Abstract
Purpose
To evaluate long-term use, efficacy and tolerability of transcutaneous tibial nerve stimulation (TTNS) in the treatment of refractory overactive bladder (OAB).
Methods
We performed a prospective observational study and included all patients treated in a single center for OAB persisting after first-line anticholinergic treatment, with ≥ 24 months follow-up. The protocol consisted of daily stimulation at home. The primary outcome was treatment persistence. Amelioration was defined as an improvement in urinary symptom profile (USP) score.
Results
We assessed 84 consecutive patients. After a mean follow-up of 39.3 months and a mean treatment use of 8.3 months, almost two-thirds of patients (71.8%) had discontinued TTNS. Treatment continuation was > 12 months for 28 patients (33.3%) and > 18 months for 16 patients (19%). TTNS was successful following 3 months of treatment in 60 (71%) patients. Mean USP score stayed significantly lower than baseline until 12 months of treatment, but was not significant anymore after 18 months. Discontinuation therapy reasons were a lack of sufficient symptom relief for 59 (70%) patients, compliance difficulty for 5 (6%) patients and becoming asymptomatic for 6 (8%) patients. No serious adverse events occurred.
Conclusions
The present study confirms the utility of TTNS as a treatment option for patients with resistant OAB. In the long-term use, few patients continued with therapy, mostly because of a decreased effectiveness with time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the International Continence Society terminology, overactive bladder (OAB) is defined by urinary urgency, with or without urgency urinary incontinence, and often associated with urinary frequency and nocturia, in the absence of any pathological or metabolic conditions that may cause or mimic OAB [1]. Nearly 12% of the European population is concerned [2]. This chronic condition requires lifelong therapy to restore the quality of life while balancing efficacy and side effects. The mainstay of treatment is pharmacotherapy with antimuscarinic agents [3]; however, patient adherence rates decrease during 12 months of therapy for many reasons (intolerable side effects or lack of sufficient symptom relief) [4]. In the case of failure or poor tolerance, surgical treatments such as sacral neuromodulation or intradetrusor injections of botulinum toxin are indicated [5].
Neuromodulation with electrical stimulation is an alternative and targets specific nerves in the sacral plexus that control pelvic floor function and bladder function. Despite its effectiveness, the therapeutic impact of sacral nerve stimulation (SNS) has been limited due to invasiveness, associated costs, and its limitations in older adult patients and those who have several medical comorbidities [6].
Other stimulation ways with non-implanted electrodes can be delivered invasively or non-invasively [7]. Percutaneous tibial nerve stimulation (PTNS) is a neuromodulation technique that delivers retrograde stimulation to the sacral nerve plexus via a needle electrode inserted into the ankle, cephalad to the medial malleolus, an anatomical area recognized as the bladder center [7]. Transcutaneous tibial nerve stimulation (TTNS) is less invasive than percutaneous stimulation, but reproduces its effectiveness while minimizing its constraints and its risk of infection [7]. Thus, TTNS is an intermediate treatment between drug and surgical treatments. There is no long-term study reporting the persistence, efficacy, and tolerability with TTNS treatment.
The aim of the present study was to evaluate the long-term outcomes for patients receiving TTNS for an anticholinergic refractory overactive bladder. The primary objective of the present study was to assess the long-term persistence of treatment. The secondary objectives were to assess the long-term efficacy of TTNS, to identify the reasons for TTNS therapy discontinuation and predictive factors for treatment continuation.
Methods
We performed a prospective observational study of all consecutive patients treated for OAB persistent after first-line anticholinergic treatment from November 2010 to May 2014 in a single university hospital, with ≥ 24 months follow-up. All patients had a complete urological evaluation comprising physical examination, urine culture, bladder diary, urethrocystoscopy, and urodynamic investigations.
To be eligible for participation in the study, patients had to be 18 years of age or older, have a diagnosis of idiopathic or neurogenic refractory OAB by a physician, and have a history of medication for OAB. We excluded patients with previous surgery for OAB (sacral neuromodulation or intradetrusor injections of botulinum toxin), acute urinary tract infection on urine culture at baseline, pregnancy, bladder outlet obstruction, local trophic lesion on the site of stimulation, unable to follow the treatment regimen at home, and contraindications for TTNS (mostly implanted items caution: pacemaker, leg prosthesis).
Patients were not prescribed antimuscarinics during their participation in the study. Informed consent was obtained from all individual participants included in the study. The institutional review board approval was already obtained throughout our short-term efficacy study.
Transcutaneous posterior nerve stimulation techniques
TTNS was performed with a URO stim 2 stimulation device and electrodes pads (Schwa-Medico, Rouffach, France). Electrodes were positioned approximately 5 cm above the medial malleolus, behind the medial tibial edge, and connected to the stimulator. Bipolar stimulation was set to a frequency of 10 Hz and amplitude adjusted below the patient’s discomfort threshold. The first session was performed at the hospital with a urology nurse specialist. During this consultation, patient understanding of the technique was checked. It was also assessed whether or not the patient was able to follow this treatment at home. Subsequently, the protocol consisted of daily 20 min stimulation at home.
Follow-up
Patients were seen at 3 months to assess treatment efficacy. Subsequent follow-up was on an individualized basis. They were proposed to be seen routinely in the outpatient department between treatments every 3 months with a urology nurse specialist.
Patient characteristics
The following data were evaluated: gender, age, body mass index (BMI), OAB etiology, detrusor overactivity, and bladder capacity upon urodynamic investigation. Stimulation effectiveness was assessed using standardized questionnaires at baseline, after 3 months of treatment, and after each appointment: the urinary symptom profile (USP) and specifically the OAB score of USP (USP–OAB score) [8]. Amelioration was defined as an improvement in USP score. A significant amelioration was defined as an improvement more than 50% in USP score.
Outcomes measurement
The primary outcome was the discontinuation of TTNS treatment. Persistence is defined as the overall duration of time from initiation to discontinuation of therapy. The urology nurse specialist collected data on treatment continuation, treatment efficacy (USP score), and side effects of the treatment for each appointment. Patients were invited to contact us when they stopped the therapy. If the patients stopped the TTNS, the reasons for discontinuation and subsequent alternative management plans were identified. Adverse events, concomitant morbidities, and medications were recorded during the follow-up. Patients were also interviewed for each consultation regarding constraints related to the treatment. Patients who continued TTNS at the last appointment were contacted by phone in June 2016 to assess persistence treatment and improvement. For patients lost to follow-up, we considered the last appointment as the end of the treatment.
Statistics
Categorical variables were represented as numbers (%) and compared using the Pearson’s Chi square test (for qualitative variables > 10 frequencies) or the Fisher exact test (for qualitative variables < 10 frequencies). Quantitative variables were represented as means (standard deviation) and compared using the independent samples t test. The paired t test was used to compare USP scores. A p value < 0.05 was considered statistically significant. Univariate and multivariate regression models were used to assess the influence of different variables on treatment discontinuation. Statistical analysis was performed on the BiostaTGV website (http://marne.u707.jussieu.fr/biostatgv/).
Results
Patient characteristics
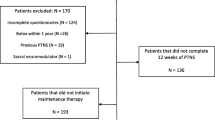
Among 103 consecutive patients, 6 were excluded for not following the treatment. Then, 97 consecutive patients were treated with TTNS: 20 (21%) were men and 77 (79%) were women, with a mean age of 58.4 ± 16.6 years. Three (3%) patients died of a nonrelated cause; their TTNS treatment persistence was, respectively, 3, 6 and 14 months. Ten patients were lost to follow-up. (Figure 1: flowchart showing the study population selection and Table 1 reports the baseline characteristics of the population.)
TTNS persistence and predictive factors for treatment persistence
The mean follow-up was 39.3 (25–65) months and mean TTNS persistence was 8.3 (1–40) months). Persistence was ≥ 12 months for 28 patients (29%) and ≥ 18 months for 16 patients (16%). Figure 2 shows the timeline of patient’s proportion still having TTNS.
Risk factors of early TTNS discontinuation
At 3 months, 24 (28.9%) patients stopped TTNS. A basal USP–OAB score superior to 11 was the only predictive factor of early treatment failure (p = 0.014) in univariate analysis, but not in multivariate analysis (Table 2).
Long-term treatment efficacy
After a mean follow-up of 39.3 months, 14 (16.9%) patients continued TTNS. We did not identify any risk factor for treatment discontinuation after an initial treatment success (Table 3).
Reasons for TTNS discontinuation
The reasons for which the 70 patients stopped their treatment at the end of the study were: the lack of sufficient symptom relief for 59 (70%) patients, compliance difficulty for 5 (6%) patients, and becoming asymptomatic for 6 (8%) patients.
Tolerability of TTNS
Patients reported no adverse events to TTNS and did not consider it painful. No patient stopped treatment because of constraints related to its implementation.
Discussion
There are several publications relating to the persistence, efficacy, and safety of PTNS in the treatment of resistant OAB. However, the only available publications about TTNS in most of the published series are short term and deal with short-term efficacy and tolerability issues.
Our study reported the outcomes of TTNS in a ‘real world’ situation. Almost two-thirds of the patients stopped the treatment after 10 months due to lower efficacy for most of them.
The 3 months efficacy rate of 71.6% in the present study is consistent with published data, including patients with idiopathic or neurogenic detrusor overactivity (IDO or NDO). Tibial nerve stimulation might be effective and safe for treating both neurogenic and idiopathic lower urinary tract dysfunction [9, 10]. In our previous study, we found that TTNS was successful in 23/43 (53%) patients following 1 month treatment for OAB after the failure of a first-line anticholinergic treatment; the only predictive factor of success was the bladder capacity [10]. De Seze et al. studied the clinical efficacy of TTNS as first-line treatment for adults with OAB secondary to multiple sclerosis patients on urgency episodes and incontinence. In this specific population, clinical improvement was reported in 82.6 and 83.3% of patients at 1 and 3 months, respectively [9]. Schreiner et al. reported subjective satisfaction in patients > 60 years who were in first-line treatment for OAB and received TTNS in addition to physiotherapy and education regarding voiding habits. Symptom improvement was higher in patients with TTNS than in patients treated with physiotherapy and bladder retraining only (68 vs 34.6%; p = 0.017) [11].
In our study, mean TTNS persistence was 8.3 months, it was over 12 months for 28 patients (29%), and over 18 months for 16 patients (16%).
Treatment persistence is an important consideration for clinicians when managing chronic conditions like OAB. Multiple publications have reported the effectiveness of PTNS for various urinary problems [12,13,14,15]. The duration of response demonstrates the effectiveness of PTNS as a viable, long-term therapy for overactive bladder until 3 years [16]. PTNS increased cystometric capacity and delayed the onset of detrusor overactivity. Cystometry seemed useful to select best candidates for PTNS: patients without detrusor overactivity or with late detrusor overactivity onset [14]. Amarenco et al. described urodynamic modifications after TTNS for clinical OAB population and documented detrusor overactivity. They reported a significant improvement for the first involuntary detrusor contraction and for maximum cystometric capacity [17].
In their patient preference study, Hashim et al. showed that perception of treatment effectiveness was associated with the choice of the most preferred treatment; then, among the 29 patients perceiving PTNS to be the most effective, 86% chose PTNS. For patients who only had experience with oral medications, the most preferred treatment option was PTNS in 56.7%, SNS in 34%, and Botox in 9.4% [18].
Electrical stimulation is a promising treatment for OAB, and combining it with other treatments may be beneficial. TTNS and oxybutynin combination was assessed by Souto et al. They assessed 75 women with a clinical complaint of OAB and reported that those treated with TTNS only or in association with oxybutynin presented longer symptom improvement than patients treated with oxybutynin only [19].
In this study, all patients rented the stimulator during the first month of treatment and bought it in case of efficacy. In France, the price of the stimulator is around 298 euros and the price of electrodes pads is around 10 euros for 1 month of treatment. The costs are higher than medical treatments of OAB (105 euros for 1 month of treatment with oxybutynin). However, costs seem reasonable with regard to the non-invasiveness of the treatment and its efficacy.
The present study has a few limitations due to the lack of a placebo group and the lack of objective urodynamic data after treatment. Secondly, this is a single-center setup; however, it provided a centralized and standardized follow-up for all the patients.
We only evaluated the persistence of treatment, but not the compliance; compliance is measured as administered doses per defined period of time. Despite having asked patients about treatment observance, we have no objective data regarding the quality of its implementation.
We chose to include all patients with OAB resistant to anticholinergic treatment, even patients for whom urodynamic investigation found an absence of detrusor overactivity. Nevertheless, detrusor overactivity was not a predictive factor of treatment success or failure.
In addition, a limitation of our investigation includes the loss to follow-up during the course of the study. To address this limitation, we performed an intent-to-treat analysis on the primary end point: all the patients were analyzed and we considered the last appointment as a discontinuation therapy for lost to follow-up patients.
Conclusions
This series from a university hospital confirms the utility of TTNS as a treatment method for patients with resistant OAB. In the long term, few patients continued with therapy, mostly because of a decreased effectiveness with time.
References
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20. https://doi.org/10.1002/nau.20798
Irwin DE, Milsom I, Hunskaar S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50:1306–1315
Madhuvrata P, Cody JD, Ellis G et al (2012) Which anticholinergic drug for overactive bladder symptoms in adults. Cochrane Database Syst Rev 1:CD005429. https://doi.org/10.1002/14651858.cd005429.pub2
D’Souza AO, Smith MJ, Miller L-A et al (2008) Persistence, adherence, and switch rates among extended-release and immediate-release overactive bladder medications in a regional managed care plan. J Manag Care Pharm JMCP 14:291–301
Abrams P, Andersson KE, Birder L et al (2010) Fourth international consultation on incontinence recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn 29:213–240. https://doi.org/10.1002/nau.20870
Zinkgraf K, Quinn AO, Ketterhagen D et al (2009) Percutaneous tibial nerve stimulation for treatment of overactive bladder and urinary retention in an elderly population. Urol Nurs 29:30–34
Stewart F, Gameiro LF, El Dib R et al (2016) Electrical stimulation with non-implanted electrodes for overactive bladder in adults. Cochrane Database Syst Rev 12:CD010098. https://doi.org/10.1002/14651858.cd010098.pub4
Haab F, Richard F, Amarenco G et al (2008) Comprehensive evaluation of bladder and urethral dysfunction symptoms: development and psychometric validation of the urinary symptom profile (USP) questionnaire. Urology 71:646–656. https://doi.org/10.1016/j.urology.2007.11.100
De Sèze M, Raibaut P, Gallien P et al (2011) Transcutaneous posterior tibial nerve stimulation for treatment of the overactive bladder syndrome in multiple sclerosis: results of a multicenter prospective study. Neurourol Urodyn 30:306–311. https://doi.org/10.1002/nau.20958
Ammi M, Chautard D, Brassart E et al (2014) Transcutaneous posterior tibial nerve stimulation: evaluation of a therapeutic option in the management of anticholinergic refractory overactive bladder. Int Urogynecol J 25:1065–1069. https://doi.org/10.1007/s00192-014-2359-0
Schreiner L, dos Santos TG, Knorst MR, da Silva Filho IG (2010) Randomized trial of transcutaneous tibial nerve stimulation to treat urge urinary incontinence in older women. Int Urogynecol J 21:1065–1070. https://doi.org/10.1007/s00192-010-1165-6
Govier FE, Litwiller S, Nitti V et al (2001) Percutaneous afferent neuromodulation for the refractory overactive bladder: results of a multicenter study. J Urol 165:1193–1198
Klingler HC, Pycha A, Schmidbauer J, Marberger M (2000) Use of peripheral neuromodulation of the S3 region for treatment of detrusor overactivity: a urodynamic-based study. Urology 56:766–771
Vandoninck V, van Balken MR, Finazzi Agrò E et al (2003) Percutaneous tibial nerve stimulation in the treatment of overactive bladder: urodynamic data. Neurourol Urodyn 22:227–232. https://doi.org/10.1002/nau.10111
Peters KM, MacDiarmid SA, Wooldridge LS et al (2009) Randomized trial of percutaneous tibial nerve stimulation versus extended-release tolterodine: results from the overactive bladder innovative therapy trial. J Urol 182:1055–1061. https://doi.org/10.1016/j.juro.2009.05.045
Peters KM, Carrico DJ, Wooldridge LS et al (2013) Percutaneous tibial nerve stimulation for the long-term treatment of overactive bladder: 3 years results of the STEP study. J Urol 189:2194–2201. https://doi.org/10.1016/j.juro.2012.11.175
Amarenco G, Ismael SS, Even-Schneider A et al (2003) Urodynamic effect of acute transcutaneous posterior tibial nerve stimulation in overactive bladder. J Urol 169:2210–2215. https://doi.org/10.1097/01.ju.0000067446.17576.bd
Hashim H, Beusterien K, Bridges JFP et al (2015) Patient preferences for treating refractory overactive bladder in the UK. Int Urol Nephrol 47:1619–1627. https://doi.org/10.1007/s11255-015-1100-3
Souto SC, Reis LO, Palma T et al (2014) Prospective and randomized comparison of electrical stimulation of the posterior tibial nerve versus oxybutynin versus their combination for treatment of women with overactive bladder syndrome. World J Urol 32:179–184. https://doi.org/10.1007/s00345-013-1112-5
Author information
Authors and Affiliations
Contributions
Author contributions
P-AL: data collection and analysis, and manuscript writing/editing. EB: project development and data collection. SL: manuscript editing. ARA: project development. PB: project development, manuscript editing and data analysis. JC: data analysis and manuscript writing/editing
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Leroux, PA., Brassart, E., Lebdai, S. et al. Transcutaneous tibial nerve stimulation: 2 years follow-up outcomes in the management of anticholinergic refractory overactive bladder. World J Urol 36, 1455–1460 (2018). https://doi.org/10.1007/s00345-018-2296-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2296-5