Abstract
Purpose
Prospective evaluation of independent risk factors for failure of the retrourethral transobturator sling suspension (RTS) with special attention on sphincter function and surgical technique.
Methods
A total of 189 patients with postprostatectomy stress urinary incontinence (SUI) were treated with RTS (AdVance® sling) in a prospective clinical study with a mean follow-up of 20.8 months. Eleven patients were lost to follow-up. Uni- and multivariate analyses were performed to identify independent risk factors for RTS failure. The success rate was defined as cured (no pad use or one dry ‘security’ pad) or improved (one to two pads and pad reduction ≥50%).
Results
At a mean follow-up of 20.8 months, the overall success rate was 73.1%. Multivariate analysis revealed that weak residual function and incomplete closure of the sphincter (OR, 29.0), no elongation of the coaptive sphincter zone (OR, 26.9), no sling tunnelling (OR, 22.6) and use of resorbable sutures with a small number (≤4) of stitches (OR, 8.4) are significant predictors for RTS failure.
Conclusions
Preoperative selection of the patients with regard to residual sphincter function and a special attention on better sling fixation may increase RTS efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, several minimally invasive slings for treatment of postprostatectomy stress urinary incontinence (SUI) were introduced. The retrourethral transobturator sling suspension (RTS), (AdVance®, American Medical Systems, Minnetonka, USA), was introduced in 2006 [1–3]. RTS failure occurs in 20–45.5% [4–7]. Several factors are accused to have a negative impact on sling efficacy: e.g. continence status [5, 6, 8], pelvic irradiation, adjuvant pelvic radiotherapy (AR) and previous urethral stricture surgery [6, 8, 9], previous invasive incontinence therapy, residual sphincter function and surgical technique of RTS placement [1, 3, 5]. However, they have not been clearly evaluated.
Detailed knowledge of predictors for RTS failure could optimize counselling of patients considering RTS procedure and improve clinical outcome.
The aim of this study was to identify independent risk factors for RTS failure.
Patients and methods
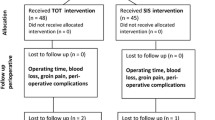
Between February 2006 and December 2009, 189 consecutive patients with SUI who underwent RTS were evaluated in a prospective, sequential clinical study. Eleven patients were excluded from the analysis due to lost to follow-up. A detailed description of inclusion and exclusion criteria can be found elsewhere [5].
All patients completed appropriate consented forms. Data were collected according to the database approved by the local institutional review board.
Patients were evaluated by two independent investigators who did not perform RTS implantations.
Preoperatively, demographics, comprehensive medical history, history of AR, surgery for urethral or bladder neck stenosis, previous incontinence therapy, uroflowmetry, postvoid residual urine (PVR), daily pad use, 1-h pad test, urodynamics and urethroscopy were performed. The impact of SUI on quality of life was assessed by questionnaires (Incontinence Quality of Life Scale (I-QOL) and Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF)).
Residual sphincter function, coaptive response, closure of EUS and coaptive sphincter zone [3, 10] were evaluated by the ‘repositioning test’ [5, 11]. The closure of the sphincter was assessed as incomplete if the lumen of the membranous urethra was not completely occluded during manual midperineal repositioning. The elongation of the coaptive sphincter zone is described as increase in the functional lengths of the urethra due to coaptive response of the sphincter during manual midperineal repositioning and additional active sphincter closure. The sphincter with still-remaining good residual sphincter function showed autonomous voluntary contractions in concentric manner with duration for at least a few seconds.
The ICS classification [12, 13] was used for the evaluation of incontinence severity. To assess the influence of severe incontinence on RTS, outcome patients with mild incontinence (1–2 pads) were opposed to them with moderate (3–5 pads) and severe incontinence (>5 pads).
RTS implantation was performed according to the previously described surgical technique [1, 5, 14] by two high-experienced and two less experienced surgeons (<25 procedures). For better sling fixation, the sling was fixed to the urethral bulb with at least four stitches of nonresorbable sutures along the midline beginning at the middle part of the sling instead of using long-term resorbable sutures at the distal border and the middle part of the sling. In addition, the sling arms were tunnelled subcutaneously to ensure better early grip and to prevent early postoperative sling slippage (Fig. 2).
Postoperatively, urethral catheter was removed routinely on day 2 or 3. Patients with acute urinary retention (AUR) (PVR > 150 ml) were re-catheterized. In all cases, catheter was removed without further treatment within 12 weeks (PVR ≤ 50 ml).
Postoperatively, patients were scheduled at 4 weeks, 3 and 6 months as well as every 6 months thereafter. At follow-up visits, evaluation of daily pad use, 1-h pad test, PVR, uroflowmetry, I-QOL and ICIQ-UI SF questionnaires were performed. Patients who were not able to come to the hospital were all followed by using standardized questionnaires which were sent to them by mail.
The success rate was defined as cured (no pad use or one dry “security” pad) or improved (1–2 pads and pad reduction ≥50%) [5]. All other cases were defined as a failure.
The SPSS® statistical software for Windows (v. 17.0, SPSS Inc., Chicago, IL, USA) was used for data analysis. The Mann–Whitney and Chi-square tests were performed to compare the success and failure groups by demographic, clinical, surgical and follow-up variables. Statistically significant independent variables of the univariate analysis were included for multivariate assessment by bivariate logistic regression. For entering and removing of explanatory variable, the significance level was considered <0.05 and <0.10, respectively. The goodness of fit of the final model was assessed using the Hosmer–Lemeshow test. The ability of the final model to predict the risk of RTS failure was assessed using probabilities on the receiver operating characteristic (ROC) curve.
Results
The overall success rate was 73.1% (133 of 178 patients). The mean follow-up was 20.8 ± 9.8 months (12–43 months). Pre- and postoperative data are listed in Table 1.
Between success and failure groups were no significant differences for age, body mass index, type of prostate surgery, time interval between prostate surgery and sling implantation, previous treatment of incontinence, history of bladder neck stenosis, severity of incontinence, daily pad use, urine loss in 1-h pad test, maximal flow rate, type of anaesthesia, AUR and hospitalization time.
Preoperative severity of incontinence had no influence on success (P = 0.089). However, grouping them in mild (1–2 pads) versus moderate (3–5 pads) and severe (>5 pads) incontinence groups revealed significant difference between success and failure groups (P = 0.04).
AR, moderate and severe incontinence, weak EUS function, no elongation of the coaptive zone and incomplete closure of EUS were found to be significant preoperative risk factors for failure by univariate analysis.
In the univariate assessment, using nonresorbable sutures, more stitches, surgeon’s experience (>25 RTS), sling tunnelling and a combination of nonresorbable sutures with at least four stitches had a significant influence on success rate.
AUR was observed in 20% (27 of 133 patients) in the success group and in 9% (4 of 45 patients) in the failure group. However, this difference was not significant (P = 0.083).
Significant changes in urine loss (1-h pad test: 169.3 ± 162.4 vs. 21.3 ± 59.2, P < 0.001 and daily pad use: 5.4 ± 3.3 vs. 1.7 ± 2.4, P < 0.001) were observed. ICIQ-UI SF score decreased (16.6 ± 3.8 vs. 9.5 ± 8.9, P < 0.001) and I-QOL score increased significantly (54.6 ± 18.1 vs. 81.1 ± 23.6, P < 0.001).
The results of multivariate analysis are presented in Table 2. Although AUR had no significant influence on success in univariate analysis, it has been included in the logistic regression model due to its importance. A few variables such as sutures materials and number of stitches as well as EUS function and closure were grouped as one variable to increase the number of observations and to give a reliable estimation. Based on the outcome from the logistic regression analysis, use of resorbable sutures and small number of stitches (< 4 stitches), no sling tunnelling, weak function and incomplete closure of EUS as well as no elongation of the coaptive sphincter zone were identified to be significant independent risk factors for RTS failure (Table 2).
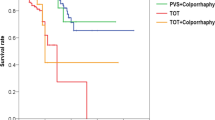
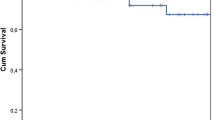
The ROC curve was generated using computed probabilities from the final model to estimate its power in predicting RTS failure (Fig. 1). The ROC area (AUC) was 0.96 (95% CI, 0.93–0.99).
Discussion
Reported RTS failure rates are between 9.3% and 45.5% [3–8, 15]. A history of AR has been assumed to be risk factor for failure in a few studies [3, 8, 11, 16]. Type of prostate surgery, a history of urethral surgery due to bladder neck stenosis or urethral stricture, previously invasive incontinence treatment and a short learning curve have been discussed to affect RTS outcome. Selection of patients with only mild and moderate SUI [5–9] and urine loss <200 g in the 24-h pad test [8] may increase the RTS efficacy. Considering the underlying mechanism of RTS action, coaptive response, sufficient residual function and closure of EUS are assumed to be important predictors for success [1, 3, 10, 15].
However, studies concerning evaluation of independent risk factors for RTS failure are lacking.
In this study, we prospectively evaluated RTS outcome in a large group of patients (n = 178) with special focus on sphincter function and surgical technique to identify independent risk factors for failure.
On multivariate logistic regression analysis, resorbable sutures and small number of stitches (<4 stitches), no sling tunnelling, weak function and incomplete closure of EUS as well as no elongation of the coaptive sphincter zone are independent risk factors predicting RTS failure. The logistic regression model shows excellent discriminative ability in prediction of probabilities for RTS failure. The AUC value allows prediction of RTS failure in 96% of all cases.
At follow-up visits, several patients reported physical activity in the first 6 weeks followed by SUI recurrence. In these cases, RTS may be caused by sling slippage. Therefore, high rates of RTS failure at short-term follow-up [4, 7] may be associated with early postoperative physical activity resulting in sling slippage [2, 14, 17]. Based on this knowledge, we improved the surgical technique with special focus on better sling fixation using nonresorbable sutures instead of resorbable sutures with at least four stitches [14]. In addition, the technique of sling tunnelling was introduced as shown in Fig. 2 [5]. In the presented study, we were able to confirm that sling tunnelling and using nonresorbable sutures with at least four stitches are independent predictors for success.
In addition, our data suggest that careful preoperative patient selection should be performed with special attention to sufficient residual EUS function and coaptive response, complete closure and ability for elongation of the coaptive sphincter zone. These data support recent discussion [1–3, 10].
Recently reported [8] association of previous surgery for urethral stenosis with RTS failure is not confirmed by our data. It could be explained by superior importance of the ability for complete closure and elongation of the coaptive sphincter zone for outcome. For this subgroup, further studies are needed.
In the univariate analysis, severity of incontinence, experience of the surgeon and AR showed a significant negative impact on success rate. However, there was no significance by logistic regression analysis. Impact of incontinence severity was found to be significant in a few studies [6–8], whereas no correlation was identified in other publications [4, 5]. Additionally, RTS outcome affected by AR was suggested [4–6, 8]. The number of patients in most of these studies was too small to show significant difference. Our group [16] reported about a lower success rate in patients with AR by univariate analysis. The present data indicate that patients with sufficient residual sphincter function and coaptive sphincter zone can benefit from RTS placement.
In contrast to univariate assessment, experience of the surgeon is found not to be predictive for failure by multivariate analysis. One explanation may be that the surgical technique itself and the EUS function appear to be superior in prediction of RTS failure. In addition, the less experienced surgeons performed sling implantation together with a high-experienced surgeon.
AUR had no influence on RTS outcome in uni- and multivariate analyses. These data support previously reported results [1, 2, 5, 11].
Limitations of the study are empirical information about postoperative patient’s physical activity, possible overestimation of ability of the model to predict RTS failure using original sample, unique data of only one centre, small number of observations in categories of some variables and qualitative evaluation of sphincter function.
Conclusion
Preoperative assessment of sphincter function, coaptive response, closure and elongation of the coaptive sphincter zone, a focus on better sling fixation using sling tunnelling and nonresorbable sutures with at least four stitches may increase the efficacy of RTS outcome. Patients with incomplete closure and low function of the external urethral sphincter as well as missing elongation of the coaptive sphincter zone are at risk for worse RTS outcome.
Abbreviations
- RTS:
-
Retrourethral transobturator sling
- SUI:
-
Postprostatectomy stress urinary incontinence
- AR:
-
Adjuvant pelvic radiotherapy
- PVR:
-
Postvoid residual urine
- EUS:
-
External urethral sphincter
- AUR:
-
Acute postoperative urinary retention
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the receiver operating characteristic curve
References
Rehder P, Gozzi C (2007) Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol 52:866–867
Davies TO, Bepple JL, McCammon KA (2009) Urodynamic changes and initial results of the AdVance male sling. Urology 74:354–357
Rehder P, Mitterberger MJ, Pichler R et al (2010) The 1 year outcome of the transobturator retroluminal repositioning sling in the treatment of male stress urinary incontinence. BJU Int (2010, in press). doi:10.1111/j.1464-410X.2010.09.400.x
Cornel EB, Elzevier HW, Putter H (2010) Can advance transobturator sling suspension cure male urinary postoperative stress incontinence? J Urol 183:1459–1463
Bauer RM, Mayer ME, Gratzke C et al (2009) Prospective evaluation of the functional sling suspension for male postprostatectomy stress urinary incontinence: results after 1 year. Eur Urol 56:928–933
Cornu JN, Sèbe P, Ciofu C et al (2009) The AdVance transobturator male sling for postprostatectomy incontinence: clinical results of a prospective evaluation after a minimum follow-up of 6 months. Eur Urol 56:923–927
Gill BC, Swartz MA, Klein JB et al (2010) Patient perceived effectiveness of a new male sling as treatment for post-prostatectomy incontinence. J Urol 183:247–252
Cornu JN, Sèbe P, Ciofu C et al (2010) Mid-term evaluation of the transobturator male sling for post-prostatectomy incontinence: focus on prognostic factors. BJU Int (2010, in press). doi: 10.1111/j.1464-410X.2010.09765.x
Montague DK (2009) Males slings: compressive versus repositioning. Eur Urol 56:934–936
Rehder P, von Gleissenthall GF, Pichler R, Glodny B (2009) The treatment of postprostatectomy incontinence with the retroluminal transobturator repositioning sling (Advance®): lessons learnt from accumulative experience. Arch Esp Urol 62:860–870
Bauer RM, Mayer ME, May F et al (2010) Complications of the AdVance transobturator male sling in the treatment of male stress urinary incontinence. Urology 75:1494–1498
Abrams P, Blaivas JG, Stanton SL et al (1988) The standardisation of terminology of lower urinary tract function. The international continence society committee on standardisation of terminology. Scand J Urol Nephrol 114:5–19
Abrams P, Cardozo L, Fall M et al (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61:37–49
Soljanik I, Becker A, Stief CG, Cozzi G, Bauer R (2010) Repeat retrourethral transobturator sling in the management of recurrent postprostatectomy stress urinary incontinence after failed first male sling. Eur Urol (2010, in press). doi:10.1016/j.eururo.2010.08.034
Bauer RM, Soljanik I, Füllhase C et al (2010) Mid-term results for the retroluminar transobturator sling suspension for stress urinary incontinence after prostatectomy. BJU Int (2010, in press). doi:10.1111/j.1464-410X.2010.09729.x
Bauer RM, Mayer M, Gratzke C et al (2009) Functional retrourethral sling for male stress urinary incontinence after radical prostatectomy and adjuvant radiotherapy: are the results as good as in patients without radiotherapy? Urology 74: S230 UP-1.189
Rapp DE, Reynolds WS, Lucioni A, Bales GT (2007) Surgical technique using AdVance sling placement in the treatment of postprostatectomy urinary incontinence. Int Braz J Urol 33:231–237
Acknowledgments
The study has not been financially supported.
Conflict of interest
Christian Gozzi holds the intellectual property as a co-inventor of the procedure. Christian Gozzi declares consultancy work, lectures and participation in clinical trials for AMS. Ricarda M. Bauer declares lectures for AMS. All authors declare that no funding or other agreement has limited their ability to fairly complete and publish this data, and they had full control of the primary data. There has been no extra-institutional funding for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soljanik, I., Gozzi, C., Becker, A.J. et al. Risk factors of treatment failure after retrourethral transobturator male sling. World J Urol 30, 201–206 (2012). https://doi.org/10.1007/s00345-011-0671-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-011-0671-6