Abstract
The discovery and targeting of genes mediating androgen-independence may lead to the development of novel therapies that delay progression of hormone refractory prostate cancer (HRPC). Clusterin is a stress-associated cell survival gene that increases after androgen ablation. Here, we review clusterin’s functional role in apoptosis and the use of antisense oligonucleotides (ASOs) against clusterin to enhance apoptosis in prostate cancer models. Immunostaining of tissue microarrays constructed from untreated and post-hormone treated radical prostatectomy specimens confirm that clusterin is highly expressed in virtually all HRPC cells, 80% of prostate cancer cells after neoadjuvant hormone therapy, but is low or absent (<20%) in untreated specimens. Overexpression of clusterin in LNCaP cells confers resistance to both androgen ablation and chemotherapy. Clusterin ASOs reduced clusterin levels in a dose-dependent and sequence-specific manner. Adjuvant treatment with murine clusterin ASOs after castration of mice bearing Shionogi tumors decreased clusterin levels, accelerated apoptotic tumor regression, and significantly delayed the recurrence of androgen-independent tumors. A human clusterin ASO targeting the translation initiation site and incorporating MOE-gapmer backbone (OGX-011) synergistically enhanced the cytotoxic effects of paclitaxel in human xenografts of prostate, renal cell, bladder, and lung cancer. Clusterin, is an anti-apoptosis protein upregulated in an adaptive cell survival manner by androgen ablation and chemotherapy that confers resistance to various cell death triggers. Suppression of clusterin levels using ASOs enhances cell death following treatment with androgen ablation, radiation, and chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Androgen withdrawal is the only effective form of systemic therapy for men with advanced prostate cancer, producing a symptomatic and/or objective response in 80% of patients. Unfortunately, androgen-independent (AI) progression and death occurs within a few years in the majority of these cases [1, 2]. Two recently completed phase III trials comparing docetaxel to mitoxantrone report a 20% prolongation in survival, 45–50% PSA response rates, delayed time to progression, and improved pain responses in men with hormone refractory prostate cancer (HRPC) [3, 4]. These improvements are significant but modest, and novel therapeutic strategies that target the molecular basis of androgen and chemo-resistance are required. One rational treatment strategy would incorporate agents that target stress-associated increases in gene expression precipitated by androgen withdrawal or chemotherapy in order to enhance treatment-induced apoptosis and delay emergence of the androgen-independent (AI) phenotype or progression of HRPC.
Progression to androgen independence is a complex process involving variable combinations of clonal selection [5], adaptive upregulation of anti-apoptotic survival genes [6, 7, 8, 9, 10], androgen receptor (AR) transactivation in the absence of androgen from mutations or increased levels of co-activators [11, 12] and alternative growth factor pathways, including Her2/neu, EGFR, and IGF-1 [12, 13, 14], leading to dysregulated AR pathways [15, 16, 17]. Improved understanding of specific mechanisms mediating AI progression and new therapeutic strategies designed to inhibit the emergence of this phenotype are needed before additional gains in survival can be realized.
Resistance to various hormonal and chemotherapies develops, in part, from alterations in the apoptotic machinery, due to increased activity of antiapoptotic pathways or expression of antiapoptotic genes. Research during the past decade has identified many gene products that may promote progression and resistance by inhibiting apoptosis. Of special relevance to the development of AI progression and HRPC are those survival proteins upregulated after apoptotic triggers like androgen ablation that function to inhibit cell death. Proteins fulfilling these criteria include antiapoptotic members of the Bcl-2 protein family, clusterin, Hsp27, and IGFBP-2 and IGFBP-5. Bcl-2 levels increase after androgen withdrawal and during AI progression [6, 18, 19, 20, 21, 22], and Bcl-2 antisense oligonucleotides (ASOs) can enhance cancer cell death after treatment with androgen withdrawal or chemotherapy [18, 23, 24]. Similar data has been published for the targeted suppression of Hsp27 [25] and IGFBP-2 [10, 26] and IGFBP-5 [9, 26, 27]. In this review, we will summarize the role of the apoptosis-associated protein, clusterin, in the development of androgen- and chemoresistance, and describe the preclinical pharmacology data and early clinical trials of OGX-011, a second generation ASO targeting clusterin.
Regulation of clusterin expression
Also known as testosterone-repressed prostate message-2 (TRPM-2), apolipoprotein J, or sulfated glycoprotein-2, clusterin is associated with a wide variety of physiological and pathological processes, including reproduction [28], Alzhiemer’s [29], renal diseases such as membranous glomerulonephritis, gentamicin nephrotoxicity, and ureteric obstruction [30]. High levels of clusterin are associated with numerous tumors including prostate [31], lung [32], breast [33, 34], lymphoma [35], and renal cell carcinoma [36]. Clusterin levels increase dramatically during castration-induced apoptosis in rat prostate epithelial cells [37], in AD Shionogi tumors [7, 8], and human prostate cancer CWR22 [38] and PC82 [39] xenografts. Moreover, clusterin levels increase and decrease during each cycle of intermittent androgen suppression in the Shionogi tumor model (Fig. 1).
Immunohistochemical analysis of clusterin protein expression in a tissue microarray of human prostate cancer tissues obtained from radical prostatectomy specimens before and after androgen withdrawal. Clusterin staining in specimens from NHT-treated patients increased in intensity (+3–+4) in 80% of cancer cells compared to absent (0) to low intensity staining (+1–+2) in 20% of cancer cells in non-NHT treated specimens
In the prostate gland, clusterin mRNA was originally cloned as TRPM-2 from regressing rat prostate where it was subsequently shown by in situ hybridization to be expressed in dying epithelial cells [40]. Subsequently, however, clusterin was shown to be an apoptosis-associated, rather than androgen-repressed, gene; clusterin upregulation did not occur when calcium channel blockers were used to inhibit castration-induced apoptosis and Shionogi tumor regression [7]. Support for clusterin having an active role in promoting apoptosis is largely derived implicitly from its direct association with a great variety of dying tissues, such that measurement of clusterin is an accepted marker of apoptotic cell death [41, 42, 43, 44, 45, 46, 47].
Clusterin expression is transcriptionally activated by heat shock factor (HSF)-1 [48], and hence increases following a diverse variety of stressors, including cytotoxic chemotherapy [49], radiation [50], heat shock [48], and androgen [7, 8] or estrogen [33] withdrawal in hormone-dependent tumors. Criswell et al. [6] demonstrated that P53, a tumor suppresser gene, can suppress sCLU induction response, which goes well with the fact that P53 is an activator of apoptosis, unlike sCLU [51]. Up-regulation of CLU has been reported after treatment with vitamin D analogues in various cell types in vitro, including MCF-7 breast cancer and benign prostatic cells [34, 52].
Clusterin as an inhibitor of apoptosis
Unraveling the function of clusterin has been an elusive goal, as it has been ascribed many, and sometimes contradictory, functions. Part of this ambiguity results from existence of two functionally divergent isoforms. The secreted glycosylated form (sCLU) is a highly conserved disulfide-linked heterodimeric sulfated glycoprotein of 76–80 kDa comprised of a 40 and 60 kDa α and ß subunits derived by translation from the first AUG codon of the full length CLU mRNA [53]. The other unglycosylated isoform is a ~55 kDa protein that is reported to be translocated from the cytoplasm to the nucleus (nCLU) following certain cytotoxic events to induce apoptosis. This shorter nCLU may be synthesized from a second in-frame AUG codon and does not undergo α or ß cleavage or extensive glycosylation. nCLU interacts with Ku-70, and can act as a cell death signal in MCF-7 breast cancer cells transfected with various GFP-tagged clusterin constructs [46].
Many recent studies provide strong evidence for an anti-apoptotic function for sCLU. Because clusterin binds to a wide variety of biological ligands [53, 54, 55], and is regulated by transcription factor HSF1 [48], an emerging view suggests that clusterin functions like a heat shock protein to chaperone and stabilize conformations of proteins at times of cell stress. Indeed, sCLU is the most potent inhibitor of protein precipitation, and may function to help stressed cells cope with an increased load of unfolded proteins. While accumulating data identify mature sCLU as an inhibitor of apoptosis, precise site(s) of action and binding proteins remain undefined.
The seemingly paradoxical roles for clusterin in apoptosis are perhaps analogous to those ascribed to two forms of Bcl-x that arise from alternative splicing [56, 57, 58]. The smaller form, Bcl-xS, can act to inhibit the protective effects of the larger form Bcl-xL as well as Bcl-2 through an unknown mechanism. The mature sCLU has a cytoprotective function [59, 60], while under certain conditions proapoptotic signals may induce intracellular forms through differential translation [46]. The various CLU isoforms may also arise from post-translational modifications of a single mRNA transcript [61]. Using a panel of antibodies directed against various α- and β-chain epitopes of clusterin, Lakins et al. [62] were able to immunologically distinguish the forms of clusterin upregulated in dying cells from those synthesized by surviving cells in regressing rat prostate. The secreted mature and core proproteins are believed to interact with glycoprotein 330, a cell surface receptor [63]. Collectively, these reports suggest that the pro- and anti-apoptotic functions of clusterin may be due to the activity of different isoforms that arise through either alternative splicing or post-translational modification of the mRNA transcript.
Clusterin as a therapeutic target in prostate cancer
In prostate cancer, experimental and clinical studies support the hypothesis that clusterin expression is associated with AI progression and has a protective role against apoptotic cell death. For example, the introduction of sCLU cDNA into LNCaP prostate cancer cells increases resistance to apoptosis induced by tumor necrosis factor (TNF) α treatment [64] and oxidative stress [65]. Increased expression of clusterin in prostate cancer is closely correlated with higher Gleason score [31] and cancer prognosis [66]. Residual foci of cancer cells from radical prostatectomy specimens treated with neoadjuvant androgen ablation stain strongly positive for clusterin [67]. Clusterin staining in specimens from neoadjuvantly-treated patients increased in intensity (+3–+4) in 80–90% of cancer cells compared to absent (0) to low intensity staining (+1–+2) in 10–20% of cancer cells in non-NHT treated specimens (Fig. 2). Clusterin levels also increase in prostate and other cancer cells after chemotherapy and radiation [49, 50, 68, 69, 70].
Clusterin ASO treatment enhanced castration-induced apoptosis and delayed androgen independence in the murine Shionogi system, a model mimicking human prostate cancer biology. Male mice bearing Shionogi tumors were castrated and randomly selected for treatment with antisense clusterin versus mismatch control ASO. Northern analysis (insert) shows reduced clusterin mRNA levels from tumors harvested on day 3 after castration plus ASO treatment. B Clusterin ASO treatment enhanced paclitaxel-induced apoptosis and delayed the progression of androgen independent human PC-3 prostate tumors. Mean tumor volume in PC3 tumor-bearing mice treated with daily doses of clusterin ASO plus paclitaxel or control ASO plus paclitaxel at 0.5 mg paclitaxel from days 10–14 and days 24–28, respectively
Clusterin overexpression confers a resistant phenotype
To investigate the functional significance of clusterin upregulation after treatments such as androgen withdrawal or chemotherapy, androgen sensitive human prostate cancer LNCaP were stably overexpressed with the sCLU cDNA expression vector and effects on time to AI progression after androgen ablation and chemosensitivity were evaluated. After castration in sCLU overexpressing LNCaP tumors, both tumor volume and serum PSA levels increased fourfold faster compared to control tumors [7]. Furthermore, overexpressing clusterin LNCaP tumors were more resistant to paclitaxel than control tumors [60]. These findings demonstrate that clusterin is a cell survival gene upregulated by apoptotic triggers (like androgen withdrawal, chemotherapy, radiation) and confers resistance when overexpressed.
Antisense oligonucleotide strategies to target relevant genes
Targeted therapies that have been approved for use in the clinical setting typically involve the use of small molecule inhibitors or antibodies. Unfortunately, many potential therapeutic targets are not amenable to such tactics, and therefore strategies to inhibit these targets at the gene expression level are an attractive concept. Antisense oligonucleotide (ASO) therapy is one such strategy to specifically target functionally relevant genes. ASOs are chemically modified stretches of single-strand DNA complementary to mRNA regions of a target gene that inhibit translation by forming RNA/DNA duplexes, thereby reducing mRNA and protein levels of the target gene [71]. The specificity and efficacy of an ASO relies on the precise targeting afforded by strand hybridization, where only a perfect match between the target mRNA sequence and the ASO will lead to hybridization and inhibition of translation.
Phosphorothioate ASOs are water soluble, stable agents resistant to nuclease digestion through substitution of a non-bridging phosphoryl oxygen of DNA with sulfur [72, 73]. ASOs targeting multiple different oncogenes have been reported to specifically inhibit the expression of these genes and delay progression in several tumor types, and clinical trials are underway for several of these compounds. In clinical trials, continuous or frequent intravenous infusions are required to administer first generation phosphorothioate ASOs because of their short tissue lives, which remains a major technical limitation. Therefore, effort has been made to improve the stability and efficacy of ASO by modifications of the phophodiester-linkage, the heterocycle, or the sugar. One such alteration is the 2′-O-(2-methoxy) ethyl (2′-MOE) modification to the 2′-position of the carbohydrate moiety. 2′MOE ASOs form duplexes with RNA with a significantly higher affinity relative to unmodified phosphorothioate ASOs. This increased affinity has been shown to result in improved antisense potency in vitro and in vivo. In addition, 2′MOE ASOs display significantly improved resistance against nuclease-mediated metabolism relative to first generation phosphorothioate ASOs. This property results in an improved tissue half-life in vivo, which produces a longer duration of action and allows for a more relaxed dosing regimen [74]. Finally, 2′MOE ASOs have been reported to display a more attractive safety profile relative to unmodified phosphorothioate ASOs [75]. Taken together, 2′MOE ASOs have the potential to be given as short infusions on a weekly schedule, yet have the same or greater activity as prolonged infusions of unmodified phosphorothioate ASO.
Using clusterin ASOs to enhance hormone sensitivity
Targeting cell survival genes upregulated by androgen withdrawal may enhance castration-induced apoptosis and thereby prolong time to overt recurrence. Murine and human ASOs corresponding to the clusterin translation initiation site reduced clusterin levels in a dose-dependent and sequence-specific manner [7, 76]. AD Shionogi tumors regressed faster and complete regression occurred earlier after castration in mice treated with clusterin ASO compared to controls. Clusterin ASO treatment significantly delayed the recurrence of AI tumors; tumor volume in the mismatch-treated control group was six times greater than the ASO-treated group by day 50 post-castration [8].
Enhancing chemo-sensitivity using clusterin ASOs
Clusterin ASOs also increased the cytotoxic effects of mitoxanthrone and paclitaxel, reducing the IC50 of PC3 and Shionogi cells by 75%–90% [49, 76]. The induction of apoptosis by 10 nM taxol, as demonstrated by DNA laddering and PARP cleavage, could only be seen when used with clusterin ASOs. Although clusterin ASO’s had no effect on the growth of established AI Shionogi or PC3 tumors, clusterin ASOs synergistically enhanced paclitaxel-induced tumor regression in both the Shionogi and human PC3 models [49, 76].
Clusterin may also play a role in mediating chemoresistance in renal cell carcinoma and other tumors. We recently reported that inhibition of clusterin levels chemosensitized various cancers including renal cell carcinoma [69], urothelial [68], lung [70], and osteosarcoma [77]. For example, pretreatment of Caki-2 cells with clusterin ASOs decreased clusterin levels and significantly enhanced chemosensitivity to paclitaxel in vitro. In vivo administration of clusterin ASO synergistically enhanced paclitaxel-induced Caki-2 tumor regression and delayed tumor progression by 50%. Similarly, clusterin siRNA enhanced the effects of cytotoxic chemotherapy in human prostate PC3 and osteosarcoma cell lines [77] (Table 1).
Enhancing radiation-sensitivity using clusterin ASOs
Little is known about the molecular mechanisms that contribute to the intrinsic radioresistance characteristic of prostate cancer. Bcl-2 overexpressing LNCaP cells appear to be more resistant to radiation-induced apoptosis and tumorigenesis compared to parental cells (78). Similarly, clusterin-overexpressing LNCaP cells were less sensitive to irradiation with significantly lower cell-death rates (23% after 8 Gy) compared to parental LNCaP cells (50% after 8 Gy) 3 days after irradiation [50, 79]. Clusterin expression in PC-3 cells after radiation increased in a dose-dependent manner in vitro by 70% up to 12 Gy and in vivo by >80%. Inhibition of clusterin expression in PC-3 cells using clusterin ASOs before radiation significantly decreased PC-3 cell growth rate and plating efficiency, and enhanced radiation-induced apoptosis. In vivo administration of clusterin ASO before and after radiation significantly reduced PC-3 tumor volume by 50% at 9 weeks as compared to mismatch control oligonucleotides. These findings support the hypothesis that clusterin acts as a cell survival protein that mediates radioresistance through the inhibition of apoptosis.
Human trials with OGX-011
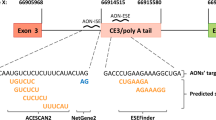
To identify the most potent ASO sequence to move into human trials, the clusterin gene was walked with a series of 80 ASO sequences. This gene walk identified a 21mer targeting the AUG translational initiation site, the sequence used in all preclinical human xenografts, as the most potent ASO sequence. This 21mer ASO was incorporated into MOE-gapmer backbone and synthesized for human trials as OGX-011 under a codevelopment relationship between OncoGenex technologies (Vancouver, BC, Canada) and Isis Pharmaceuticals (Carlsbad, Calif, USA).
A phase I trial, NCIC IND.153, was recently completed with a 2′MOE ASO targeted to clusterin mRNA using OGX-011. This trial had a unique design in that patients with localized prostate cancer were administered the 2′MOE ASO prior to radical prostatectomy, and thus a pharmacodynamic endpoint (i.e. inhibition of clusterin expression) could be evaluated for each patient and dose level [80]. The OGX-011 was given as a 2-hour intravenous infusion over 2 h on days 1, 3, 5, 8, 15, 22 and 29 with radical prostatectomy carried out within 7 days of the last dose. Relevant concentrations of OGX-011 could be achieved that inhibited expression of clusterin in human cancer tissue in a dose dependent fashion, a notable first in the literature. Concentrations of OGX-011 associated with preclinical effect could be achieved in tumor tissue and a biologically effective dose of 640 mg based on clusterin target suppression by up to 90% was identified. Furthermore, a well tolerated phase II dose was established based on biologic effectiveness, rather than the traditional phase I endpoint of maximum tolerated dose which may not be relevant for targeted therapeutics. Side effects included fever and chills in the first week of infusions, and transient myelosuppression and elevations of liver enzyme tests that normalized despite continued therapy. This phase I trial demonstrates that OGX-011 is well tolerated and inhibits clusterin expression in prostate cancers. The phase II dose for OGX-011 is 640 mg based on pharmacokinetic and target regulation parameters. Phase II studies of OGX-011 in combination with hormone and chemotherapy are planned in patients with prostate, breast and lung cancers (Table 2).
Summary.
The data reviewed above identify clusterin as an anti-apoptosis protein upregulated in an adaptive cell survival manner by androgen ablation and chemotherapy that confers resistance to various cell death triggers, including hormone-, radiation-, and chemotherapy. Inhibition of clusterin upregulation using clusterin ASOs can enhance cell death following treatment with androgen ablation and chemotherapy. Clinical trials using ASOs confirm potent suppression of clusterin levels and phase II studies of OGX-011 in combination with docetaxel will begin in early 2005.
References
Denis L, Murphy GP (1993) Overview of phase III trials on combined androgen treatment in patients with metastatic prostate cancer. Cancer 72:3888–3895
Oh WK, Kantoff PW (1998) Management of hormone refractory prostate cancer: current standards and future prospects. J Urol 160:1220–1229
Tannock IF, De Wit R, Berry WR et al. for the TAX 327 Investigators (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351:1502–1512
Petrylak DP, Tangen CM, Hussain MH et al. (2004) Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med 351:1513–1520
Isaacs JT, Wake N, Coffey DS, Sandberg AA (1982) Genetic instability coupled to clonal selection as a mechanism for progression in prostatic cancer. Cancer Res 42–48:2353
Miyake H, Tolcher A, Gleave ME (1999) Antisense Bcl-2 oligodeoxynucleotides delay progression to androgen-independence after castration in the androgen dependent Shionogi tumor model. Cancer Res 59:4030–4034
Miyake H, Rennie P, Nelson C, Gleave ME (2000) Testosterone-repressed prostate message-2 (TRPM-2) is an antiapoptotic gene that confers resistance to androgen ablation in prostate cancer xenograft models. Cancer Res 60:170–176
Bruchovsky N, Rennie PS, Coldman AJ, Goldenberg SL, To M, Lawson D (1990) Effects of androgen withdrawal on the stem cell composition of the Shionogi carcinoma. Cancer Res 50:2275–2282
Miyake H, Nelson C, Rennie P, Gleave ME (2000) Overexpression of insulin-like growth factor binding protein-5 helps accelerate progression to androgen-independence in the human prostate LNCaP tumor model through activation of phosphatidylinositol 3′-kinase pathway. Endocrinology 141:2257–2265
Kiyama S, Morrison K, Zellweger T, Akbari M, Cox ME, Yu D, Miyake H, Gleave ME (2003) Castration-induced increased in insulin-like growth factor-binding protein 2 promotes proliferation of androgen-independent human prostate LNCaP tumors. Cancer Res 63:3575–3584
Sato N, Sadar MD, Bruchovsky N, Saatcioglu F, Rennie PS, Sato S, Lange PH, Gleave ME (1997) Androgenic induction of prostate-specific antigen gene is repressed by protein-protein interaction between androgen receptor and AP-1c-Jun in the human prostate cancer cell line LNCaP. J Biol Chem 272:17485–17494
Craft N, Shostak Y, Carey M, Sawyers C (1999) A mechanism for hormone-independent prostate cancer through modulation of androgen receptor signaling by the HER-2/neu tyrosine kinase. Nat Med 5:280–285
Sherwood ER, Van Dongen JL, Wood CG, Liao S, Kozlowski JM, Lee C (1998) Epidermal growth factor receptor activation in androgen-independent but not androgen-stimulated growth of human prostatic carcinoma cells. Br J Cancer 77:855–861
Abreu-Martin MT, Chari A, Palladino AA, Craft NA, Sawyers CL (1999) Mitogen-activated protein kinase 1 activates androgen receptor-dependent transcription and apoptosis in prostate cancer. Mol Cell Biol 19:5143–5154
Chen CD, Welsbie DS, Tran C, Baek SH, Chen R, Vessella R, Rosenfeld MG, Sawyers CL (2004) Molecular determinants of resistance to antiandrogen therapy. Nat Med 10:33–39
Ettinger SL, Sobel R, Whitmore T, Akbari M, Bradley D, Gleave M, Nelson C (2004) Dysregulation of sterol response element binding proteins and downstream effectors in prostate cancer during progression to androgen-independence. Cancer Res 64:2212–21
Gimenez-Bonafe, P, Fedoruk MN, WhitmoreTG, Akbari M, Ralph JL, Ettinger S, Gleave ME, Nelson CC (2004) Up-regulation of the transcription factor YB-1 and its correlation with P-glycoprotein expression during prostate cancer tumor progression. Prostate 59:337–349
Gleave ME, Tolcher A, Miyake H, Beraldi E, Goldie J (1999) Progression to androgen-independence is delayed by antisense bcl-2 oligodeoxynucleotides after castration in the LNCaP prostate tumor model. Clin Cancer Res 5:2891–2898
Paterson R, Gleave M, Jone E, Zubovits J, Goldenberg SL, Sullivan LD (1999) Immunohistochemical analysis of radical prostatectomy specimens after 8 months of neoadjuvant hormone therapy. Mol Urol 3:277–286
McDonnell TJ, Troncoso P, Brisby SM, Logothetis CL, Chung LWK, Hsieh JT et al. (1992) Expression of the protooncogene Bcl-2 in the prostate and its association with emergence of androgen-independent prostate cancer. Cancer Res 52:6940–6944
Colombel M, Symmans F, Gil S, O’Toole KM, Choplin D, Benson M et al. (1993) Detection of the apoptosis-suppressing oncoprotein Bcl-2 in hormone-refractory human prostate cancers. Am J Pathol 143:390–400
Raffo AJ, Periman H, Chen MW, Streitman JS, Buttyan R (1995) Overexpression of bcl-2 protects prostate cancer cells from apoptosis in vitro and confers resistance to androgen depletion in vivo. Cancer Res 55:4438–4445
Jansen B, Schlagbauer-Wadl H, Brown BD, Bryan RN, Van Elsas A, Muller M et al. (1998) bcl-2 antisense therapy chemosensitizes human melanoma in SCID mice. Nat Med 4:232–234
Miyake H, Tolcher A, Gleave ME (2000) Antisense bcl-2 oligodeoxynucleotides enhance taxol chemosensitivity and synergistically delays progression to androgen-independence after castration in the androgen dependent Shionogi tumor model. J Natl Cancer Inst 92:34–41
Rocchi P, So A, Kojima S. Beraldi E, Fazli L, Gleave ME (2004) Heat shock protein 27 increases after androgen ablation and plays a cytoprotective role in hormone refractory prostate cancer. Cancer Res 64:6595–6602
Nickerson T, Miyake H, Gleave ME, Pollak M (1999) Castration-induced apoptosis of androgen-dependent Shionogi carcinoma is associated with increased expression of genes encoding insulin-like growth factor binding proteins. Cancer Res 59:3392–3395
Miyake H, Pollak, Gleave ME (2000) Castration-induced up-regulation of insulin-like growth factor binding protein-5 potentiates insulin-like growth factor-I activity and accelerates progression to androgen independence in prostate cancer models. Cancer Res 60:3058–3064
Tenniswood M, Wang Z, Lakins J, Morrissey C, O’Sullivan J, Tang H (1998) Clusterin in the male reproductive tract. J Androl 19:508–516
Calero M, Rostagno A, Matsubara E, Zlokovic B, Frangione B, Ghiso J (2000) Apolipoprotein J (clusterin) and Alzheimer’s disease. Microsc Res Tech 50:305–315
Rosenberg ME, Silkensen J (1995) Clusterin and the kidney. Exp Nephrol 3: 9–14
Steinberg J, Oyasu R, Lang S, Sintich S, Rademaker A, Lee C, Kozlowski JM, Sensibar JA (1997) Intracellular levels of SGP-2 (clusterin) correlate with tumor grade in prostate cancer. Clin Cancer Res 3:1701–1711
Cervellera M, Raschella G, Santilli G, Tanno B, Ventura A, Mancini C, Sevignani C, Calabretta B, Sala A (2000) Direct transactivation of the anti-apoptotic gene apolipoprotein J (clusterin) by B-MYB. J Biol Chem 275:21055–21060
Kyprianou N, English HF, Davidson NE, Isaacs JT (1991) Programmed cell death during regression of the MCF-7 human breast cancer following estrogen ablation. Cancer Res 51:162–166
Redondo M, Villar E, Torres-Munoz J, Tellez T, Morell M, Petito CK (2000) Overexpression of clusterin in human breast carcinoma. Am J Pathol 157:393–399
Wellmann A, Thieblemont C, Pittaluga S, Sakai A, Jaffe ES, Siebert P, Raffeld M (2000) Detection of differentially expressed genes in lymphomas using cDNA arrays: identification of clusterin as a new diagnostic marker for anaplastic large-cell lymphomas. Blood 96:398–404
Parczyk K, Pilarsky C, Rachel U, Koch-Brandt C (1994) Gp80 (clusterin; TRPM-2) mRNA level is enhanced in human renal clear cell carcinomas. J Cancer Res Clin Oncol 120:186–188
Montpetit ML, Lawless KR, Tenniswood M (1986) Androgen-repressed messages in the rat ventral prostate. Prostate 8:25–36
Budendorf L, Kolmer M, Kononen J et al. (1999) Hormone therapy failure in human prostate cancer: analysis by complementary DNA and tissue arrays. J Natl Cancer Inst 91:1758–1764
Kyprianou N, English HF, Isaacs JT (1990) Programmed cell death during regression of PC-82 human prostate cancer following androgen ablation. Cancer Res 50:3748–3753
Tenniswood MP, Guenette RS, Lakins J, Mooibroek M, Wong P, Welsh JE (1992) Active cell death in hormone-dependent tissues. Cancer Metastasis Rev 11:197–220
Danik M, Chabot JG, Mercier C, Benabid AL, Chauvin C, Quirion R, Suh M (1991) Human gliomas and epileptic foci express high levels of a mRNA related to rat testicular sulfated glycoprotein 2, a purported marker of cell death. Proc Natl Acad Sci U S A 88:8577–8581
Connor J, Buttyan R, Olsson CA, D’Agati V, O’Toole K, Sawczuk IS (1991) SGP-2 expression as a genetic marker of progressive cellular pathology in experimental hydronephrosis. Kidney Int 39:1098–1103
Ho SM, Leav I, Ghatak S, Merk F, Jagannathan VS, Mallery K (1998) Lack of association between enhanced TRPM-2/clusterin expression and increased apoptotic activity in sex-hormone-induced prostatic dysplasia of the Noble rat. Am J Pathol 153:131–139
Schwochau GB, Nath KA, Rosenberg ME (1998) Clusterin protects against oxidative stress in vitro through aggregative and nonaggregative properties. Kidney Int 53:1647–1653
French LE, Sappino AP, Tschopp J, Schifferli JA (1992) Distinct sites of production and deposition of the putative cell death marker clusterin in the human thymus. J Clin Invest 90:1919–1925
Yang CR, Leskov K, Hosley-Eberlein K, Criswell T, Pink JJ, Kinsella TJ, Boothman DA (2000) Nuclear clusterin/XIP8, an x-ray-induced Ku70-binding protein that signals cell death. Proc Natl Acad Sci U S A 97:5907–5912
Koch-Brandt C, Morgans C (1996) Clusterin: a role in cell survival in the face of apoptosis? Prog Mol Subcell Biol 16:130–149
Michel D, Chatelain G, North S, Brun G (1997) Stress-induced transcription of the clusterin/apoJ gene. Biochem J 328:45–50
Miyake H, Rennie P, Nelson C, Gleave ME (2000) Acquisition of chemoresistant phenotype by overexpression of the antiapoptotic gene, testosterone-repressed prostate message-2 (TRPM-2), in prostate cancer xenograft models. Cancer Res 60:2547–2554
Zellweger T, Chi K, Miyake H, Adomat H, KiyamaS, Skov K, Gleave M (2002) Enhanced radiation sensitivity in prostate cancer by inhibition of the cell survival protein clusterin. Clin Cancer Res 8:3276–3284
Criswell T, Klokov D, Beman M, Lavik JP, Boothman DA (2003) Repression of IR-inducible clusterin expression by the p53 tumour suppression protein. Cancer Biol Ther 2:372–380
Crescioli C, Ferruzzi P, Caporali A, Scaltriti M, Bettuzzi S, Mancina R, Gelmini S, Serio M, Villari D, Vannelli GB, Colli E, Adorini L, Maggi M (2004) Inhibition of prostate cell growth by BXL-628, a calcitriol analogue selected for a phase II clinical trial in patients with benign prostate hyperplasia. Eur J Endocrinol 150: 591–603
Jones SE, Jomary C (2002) Clusterin. IntJBiochem Cell Biol 34:427–431
Wilson MR, Easterbrook-Smith SB (2000) Clusterin is a secreted mammalian chaperone. Trends Biochem Sci 25:95–98
Humphreys DT, Carver JA, Easterbrook-Smith SB, Wilson MR (1999) Clusterin has chaperone-like activity similar to that of small heat shock proteins. J Biol Chem 274:6875–6881
Boise LH, Gonzalez-Garcia M, Postema CE, Ding L, Lindsten T, Turka LA, Mao X, Nunez G, Thompson CB (1993) bcl-x, a bcl-2-related gene that functions as a dominant regulator of apoptotic cell death. Cell 74:597–608
Rouayrenc JF, Boise LH, Thompson CB, Privat A, Patey G (1995) Presence of the long and the short forms of Bcl-X in several human and murine tissues. C R Acad Sci III 318:537–540
Minn AJ, Boise LH, Thompson CB (1996) Bcl-x(S) anatagonizes the protective effects of Bcl-x(L). J Biol Chem 271:6306–6312
Sintich SM, Steinberg J, Kozlowski JM, Lee C, Pruden S, Sayeed S, Sensibar JA (1999) Cytotoxic sensitivity to tumor necrosis factor alpha in PC3 and LNCaP prostatic cancer cells is regulated by extracellular levels of SGP-2 (clusterin). Prostate 39:87–93
Miyake H, Hara I, Kamidono S, Gleave ME, Eto H (2003) Resistance to cytotoxic chemotherapy-induced apoptosis in human prostate cancer cells is associated with intracellular clusterin expression. Oncol Rep 10:469–473
Wong P, Pineault J, Lakins J, Taillefer D, Leger J, Wang C, Tenniswood M (1993) Genomic organization and expression of the rat TRPM-2 (clusterin) gene, a gene implicated in apoptosis. J Biol Chem 268:5021–5031
Lakins J, Bennett SA, Chen JH, Arnold JM, Morrissey C, Wong P, O’Sullivan J, Tenniswood M (1998) Clusterin biogenesis is altered during apoptosis in the regressing rat ventral prostate. J Biol Chem 273:27887–27895
Kounnas MZ, Loukinova EB, Stefansson S, Harmony JA, Brewer BH, Strickland DK, Argraves WS (1995) Identification of glycoprotein 330 as an endocytic receptor for apolipoprotein J/clusterin. J Biol Chem 270:13070–13075
Sensibar JA, Sutkowski DM, Raffo A et al. (1995) Prevention of cell death induced by tumor necrosis factor in alpha LNCaP cells by overexpression of sulfated glycoprotein-2 (clusterin). Cancer Res 55:2431–2437
Miyake H, Hara I, Gleave ME, Eto H (2004) Protection of androgen-dependent human prostate cancer cells from oxidative stress-induced DNA damage by overexpression of clusterin and its modulation by androgen. Prostate 61: 318–323
Pins MR, Fiadjoe JE, Korley F, Wong M, Rademaker AW, Jovanovic B, Yoo TK, Kozlowski JM, Raji A, Yang XJ, Lee C (2004) Clusterin as a possible predictor for biochemical recurrence of prostate cancer following radical prostatectomy with intermediate Gleason scores: a preliminary report. Prostate Cancer Prostatic Dis 7:243–248
July L, Akbari M, Zellweger T, Jones EC, Goldenberg SL, Gleave ME (2002) Clusterin expression is significantly enhanced in prostate cancer cells following androgen withdrawal therapy. Prostate 50:179–188
Miyake H, Hara I, Kamidono S, Gleave ME (2001) Synergistic chemosensitization and inhibition of tumour growth and metastasis by the antisense oligodeoxynucleotide targeting clusterin gene in a human bladder cancer model. Clin Cancer Res 7:4245–4252
Zellweger T, Miyake H, July L, Akbari M, Kiyama S, Gleave ME (2001) Chemosensitization of a human renal cell cancer model by antisense TRPM-2 oligodeoxynucleotides both in vitro and in vivo. Neoplasia 3:1–8
July LV, Beraldi E, So AI, Evans K, English J, Fazli L, Gleave ME (2004) Nucleotide-based therapies targeting clusterin chemosensitizes human lung adenocarcinoma cells both in vitro and in vivo. Mol Cancer Ther 3:223–232
Crooke ST (1993) Therapeutic applications of oligonucleotides. Annu Rev Pharmacol Toxicol 32:329–376
Saijo Y, Perlaky L, Wang H, Busch H (1994) Pharmacokinetics, tissue distribution, and stability of antisense oligodeoxynucleotide phosphorothioate ISIS 3466 in mice. Oncol Res 6:243–249
Monia BP, Johnston JF, Geiger T, Muller M, Fabbro D (1996) Antitumor activity of a phosphorothioate antisense oligodeoxynucleotide targeted against C-raf kinase. Nat Med 2:668–675
Zellweger T, Miyake H, Cooper S, Chi K, Conklin BS, Monia B, Gleave ME (2001) Antitumor activity of antisense clusterin oligonucleotides is improved in vitro and in vivo by incorporation of 2′-o-(2-methoxy) ethyl chemistry. J Pharmacol Exp Ther 298:934–940
Henry S, Stecker K, Brooks D, Monteith D, Conklin B, Bennett CF (2000) Chemically modified oligonucleotides exhibit decreased immune stimulation in mice. J Pharmacol Exp Ther 292:468–479
Miyake H, Chi K, Gleave ME (2000) Antisense TRPM-2 oligodeoxynucleotides chemosensitize human androgen-independent PC-3 prostate cancer cells both in vitro and in vivo. Clin Cancer Res 6:1655–1663
Trougakso IP, So A, Jansen B, Gleave ME, Gonos ES (2004) Silencing expression of the clusterin/apolipoprotein J gene in human cancer cells using small interfering RNA induces spontaneous apoptosis reduced growth ability, and cell sensitization to genotoxic and oxidative stress. Cancer Res 64:1834–1842
Kyprianou N, King ED, Bradbury D, Rhee JG (1997) Bcl-2 overexpression delays radiation-induced apoptosis without affecting the clonogenic survival of human prostate cancer cells. Int J Cancer 70:341–348
Zellweger T, Kiyama S, Chi K, Miyake H, Adomat H, Skov K, Gleave ME (2003) Overexpression of the cytoprotective protein clusterin decreases radiosensitivity in the human LNCaP prostate tumour model. BJU Int 92:463–469
Chi KN, Eisenhauer E, Fazli L, Jones EC, Powers J, Ayers D, Goldenberg SL, Gleave ME (2004) A phase I pharmacokinetic (PK) and pharmacodynamic (PD) study of OGX-011, a 2′methoxyethyl phosphorothioate antisense to clusterin, in patients with prostate cancer prior to radical prostatectomy. J Clin Ocol, Proceedings of American Society of Clinical Oncology, 2004
Hoeller C, Pratscher B, Thallinger C, Winter D, Fink D, Kovacic B, Sexl V, Wacheck V, Gleave ME, Pehamberger H, Jansen B (2005) Clusterin regulates drug-resistance in melanoma cells.J Invest Dermatol (in press)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gleave, M., Miyake, H. Use of antisense oligonucleotides targeting the cytoprotective gene, clusterin, to enhance androgen- and chemo-sensitivity in prostate cancer. World J Urol 23, 38–46 (2005). https://doi.org/10.1007/s00345-004-0474-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-004-0474-0