynin Group, and 7.9 in Multimodal Group), with no significant difference among groups, p = 0.31.
At 6 months follow-up, 12 weeks after treatment discontinuation (week 24), patients in Oxybutynin Group showed a significant increase in incontinence episodes, represented by the ICIQ-SF increase (from 9.8 to 13.3) compared to TENS Group and Multimodal Group that maintained improvement observed after treatment (p = 0.0006), Fig. 1 and Table 1.
ICIQ-OAB
During the initial evaluation (week 0), the ICIQ-OAB average score was 10.3 in TENS Group, 11.8 in Oxybutynin Group, and 11.0 in Multimodal Group, p = 0.15. Analyzing the scores at 12 weeks of treatment (week 12), multimodal treatment had a higher improvement in symptoms of OAB (2.9) compared to patients treated with monotherapy, TENS (5.9) and oxybutynin (4.6), p = 0.01.
Also, patients that underwent TENS as single or multimodal therapy kept the scores at the end of study at 6 months follow-up (week 24) without any significant difference, whereas Oxybutynin Group had a significant increase in the ICIQ-OAB score from 4.6 to 9.2, p < 0.0001; demonstrating that these patients experienced OAB symptoms again after stopping treatment with oxybutynin (Fig. 1 and Table 1).
Symptom bother
The mean Symptom bother score of patients in TENS Group went from 8.3 during the initial evaluation (week 0) to 3.9 at 12 weeks of treatment (week 12), (p = 0.0002), the Oxybutynin Group went from 8.4 to 3.4 (p < 0.0001), and Multimodal Group from 8.3 to 1.7 (p < 0.0001), with no difference among groups at weeks 0 and 12, p = 0.92 and p = 0.06, respectively; nevertheless, multimodal treatment trended toward better mean Symptom bother score at week 12.
When assessed at 6 months follow-up (week 24), 3 months after the end of interventions, there was a statistically significant difference among the three groups regarding Symptom bother, p < 0.0001, the scores being 4.2, 7.0, and 1.6 in TENS, Oxybutynin, and Multimodal Groups, respectively (Fig. 1 and Table 1), illustrating the same phenomenon of “effect loss” in the Oxybutynin Group demonstrated for ICIQ-SF and ICIQ-OAB. Interestingly, Multimodal Group patients reported better QoL than TENS Group patients, especially regarding nocturia, p = 0.02.
Voiding diary
The baseline (week 0) and post-treatment (week 12) urinary frequency decreased from 12.7 to 8 in TENS Group, 11 to 7.9 in Oxybutynin Group, and 11.2 to 7.6 in Multimodal Group, with no difference among groups, p = 0.75.
The proportions of patients presenting with urinary incontinence at baseline (week 0) and after treatment (week 12) significantly decreased in all groups, p < 0.0001, with no difference among groups, p = 0.33; 94 and 11 % in TENS Group, 100 and 31 % in Oxybutynin Group, and 95 and 19 % in Multimodal Group, respectively.
The percentages of patients presenting with nocturia significantly decreased in all groups at week 12, p < 0.0001, from 94 to 11 % in TENS Group, 84 to 5 % in Oxybutynin Group, and 95 to 14 % in Multimodal Group, with no difference among groups, p = 0.24.
At week 24, urinary frequency, urinary incontinence, and nocturia patient proportions were not different among groups, p = 0.51, being 7.9, 14%, and 13 % in TENS Group, 9.2, 34 %, and 15 % in Oxybutynin Group, and 7.8, 18 %, and 14 % in Multimodal Group, respectively.
Discussion
The present study showed a significant decrease in the studied scores and in the number of episodes of urgency incontinence, nocturia, and urinary frequency after all treatments. In accordance with the literature [5], there was no significant difference between patients treated with electrical stimulation of the posterior tibial nerve or oxybutynin; after treatment, all groups reported improvement in symptoms and QoL, but when treatment was interrupted, patients treated with oxybutynin only presented with recurrence of OAB symptoms and their QoL decreased.
A meta-analysis by Burton et al. [5] showed improvement or cure of OAB symptoms ranging from 37 to 82 % of patients treated with TENS. When compared to antimuscarinic treatment, no significant difference was found. Rai et al. [6] in another meta-analysis pointed that more evidence comparing individual types of electrostimulation to the most effective types of anticholinergics is required and that it is unlikely that the effects of anticholinergics persist after stopping treatment, also in agreement with the current study.
When compared to patients who underwent the multimodal treatment (oxybutynin + TENS), significant difference was found in improving symptoms of OAB, mainly regarding the urgency and nocturia. Patients in multimodal treatment had reported better QoL and had improved more regarding urgency and nocturia when compared to those who received isolated treatments.
Furthermore, most patients do not improve from continence with a single therapy and the long-term medication compliance may be difficult due to side effects, expense, tolerability, and convenience issues [7].
Overactive bladder is a chronic condition and requires lifelong treatment to control symptoms. The effectiveness of antimuscarinic agents is well documented in the literature, but after 12 months of treatment only 32 % of patients follow on use of medication, mainly due to side effects [8].
On the other hand, Govier et al. found no significant adverse effects with electrical stimulation of the posterior tibial nerve in a prospective multicenter study including 53 patients, reporting successful treatment in 71 % (25 % reduction in the number of daytime urination, 21 % in nocturia, 35 % improvement in incontinence, 30 % improvement in pain, and 20 % improvement in quality of life) [9].
Peters et al. have hypothesized that fewer side effects or even biases related to the novelty of treatment might account for the better results of TENS (12 weekly sessions for 30 min) compared to tolterodine (for 90 days, 4 mg/day; in case of adverse effects, the dose was decreased to 2 mg/day), with improvement or cure in 79.5 % compared to 54.8 %, respectively (p < 0.01). With regard to improvement of OAB symptoms compared to baseline, these were significantly higher in TENS group (79.5 % cure or improvement) compared to the tolterodine group (54.8 %) [10].
Adding TENS to drug treatment is an attractive approach to improve the results and possibly allow the interruption of pharmaceutical therapy, limiting side effects and positively impacting QoL. Also, anticholinergic drugs can work synergistically with TENS intervention due to different mechanisms of action and TENS seems to be an effective and safe treatment for refractory OAB [11]. Due to the use of different courses of action, the association of different treatments is expected to lead to better results in the improvement of OAB symptoms.
Pharmacological treatment with oxybutynin blocks muscarinic receptors that are responsible for vesical contractions. TENS inhibits involuntarily the detrusor by central reflex, reorganizes synapses activating the sympathetic inhibitory neurons (hypogastric nerve), and inhibits parasympathetic excitatory neurons (pelvic nerve) [2].
There are various types of treatment for OAB available in literature, with different mechanisms of action, allowing the combination of these to improve the QoL of patients. The choice of therapy will be based on several factors, including co-morbidities, mental status, age, education, motivation, and mobility, but it is always important to tailor the optimal treatment for each individual, knowing that this is a chronic disease and that therapy must be adapted over the life of each patient.
Mattiasson et al. [4] showed that the combination of tolterodine (anticholinergics) with bladder training significantly reduced the urinary frequency and increased the voided volume compared with the use of tolterodine alone. About 76 % of patients who have used combined treatment reported an improvement in their urinary symptoms compared to baseline and compared to 71 % in the tolterodine monotherapy. This finding is consistent with previous studies showing that the association of non-drug active therapies significantly increases the effectiveness of anticholinergics, reducing the voiding frequency and increasing voided volume [12].
Additionally, though in agreement with our results, symptom improvement after 12 weekly tibial nerve stimulation demonstrates durability through 12 months [13], it is not precise how long after the interruption of the treatment patients who were treated with TENS or association of TENS and medication will present clinical symptoms of OAB, as this is a chronic condition. Studies have not demonstrated whether a longer treatment, with a few more sessions of electrical stimulation, would help to maintain the improvement in symptoms and long-term follow-up of patients is needed to clarify these questions.
Levin et al. [14] in a systematic review emphasized the limited high quality data on TENS for OAB specifically in women, to which the present study meaningfully adds. Further studies are needed in order to assess whether multimodal treatment would make possible to decrease the dosage of antimuscarinics, diminishing side effects and improving QoL of patients, as well as decreasing treatment interruptions.
Finally, while the small number of patients, the lack of a cross-over design with placebo and sham TENS groups, the restriction to the slow release oxybutynin 10 mg representing anticholinergics and a relatively short-term follow-up are limitations of the current study, important strengths are not pooling of results for male and female subjects, the comprehensive evaluation with differentiation of specific symptoms of OAB utilizing validated questionnaires, the use of control arms and additional evaluation after treatment cessation.
Conclusions
Multimodal treatment was more effective for improvement of clinical symptoms of OAB and improvement of QoL than TENS and oxybutynin alone. Also, TENS treatment (alone or in association) presented longer lasting results than oxybutynin monotherapy.
References
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
Abrams P, Cardozo L, Wein A (2012) 3rd international consultation on incontinence–research society 2011. Neurourol Urodyn 31:291–292
Bellette PO, Rodrigues Palma PC, Hermann V et al (2009) Posterior tibial nerve stimulation in the management of overactive bladder: a prospective and controlled study. Actas Urol Esp 33:58–63
Mattiasson A, Blaakaer J, Hoye K et al (2003) Simplified bladder training augments the effectiveness of tolterodine in patients with an overactive bladder. BJU Int 91:154–160
Burton C, Sajja A, Latthe PM (2012) Effectiveness of percutaneous posterior tibial nerve stimulation for overactive bladder: a systematic review and meta-analysis. Neurourol Urodyn 31:1206–1216
Rai BP, Cody JD, Alhasso A et al (2012) Anticholinergic drugs versus non-drug active therapies for non-neurogenic overactive bladder syndrome in adults. Cochrane Database Syst Rev 12:CD003193
Pelletier EM, Vats V, Clemens Q (2009) Pharmacotherapy adherence and costs versus nonpharmacologic management in overactive bladder. Am J Manag Care 15:S108–S114
Anderson KE (2004) Antimuscarinics for treatment of overactive bladder. Lancet Neurol 3:46–53
Govier FE, Litwiller S, Nitti V et al (2001) Percutaneous afferent neuromodulation for the refractory overactive bladder: results of a multicenter study. J Urol 165:1193–1198
Peters KM, MacDiarmid SA, Wooldridge LS et al (2009) Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: results from the overactive bladder innovative therapy trial. J Urol 182:1055–1061
Tellenbach M, Schneider M, Mordasini L et al (2012) Transcutaneous electrical nerve stimulation: an effective treatment for refractory non-neurogenic overactive bladder syndrome? World J Urol. doi:10.1007/s00345-012-0888-z
Goode PS, Burgio KL, Locher JL et al (2002) Urodynamic changes associated with behavioral and drug treatment of urge incontinence in older women. J Am Geriatr Soc 50:808–816
MacDiarmid SA, Peters KM, Shobeiri SA et al (2010) Long-term durability of percutaneous tibial nerve stimulation for the treatment of overactive bladder. J Urol 183:234–240
Levin PJ, Wu JM, Kawasaki A et al (2012) The efficacy of posterior tibial nerve stimulation for the treatment of overactive bladder in women: a systematic review. Int Urogynecol J 23:1591–1597
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Souto, S.C., Reis, L.O., Palma, T. et al. Prospective and randomized comparison of electrical stimulation of the posterior tibial nerve versus oxybutynin versus their combination for treatment of women with overactive bladder syndrome. World J Urol 32, 179–184 (2014). https://doi.org/10.1007/s00345-013-1112-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-013-1112-5