Abstract
Objectives
Topical steroids have been advocated as an effective alternative treatment to circumcision in boys with phimosis. We evaluated the effectiveness of topical steroid therapy compared to a placebo neutral cream in 240 patients with phimosis.
Methods
A prospective study was carried out over a 24-months period, on an out-patient basis on two groups of patients with phimosis. One-hundred twenty patients applied a steroid cream twice a day for 4 weeks, and another group of 120 pts used a placebo cream twice a day for 4 weeks. Patients were assigned to either group by a computer-generated random choice.
Results
All patients in our series completed the two treatment periods without interruption. At a median follow-up of 20 months (6–30 months) therapeutic success was obtained in 43.75% (99/240) of cases, independently of the protocol. In particular, therapeutic success was obtained in 65.8% (79/120) of cases in the steroids group and in 16.6% (20/120) of cases in the placebo group, the difference being statistically significant (P < 0.0001, Mann–Withney test).
Conclusion
Our study shows that topical steroids represent a good alternative to surgery in case of phimosis. Steroid therapy using monometasone furoate 0.1% in our series gave better results that placebo with an overall efficacy of 65.8%. In patients where a phimotic ring persist after steroid therapy, circumcision is mandatory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of male newborns (96%) have physiological phimosis [1, 2]. Within 2–3 years, the foreskin detaches spontaneously from the glans [3]. This process is mainly linked to maternal daily washing which, together with intermittent erections, allows the foreskin to separate and produce a physiological retraction. In more than 80% of uncircumcised boys the foreskin can be retracted over the glans by the age of 3 years [1]. Circumcision has long been advocated as an effective way to treat phimosis. In the last 5 years several articles have reported the use of topical corticosteroids as an alternative treatment for phimosis, with high success rates (67–95%) [3–6]. However, no randomized prospective controlled trials on a large number of patients have been published on this topic. In this study we compared the results of two different protocols of conservative therapy used in boys with phimosis, to try to understand whether topical steroids are more effective than placebo.
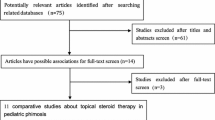
Patients and methods
Ours was a prospective study was carried out on 240 boys with phimosis, on an out-patient basis. The 240 patients with phimosis who came to our observation during a 24 months period (June 2003–2005) were divided into 8 groups of 30 patients each.
Using a computer-generated random choice, the two types of medical treatment were matched with the eight groups: four groups (for a total of 120 boys) was given a placebo cream therapy twice a day for 4 weeks; the other four groups (also comprising 120 boys) was given steroid cream therapy twice a day for 4 weeks (Table 1). In both groups the medication was applied by the parents. The dosages of steroid cream (monometasone furoate 0.1%) were based on the existing recommendations for the product.
The patients’ ages ranged between 36 months and 13 years (4.7 median). Of these, 86 had a grade V phimosis, 79 a grade IV phimosis and 75 a grade III phimosis (Table 2). Before including each patient in the study we confirmed the diagnosis of phimosis by evaluating the shape of preputium during urination in all cases.
Exclusion criteria were: partial exposure of the glans; previous operation of the penis; prior use of steroid treatment for the same pathology; recurrent episodes of balanopostitis. Steroid cream was adopted in the first group of 120 patients (50 grade V; 33 grade IV; 37 grade III), while placebo cream was adopted in the other 120 (36 grade V; 46 grade IV; 38 grade III). The results were evaluated by two paediatric surgeons unaware of the type of treatment the patients had undergone. Treatment was considered successful when the full retraction of the prepuce was achieved, otherwise the patient was scheduled for circumcision. Informed consent was obtained by the parents of the children included in the study, which had been approved by the Ethics Committee of our University.
Statistical analyses of the data were performed by means of the non-parametric test Mann–Withney; a P value < 0.001 was considered significant.
Results
All the patient in our series completed the two treatment periods without interruption. Neither group reported any untoward effects of the drugs. There were no statistical differences (ns) in terms of age between the two groups (median age 4.9 and 4.6, respectively, P = ns). A successful outcome was the attainment of a normal looking foreskin that retracted in an appropriate fashion, thus doing away with the need for surgery. At a median follow-up of 20 months (6–30 months), therapeutic success was obtained in 43.75% (99/240) cases, independently of the protocol. In particular, therapeutic success was obtained in 65.8% (79/120) of cases in the steroids group, and in 16.6% (20/120) of cases in the placebo group; this result has a strong statistical significance (P > 0.0001).
Results for each grade of phimosis and the type of therapy adopted are reported in Table 3. We also compared the results of steroid therapy in the different grades of phimosis: grade III versus grade IV P < 0.0126 (statistically significant); grade III versus grade V P < 0.0042 (statistically significant); grade IV versus grade V P < 0.7099 (ns). The 41 patients in the steroid group and the 80 patients in the placebo group who experienced no improvement after therapy underwent a circumcision at our centre.
Discussion
Until a few years ago surgery was the only option available to patients with phimosis. Some surgeons prefer to perform foreskin sparing procedures as preputioplasty, some others a circumcision. In the last 5 years, with the introduction of topical steroids for the treatment of phimosis, surgery has become the object of debate among paediatric surgeons [7–9]. However, two main problems need to be considered in evaluating the results of topical steroids therapy in boys with phimosis: first of all there is no clear definition of phimosis in patients enrolled in the studies so far published, i.e., no differentiation between pathological phimosis and physiological non-retractile foreskin; the second problem is the absence of a large study comparing two groups of patient treated with steroid versus placebo therapy.
For this reason, in our study we first performed a grading of phimosis (5°) according to Kayaba et al. [3] (modified by our group), excluding boys with grade I and II phimosis (which never requires surgery as it may disappear spontaneously); second, the main aspect of our study is that we have comparatively studied two homogeneous groups of patients, the first treated with steroid cream and the second with a neutral placebo cream.
To understand the reasons for the good results of medical treatment, it is important to try to explain the mechanisms of action of topical steroids [1]. Three possible mechanisms have been proposed in the treatment of phimosis.
Steroids can cause thinning of the skin and improve the elasticity of the foreskin by decreasing the synthesis of hyaluronic acid, which has an antiproliferative effect on the epidermis [10, 11]. In addition, topical steroids can inhibit the production of the mediators of skin inflammation, i.e., prostaglandins and leukotrienes. Finally, the lubricant effect of the cream allows boys to retract the foreskin easily [3, 12].
The third mechanism is the only one applicable to the neutral placebo cream; this has only a lubricating effect on the foreskin, as shown in our study, where there was a low therapeutic success rate in the placebo group, with 16.6% (20/120) of patients only compared to the steroid group. In agreement with Wright et al. [12] parent and patient compliance is the key factor in predicting successful treatment. In fact in our series all the parents, after talking with our team, were extremely motivated to perform steroids therapy which influenced their children in a positive way. As a matter of fact another important point to underline is that in our series the medication was always applied by the parents, to ensure proper administration [13].
Another issue in favour of steroid therapy compared to surgery is the cost: several studies have estimated that the overall cost of topical steroid therapy is approximately 25% lower that of surgery [1, 14]. As to our results, we believe that the lower therapeutic success rate in our series (65.8%) compared to the other reports published (75, 87 and 88%) is certainly related to the large number of patients with grade IV and V phimois [1, 3, 7]. As a matter of fact, the therapeutic success in our series seems to be related to the degree of phimosis: in grade III the success rate (81%) is significantly higher than in grade IV (60.6%; P < 0.0126) and V (58%; P < 0.0042). On the contrary the difference in the results between group IV and V is not statistically significant (ns) (P < 0.7099).
Other authors have reported that steroid therapy seems to have no success in patients with severe baolanitis xerotica, who should primarily be considered for surgery; in our series we have no data on this point [1, 15].
Moreover, none of our patients reported adverse effects related to the two medications [15–18]. As to the stability of the results at the end of the treatment period, in agreement with Ashfield et al. [1], our results proved stable over time at a median follow-up of 12 months. However, in order to maintain the good results achieved, it is extremely important to stress to the parents the daily practice of genital hygiene, consisting in adequate care and cleansing of the foreskin and glans, even after withdrawal of the medication.
As for the surgical procedure to adopt in patient with phimosis, our experience was to perform a preputioplasty; however, considering that in some patients a phimotic ring persists after steroids therapy, a preputioplasty would have no therapeutic role and the only suitable surgical procedure is a circumcision. In conclusion, on the basis of our experience, we believe that steroid therapy is indicated only in patients with high-grade phimosis (III–V), as grade I and II phimois disappear spontaneously without any treatment. Topical steroids will probably become the standard conservative measure for treating phimosis in the near future.
Our study shows that topical steroids give better and more statistically significant results than placebo, with an overall efficacy of 65.8% without adverse effects. In patients where a phimotic ring persist after steroid therapy, circumcision is necessary.
References
Ashfield JE, Nickel KR, Siemens DR, MacNeily AE, Nickel JC (2003) Treatment of phimosis with topical steroids in 194 children. J Urol 169:1106–1110
Elmore JM, Baker LA, Snodgrass WT (2002) Topical steroid therapy as an alternative to circumcision for phimosis younger than 3 years. J Urol 168:1746–1750
Kayaba H, Tamura H, Kitajima S, Fujiwara Y, Kato T, Kato T (1996) Analysis of shape and retractability of the prepuce in 603 Japanese boys. J Urol 156:1813–1815
Atilla MK, Dundaro R, Odabas O, Ozturk H, Akin R, Gokcay E (1997) A nonsurgical approach to the treatment of phimosis: local nonsteroidal anti-inflammatory ointment application. J Urol 158:196–201
Golubovic Z, Milanovic D, Vukadinovic V, Rakic I, Perovic S (1996) The conservative treatment of phimosis in boys. Br J Urol 78:786–790
Kikiros CS, Beasley SW, Woodward AA (1993) The response of phimosis to local steroid application. Pediatr Surg Int 8:329–332
Chu CC, Chen KC, Diau GY (1999) Topical steroid treatment of phimosis in boys. J Urol 162:861–864
Monsour MA, Rabinovitch HH, Dean GE (1999) Medical management of phimosis in children: our experience with topical steroids. J Urol 162:1162–1167
Orsola A, Caffaratti J, Garat JM (2000) Conservative treatment of phimosis in children using a topical steroid. Urology 56:307–310
Kragballe K (1989) Topical corticosteroids: mechanisms of action. Acta Derm Venereol 151:7–10
Ng WT, Fan N, Wong CK, Leung SL, Yuen KS, Sze YS (2001) Treatment of childhood phimosis with a moderately potent topical steroid. ANZ J Surg 71:541–543
Wright JE (1994) The treatment of childhood phimosis with topical steroid. Aust N Z J Surg 64:327–330
To T, Agha M, Dick PT, Feldman W (1998) Cohort study on circumcision of newborn boys and subsequent risk of urinarytract infection. Lancet 352:1813–1817
Cuckow PM (1998) Circumcision. In: Stringer MD, Oldham KT, Mouriquand P, Howard ER (eds) Pediatric surgery and urology: long term outcomes. W. B. Saunders Co Ltd, London, pp 616–620
Krafchik BR (1995) The use of topical steroids in children. Semin Dermatol 14:70–74
MacKie RM (2004) Drug eruptions. In: Lay G, Ragon FG (eds) Clinical dermatology, Oxford University Press, New York, pp 300–310
Perry RJ, Findlay CA, Donaldson MD (2002) Cushing’s syndrome, growth impairment, and occult adrenal suppression associated with intranasal steroids. Arch Dis Child 87:45–49
Zheng PS, Lavker RM, Lehmann P, Kligman AM (1984) Morphologic investigations on the rebound phenomenon after corticosteroid-induced atrophy in human skin. J Invest Dermatol 82:345–347
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Esposito, C., Centonze, A., Alicchio, F. et al. Topical steroid application versus circumcision in pediatric patients with phimosis: a prospective randomized placebo controlled clinical trial. World J Urol 26, 187–190 (2008). https://doi.org/10.1007/s00345-007-0231-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-007-0231-2