Abstract
Objectives
To investigate outcomes and retrospectively evaluate characteristics of additional lesions initially assessed as BI-RADS category 3, 4, and 5 at preoperative MRI to determine appropriate follow-up management.
Methods
We retrospectively reviewed 429 lesions other than primary cancer initially assessed as BI-RADS category 3, 4, and 5 at preoperative MRI in 391 patients with breast cancer from March 2012 to December 2013. We investigated their malignancy rate and outcome according to BI-RADS category assessments. We also analyzed clinical and imaging characteristics of each lesion. Pathological results and imaging follow-up of at least 2 years were used as reference standards.
Results
Of 429 lesions in 391 patients (mean 48.1 years ± 9.4), the malignancy rate of BI-RADS 3, 4, and 5 lesions was 1.4% (3/213), 17.8% (38/214), and 50% (1/2), respectively. Of BI-RADS 3 lesions or BI-RADS 4 or 5 lesions that were followed up after benign-concordant biopsy (n = 114), two contralateral masses (2/306, 0.7%) were diagnosed as malignancy at 13.3 and 33.2 months after initial detection, within a median follow-up of 63.3 months. None of the NME or foci or lesions followed up after benign-concordant biopsy had a delayed diagnosis of malignancy. Of the 391 patients, 97.4% (381/391) received at least one type of adjuvant therapy.
Conclusion
The incidence of delayed cancer diagnosis among additionally detected lesions other than primary cancer is very low and short-term follow-up is unnecessary. Contralateral masses which were not confirmed by biopsy may need annual follow-up.
Key Points
• 1.4% (3/213) of BI-RADS 3 lesions were malignant including 2 delayed diagnoses after 13.2 months and 33.2 months, and 17.8% (38/214) of BI-RADS 4 lesions and 50% (1/2) of BI-RADS 5 lesions were malignant.
• The incidence of delayed diagnosis from additional MRI-detected lesions was very low (0.7%, 2/306) during follow-up, which were all T1N0 contralateral cancer.
• Annual follow-up might be adequate for preoperative MRI-detected BI-RADS 3 lesions and BI-RADS 4 lesions followed up after benign-concordant biopsy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast magnetic resonance imaging (MRI) has consistently been the most sensitive modality for depicting breast cancer and has been widely used for preoperative planning in breast cancer patients [1, 2]. In a range of 1.6–17% of patients, additional malignant lesions are found at preoperative MRI which had been occult on initial mammography and ultrasound (US) [3,4,5]. Although breast MRI has shown acceptable specificity compared with other imaging modalities, approximately one out of three additionally detected lesions will result in false-positive findings, suggesting the need for additional preoperative interventions such as biopsy [6,7,8,9,10,11,12,13]. Furthermore, BI-RADS 3 lesions are frequently encountered at preoperative MRI, which may require short-term follow-up [14, 15].
Whereas large-scale studies have suggested that annual follow-up might be sufficient in US-detected BI-RADS 3 lesions or US lesions considered to be concordant benign after biopsy [16, 17], there is limited data for lesions detected at preoperative MRI. For BI-RADS 3 lesions identified at MRI, the assessment of which remains intuitive for inexperienced radiologists [18], initial short-term and further follow-up is recommended at 6, 12, and 24 months as is for BI-RADS 3 lesions identified at mammography or US [18, 19]. However, the appropriate follow-up interval for additional lesions detected at preoperative MRI is still controversial. Although patients with newly diagnosed breast cancer have an elevated lifetime risk of malignancy, follow-up management approaches may differ from other high-risk screening populations as most of these patients receive adjuvant therapy including antihormonal therapy, chemotherapy, and radiation therapy [20, 21]. In addition, although MR imaging features associated with malignancy are well established, there is relatively limited data regarding additional lesions detected on preoperative MRI [22,23,24].
Therefore, the purpose of this study was to investigate outcomes and retrospectively evaluate characteristics of additional lesions initially assessed as BI-RADS category 3, 4, and 5 at preoperative MRI to determine appropriate follow-up management.
Materials and methods
Study population
Our institutional review board approved this retrospective study, and the requirement for informed consent was waived. Between March 2012 and December 2013, 1252 consecutive breast MR examinations were performed for preoperative evaluation in patients with newly diagnosed breast cancer. We reviewed the reports of each MR examination and found a total of 725 lesions, other than the primary cancer, in 658 patients which had been initially assigned to BI-RADS category 3, 4, or 5. In patients with more than one assessment in a single breast, we included the first lesion noted in the impression section of the radiology report or located at a different quadrant from the proven malignancy. Specific exclusion criteria are presented in Fig. 1 and Appendix E1 (online). Finally, a total of 429 lesions additionally detected at preoperative MRI in 391 breast cancer patients (mean age 48.1 years, range 25–78 years) were included in our study, which consisted of 174 (40.6%) initial BI-RADS 3 lesions, 253 (59.0%) initial BI-RADS 4 lesions, and 2 (0.5%) initial BI-RADS 5 lesions, based on the initial BI-RADS category assessment assigned at the time of MRI interpretation. Among them, 39 lesions initially classified as BI-RADS 4 were later downgraded to BI-RADS 3 prior to surgery, after re-review of MRI and targeted US features. Therefore, the final BI-RADS categories of our study population were 213 BI-RADS 3 lesions, 214 BI-RADS 4 lesions, and 2 BI-RADS 5 lesions (Fig. 1). Clinical information about family history, BRCA mutation, and adjuvant treatment are shown in Table 1.
MRI interpretation and initial management
The MRI technique is described in Appendix E2. MRI was initially prospectively interpreted by one of four faculty radiologists with 7–12 years of experience in breast MRI. A computer-aided diagnosis (CAD) program (CADstream version 5.2; Merge Healthcare, Inc.) was available for breast interpretation and was freely used at the discretion of the interpreting radiologist. Although no formal criteria existed during the study period regarding which lesion types should be assigned BI-RADS 3, category 3 was commonly assigned to isolated or prominent foci among multiple bilateral foci without washout, masses without suspicious MRI features, or focal/regional nonmass enhancement (NME) with internal homogeneous enhancement. Targeted US was not routinely performed for BI-RADS 3 lesions, but biopsy or excision was occasionally performed at the request of the physician. Lesions with suspicious MRI features were assessed as BI-RADS 4 or 5. When any suspicious findings were newly identified at preoperative MRI examinations, targeted US was performed for further evaluation and to decide the guidance modality for biopsy. US-guided biopsy, surgical excision under US-guided needle localization, or MR-guided biopsy was recommended at the discretion of the radiologist who performed the targeted US. In addition, all preoperative cases were reviewed at a weekly conference between radiologists and surgeons, for which a faculty breast radiologist re-reviewed MRI and targeted US features and recommended imaging follow-up if lesions were reassessed as BI-RADS 3.
All MRI examinations were later retrospectively re-analyzed by two breast imaging dedicated radiologists (V.Y.P and J.H.L). Each radiologist independently reviewed the MRI examinations and evaluated each lesion in terms of lesion type including foci, mass (shape, margin, and internal enhancement), NME (distribution and internal enhancement), and T2 signal intensity according to the BI-RADS lexicon. Discordant findings were reviewed again in consensus. Each lesion was re-analyzed using two CAD programs (CADstream version 5.2; Merge Healthcare, Inc. and Myrian®; Intrasense) to obtain kinetic features for initial (slow, medium, fast) and delayed phases (persistent, plateau, washout).
Follow-up protocol
Follow-up was recommended for lesions considered imaging pathology–concordant after image-guided biopsy or BI-RADS 3 lesions identified at preoperative MRI. If a lesion had been initially classified as BI-RADS 4 but was downgraded to BI-RADS 3 after re-review of imaging features prior to surgery, imaging follow-up was also recommended. When the lesion was determined to have a mammographic or US correlate, follow-up was performed with mammography or US. If the lesion was stable for 2 years, it was downgraded to BI-RADS 2. During the study period, patients routinely underwent breast imaging follow-up with breast US every 6 months and with mammography every 12 months for 5 years following definitive breast cancer surgery. Short-term MRI follow-up was performed in lesions requiring MR imaging evaluation or at the request of the clinician or patient. Since 2013, breast MRI has been increasingly implemented in the routine post-treatment surveillance protocol at our institution, and patients undergo surveillance breast MRI imaging instead of US at approximately 2 and 5 years after surgery.
Data and statistical analysis
We collected clinical data on family history of breast cancer, type of surgery, neoadjuvant chemotherapy, radiation therapy, adjuvant chemotherapy, and antihormonal therapy from electronic medical records. We reviewed all available images, histopathology results, and the interval between lesion detection and delayed cancer diagnosis. Rates of malignancy for each final BI-RADS category were calculated. A malignancy was defined as a lesion that yielded invasive carcinoma or ductal carcinoma in situ at needle biopsy or surgery. Benignity was based on histological confirmation by biopsy or surgery or imaging follow-up of at least 24 months.
Interobserver agreements for retrospective evaluation of MRI imaging features were evaluated by Cohen’s kappa statistics. A kappa statistic of 0.2 or less indicated slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–0.99, perfect agreement. Further analysis on the association between lesion characteristics and malignancy risk was done in consensus between the two radiologists, using the chi-square test or Fisher’s exact test with logistic regression analysis. Odds ratios with 95% confidence interval were estimated by univariable and multivariable logistic regression. Initial phase enhancement characteristics (fast or medium/slow), delayed phase enhancement characteristics (washout or plateau/persistent), and shape of the mass lesions (oval/round or irregular) were dichotomized for statistical analysis. Internal enhancement patterns were analyzed according to the BI-RADS lexicon. For variables that showed complete separation between benign and malignancy, we used Firth’s method to correct the biased estimation [25]. Statistical analyses were performed using the SPSS version 23 (IBM Corp.) and R (version 3.5.2; R Foundation for Statistical Computing). A p value of less than 0.05 was considered to indicate a significant difference.
Results
The malignancy rates of additionally detected BI-RADS category 3, 4, and 5 were 1.4% (3/213), 17.8% (38/214), and 50% (1/2), respectively. The malignancy rate was 12.2% (16/131) and 8.7% (26/298) for ipsilateral and contralateral lesions, respectively. The outcomes of the additional lesions are summarized according to BI-RADS category in Fig. 2. The 42 malignant lesions included 4 foci (4/154, 2.6%), 32 masses (32/218, 14.7%), and 6 NME (6/57, 10.5%). Of 387 benign lesions, 114 (29.4%) were confirmed by biopsy (US-guided core needle biopsy (CNB), n = 113; MRI-guided biopsy, n = 1), 83 (21.4%) were confirmed by surgery, and 190 (49.1%) were stable or disappeared during a median follow-up of 63.3 months (range, 24.0–81.8 months). Of the benign lesions, 83% (321/387) were followed up by MRI at least once. Of BI-RADS 3 lesions and BI-RADS 4 or 5 lesions followed up after benign-concordant biopsy, two contralateral masses (2/306, 0.7%) were diagnosed as malignancy at 13.3 and 33.2 months after initial detection, within a median follow-up of 63.3 months.
Outcome of BI-RADS category 3 lesions
Among the 213 BI-RADS 3 lesions (57 ipsilateral, 156 contralateral lesions), 192 (90.1%) underwent imaging follow-up, 10 (4.5%) underwent US-guided CNB, 4 (1.9%) were confirmed by surgery after biopsy, and 7 lesions (3.3%) directly underwent surgical excision (Fig. 1). These included thirty-nine (18.3%) nodules initially classified as BI-RADS 4 but which were downgraded to BI RADS 3 based on re-review of MRI and US features prior to surgery and underwent follow-up. In one patient with a BI-RADS 3 lesion diagnosed as an intraductal papilloma by CNB, an incidental 1-mm-size solid papillary carcinoma was found near the previous biopsy site at excision.
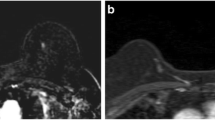
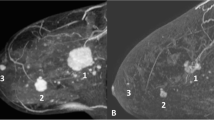
There were two (1.0%, 2/202) delayed cancer diagnosis during follow-up, occurring in patients who received antihormonal therapy and radiation therapy for the ipsilateral breast. One of them was a 10-mm contralateral mass which was diagnosed as a node-negative 12-mm invasive ductal carcinoma 13.2 months after initial detection (Fig. 3). Another was a 12-mm contralateral mass initially assessed as BI-RADS 4 but which was occult at targeted US. After re-review of MRI features, it was downgraded to BIRADS 3 based on its hyperintensity on T2-weighted images, but was confirmed as a node-negative 14-mm metaplastic carcinoma 33.2 months later.
A 63-year-old woman with a delayed diagnosis of contralateral breast cancer. a The initial preoperative T1-weighted early postcontrast subtraction axial MRI image shows a 10-mm circumscribed mass in the left upper outer breast (arrow), which was assessed as BI-RADS 3. b At a follow-up mammogram 1.1 years later, distortion was newly detected and a spiculated mass (arrow) at the left upper breast was identified. c US image shows an irregular mass (arrow) that was newly detected on the subsequent US examination. d The T1-weighted delayed postcontrast subtraction axial MR image shows the mass (arrow) with newly developed irregular shape. The mass was confirmed as a 12-mm node-negative invasive ductal carcinoma by biopsy and surgery
None of 10 lesions followed up after benign-concordant biopsy had a delayed diagnosis of cancer, within a median follow-up of 62.6 months (range, 37.8–78.4 months).
Outcomes of BI-RADS category 4 and 5 lesions
Among the 214 BI-RADS 4 lesions (73 ipsilateral, 141 contralateral lesions), 101 (47.2%) underwent US-guided CNB, 7 (3.3%) underwent US-guided vacuum-assisted biopsy, 1 lesion (0.5%) underwent MR-guided biopsy, 65 (30.4%) were confirmed by surgery after biopsy, and 40 (18.7%) directly underwent surgical excision. None of 103 lesions followed up after benign-concordant biopsy had a delayed diagnosis of cancer, within a median follow-up of 59.6 months (range, 24.0–77.8 months).
Of the two BI-RADS 5 lesions (1 ipsilateral, 1 contralateral lesion), one malignancy (50.0%) was confirmed by surgery. The other lesion was downgraded to BI-RADS category 4a at targeted US and was confirmed as adenosis with apocrine change by US-guided CNB. It was considered as concordant benign and disappeared on subsequent follow-up MRI examinations obtained 25.2 and 59.5 months later.
Characteristics associated with malignancy risk
At first, we evaluated interobserver agreement between the two reviewers for lesion type (focus, mass, or NME), T2 hyperintensity and other imaging features. Kappa statistics showed perfect agreement except for margin of mass (0.76, substantial agreement) (Table E1, online).
Age, family history, and relative location of the additional lesion to the index cancer were not associated with malignancy risk for all lesion types. Associations between imaging characteristics and malignancy in mass lesions are presented in Table 2. Washout kinetics, irregular shape, non-circumscribed margin, and heterogeneous or rim enhancement were associated with malignancy at univariable analysis (p < 0.05). Benign masses tended to be hyperintense on T2-weighted images, but with borderline significance (p = 0.07). At multivariable analysis, washout kinetics, irregular shape, non-circumscribed margin, and rim enhancement were significantly associated with malignancy (p < 0.05). However, the malignancy rate of additional masses with no suspicious enhancing features (oval/round shape, circumscribed, homogeneous enhancement/dark internal septation, and persistent/plateau kinetics) was 3.9% (3/77). Among masses with no suspicious enhancing features showing T2 hyperintensity, the malignancy rate was 2.6% (1/39). For foci and NME lesions, there were no imaging features significantly different between benign and malignant lesions, although T2 hyperintensity was associated with the malignancy rate at univariable logistic regression analysis (p = 0.048) but not by Fisher’s exact test (p = 0.08) (Table E2 and E3, online).
Discussion
We found that the malignancy rates of BI-RADS 3 (1.4%) and 4 (17.8%) lesions detected at preoperative MRI were within the ranges specified by BI-RADS, with exception of BI-RADS category 5 (50%) due to the small number of cases (n = 2). It should be noted that the malignancy rate of additional lesions detected at preoperative MRI may differ from primary lesions, as these are candidates for multicentric or bilateral breast cancer. The overall prevalence of MRI-detected multicentric or bilateral breast cancer in our study was about 3.4% (42 out of 1252) during the study period, which was comparable with that in previous studies [26,27,28]. This may lower the PPV of BI-RADS in additionally detected lesions—however, we found that they were still within recommended ranges. We also found that the rate of delayed cancer diagnosis was very low (0.7%, 2/305) among BI-RADS 3 lesions and BI-RADS 4 lesions followed up after benign-concordant biopsy. In particular, none of the lesions that were followed up after benign-concordant biopsy had a delayed cancer diagnosis. At least in patients with breast cancer receiving adjuvant therapy, our results suggest that short-term follow-up is unnecessary for preoperative MRI-detected BI-RADS 3 lesions and BI-RADS 4 lesions followed up after benign-concordant biopsy. However, annual follow-up should be considered for additionally detected masses that are not confirmed with biopsy, considering the very low but possible delayed cancer diagnoses.
Whereas large-scale studies have suggested that annual follow-up might be sufficient for US-detected BI-RADS 3 lesions or concordant benign lesions after US-guided biopsy [16, 17, 29], the appropriate follow-up interval is still unresolved for MR-detected lesions. Established short-term follow-up recommendations for probably benign lesions or benign-concordant lesions after MR-guided biopsy are largely based on high-risk screening or heterogeneous populations, with a wide range of reported malignancy risk ranging from 0 to 10.1% [15, 18, 30,31,32]. Periodic surveillance may be appropriate for MRI BI-RADS 3 lesions in a scenario in which the stability of the finding is unknown, depending on factors that affect the probability of malignancy [18]. One difficulty in the management of BI-RADS 3 lesions in patients with newly diagnosed breast cancer is the unclear effect of adjuvant therapies on these lesions. As the patient is scheduled for treatment and has increased cancer risk, some physicians may prefer to confirm BI-RADS 3 lesions by biopsy, whereas some MRI-detected lesions may be effectively treated or suppressed by adjuvant therapies and therefore rendering short-term follow-up unnecessary. In this aspect, contralateral lesions may be more relevant as no radiation therapy is given to the contralateral breast [33]. One previous study reviewed BI-RADS 3 lesions on preoperative MRI and reported a low malignancy rate of 0.8%, with all delayed diagnoses being early-stage cancers detected after 24 months [34]. Two previous studies on preoperative MRI also reported a low malignancy risk of 0.9% among contralateral probably benign lesions [14, 22]. In a patient population in which almost all patients (97.4%) received at least one type of adjuvant therapy, we found similar results, although one missed contralateral T1 cancer was diagnosed after 13.3 months. In addition, none of the concordant benign lesions which underwent follow-up after biopsy had a delayed diagnosis of cancer. It is noteworthy that there were no delayed diagnoses in the ipsilateral breast during follow-up, possibly implying the effects of radiation therapy.
MRI imaging features associated with malignancy have been widely investigated—however, the majority of previous studies have focused on primary cancer lesions or were based on screening MRI in high-risk populations [35,36,37]. As additional lesions detected on preoperative MRI tend to be smaller than index lesions, additionally detected cancers may show relatively benign characteristics and thus cause difficulties in differential diagnosis and management [3, 38]. Several previous studies have associated delayed washout kinetics and lesions closer or ipsilateral to the main mass with malignancy, whereas hyperintensity on T2-weighted images was predictive of benignity in additional lesions [4, 24]. However, in our study, we found no significant association between lesion location and malignancy. This may be because we excluded ipsilateral lesions which were in the same quadrant as the main mass to ensure lesion-pathology matching and maximize the clinical impact of our study. In our study, benign mass lesions also tended to show T2 hyperintensity. Although none of the BI-RADS descriptors was significantly associated with malignancy in foci and NME, likely due to the small number of malignancies in these subgroups, we were able to confirm that known suspicious imaging features are well associated with malignancy in additionally detected masses at preoperative MRI. Our results showed that washout kinetics, irregular shape, non-circumscribed margin, and rim enhancement of additional masses were significantly associated with malignancy, suggesting that interpretation of additional lesions should not differ from that of breast lesions in general [39]. However, we found a 3.9% malignancy rate in masses without suspicious MRI features, similar to the results of previous studies [39,40,41,42]. Yet, annual follow-up can be confidently offered for additionally detected masses at preoperative MRI showing T2 hyperintensity without suspicious features, considering the low cancer rate (2.6%, 1/39) and early stage of missed cancers at diagnosis.
There are several limitations to our study. First, as the median follow-up period was 63.3 months, conclusions regarding late progression, especially following the termination of antihormonal therapy, cannot be drawn from our study results. Second, as a single tertiary institution, our findings may not be generalizable to clinical practice. Larger-scale studies with further long-term outcome data are needed to confirm our results, especially regarding follow-up management. Third, the possibility of misdiagnosis cannot be excluded. However, interobserver variability is an inevitable aspect of subjective assessments such as BI-RADS and of real clinical practice. Last, we excluded additional lesions located in the same quadrant as the primary cancer. However, this approach allowed a more robust outcome assessment for lesions undergoing follow-up. Furthermore, lesions located near the primary cancer may be less critical in clinical decision-making, as these lesions are more easily included in both the surgical and radiation field, even when more advanced radiotherapy techniques such as partial breast irradiation are applied.
In conclusion, the results of our study suggest that in a patient population in which most breast cancer patients receive adjuvant therapy, short-term follow-up is unnecessary for MRI-detected BI-RADS 3 and 4 lesions followed up after benign-concordant biopsy. Contralateral masses which were not confirmed by biopsy may need annual follow-up MRI. Clinically important missed diagnoses of cancer are unlikely and patients may undergo routine surveillance according to individual risk assessment.
Abbreviations
- CAD:
-
Computer-aided diagnosis
- CNB:
-
Core needle biopsy
- MRI:
-
Magnetic resonance imaging
- NME:
-
Nonmass enhancement
- US:
-
Ultrasound
References
Berg WA, Zhang Z, Lehrer D et al (2012) Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA 307:1394–1404
Morrow M, Waters J, Morris E (2011) MRI for breast cancer screening, diagnosis, and treatment. Lancet 378:1804–1811
Nam SJ, Kim E-K, Kim MJ, Moon HJ, Yoon JH (2015) Significance of incidentally detected subcentimeter enhancing lesions on preoperative breast MRI: role of second-look ultrasound in lesion detection and management. AJR Am J Roentgenol 204:W357–W362
Park SY, Han BK, Ko ES, Ko EY, Cho EY (2018) Additional lesions seen in magnetic resonance imaging of breast cancer patients: the role of second-look ultrasound and imaging-guided interventions. Ultrasonography. https://doi.org/10.14366/usg.18002
Hong MJ, Cha JH, Kim HH et al (2015) Second-look ultrasonography for MRI-detected suspicious breast lesions in patients with breast cancer. Ultrasonography 34:125–132
Beran L, Liang W, Nims T, Paquelet J, Sickle-Santanello B (2005) Correlation of targeted ultrasound with magnetic resonance imaging abnormalities of the breast. Am J Surg 190:592–594
Aracava MM, Chojniak R, Souza JA, Bitencourt AG, Marques EF (2014) Identification of occult breast lesions detected by magnetic resonance imaging with targeted ultrasound: a prospective study. Eur J Radiol 83:516–519
Leung JW (2011) Utility of second-look ultrasound in the evaluation of MRI-detected breast lesions. Semin Roentgenol 46:260–274
Bennani-Baiti B, Bennani-Baiti N, Baltzer PA (2016) Diagnostic performance of breast magnetic resonance imaging in non-calcified equivocal breast findings: results from a systematic review and meta-analysis. PLoS One 11:e0160346
Baltzer P, Schelhorn J, Dietzel M, Kaiser WA (2010) Breast screening programs using MRI: is there a role for computer-aided diagnosis. Imaging Med 2:659–673
Houssami N, Ciatto S, Macaskill P et al (2008) Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol 26:3248–3258
Spick C, Baltzer PA (2014) Diagnostic utility of second-look US for breast lesions identified at MR imaging: systematic review and meta-analysis. Radiology 273:401–409
Dietzel M, Baltzer PAT, Schön K, Kaiser WA (2012) MR-mammography: high sensitivity but low specificity? New thoughts and fresh data on an old mantra. Eur J Radiol 81:S30–S32
Weinstein SP, Hanna LG, Gatsonis C, Schnall MD, Rosen MA, Lehman CD (2010) Frequency of malignancy seen in probably benign lesions at contrast-enhanced breast MR imaging: findings from ACRIN 6667. Radiology 255:731–737
Spick C, Szolar DH, Baltzer PA et al (2014) Rate of malignancy in MRI-detected probably benign (BI-RADS 3) lesions. AJR Am J Roentgenol 202:684–689
Chae EY, Cha JH, Shin HJ, Choi WJ, Kim HH (2016) Reassessment and follow-up results of BI-RADS category 3 lesions detected on screening breast ultrasound. AJR Am J Roentgenol 206:666–672
Barr RG, Zhang Z, Cormack JB, Mendelson EB, Berg WA (2013) Probably benign lesions at screening breast US in a population with elevated risk: prevalence and rate of malignancy in the ACRIN 6666 trial. Radiology 269:701–712
Morris EA, Comstock CE, Lee CH et al (2013) ACR BI-RADS® Magnetic Resonance Imaging. In: D’Orsi CJ, Sickles EA, Mendelson EB et al (Eds) ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. American College of Radiology, Reston, VA
Spick C, Bickel H, Polanec SH, Baltzer PA (2017) Breast lesions classified as probably benign (BI-RADS 3) on magnetic resonance imaging: a systematic review and meta-analysis. Eur Radiol. https://doi.org/10.1007/s00330-017-5127-y
Burstein HJ, Lacchetti C, Anderson H et al (2016) Adjuvant endocrine therapy for women with hormone receptor–positive breast cancer: American Society of Clinical Oncology clinical practice guideline update on ovarian suppression. J Clin Oncol 34:1689–1701
Denduluri N, Chavez-MacGregor M, Telli ML et al (2018) Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO clinical practice guideline focused update. J Clin Oncol 36:2433–2443
Mahoney MC, Gatsonis C, Hanna L, DeMartini WB, Lehman C (2012) Positive predictive value of BI-RADS MR imaging. Radiology 264:51–58
Gutierrez RL, DeMartini WB, Eby PR, Kurland BF, Peacock S, Lehman CD (2009) BI-RADS lesion characteristics predict likelihood of malignancy in breast MRI for masses but not for nonmasslike enhancement. AJR Am J Roentgenol 193:994–1000
Song SE, Park EK, Cho KR et al (2017) Additional value of diffusion-weighted imaging to evaluate multifocal and multicentric breast cancer detected using pre-operative breast MRI. Eur Radiol 27:4819–4827
Firth D (1993) Bias reduction of maximum likelihood estimates. Biometrika 80:27–38
Iacconi C, Galman L, Zheng J et al (2016) Multicentric cancer detected at breast MR imaging and not at mammography: important or not? Radiology 279:378–384
Brennan ME, Houssami N, Lord S et al (2009) Magnetic resonance imaging screening of the contralateral breast in women with newly diagnosed breast cancer: systematic review and meta-analysis of incremental cancer detection and impact on surgical management. J Clin Oncol 27:5640–5649
Sakai T, Ozkurt E, DeSantis S et al (2019) National trends of synchronous bilateral breast cancer incidence in the United States. Breast Cancer Res Treat 178:161–167
Ruamsup S, Wiratkapun C, Wibulpolprasert B, Lertsithichai P (2010) A comparison between short-interval and regular-interval follow-up for BI-RADS category 3 lesions. Singapore Med J 51:120
Chikarmane SA, Birdwell RL, Poole PS, Sippo DA, Giess CS (2016) Characteristics, malignancy rate, and follow-up of BI-RADS category 3 lesions identified at breast MR imaging: implications for MR image interpretation and management. Radiology 280:707–715
Li J, Dershaw DD, Lee CH, Kaplan J, Morris EA (2009) MRI follow-up after concordant, histologically benign diagnosis of breast lesions sampled by MRI-guided biopsy. AJR Am J Roentgenol 193:850–855
Lee KA, Talati N, Oudsema R, Steinberger S, Margolies LR (2018) BI-RADS 3: current and future use of probably benign. Curr Radiol Rep 6:5–5
Mann R, Balleyguier C, Baltzer P et al (2015) Breast MRI: EUSOBI recommendations for women’s information. Eur Radiol 25
Gweon HM, Cho N, Kim SY et al (2017) Management for BI-RADS category 3 lesions detected in preoperative breast MR imaging of breast cancer patients. Eur Radiol 27:3211–3216
Liberman L, Morris EA, Lee MJ et al (2002) Breast lesions detected on MR imaging: features and positive predictive value. AJR Am J Roentgenol 179:171–178
Schnall MD, Blume J, Bluemke DA et al (2006) Diagnostic architectural and dynamic features at breast MR imaging: multicenter study. Radiology 238:42–53
Wedegartner U, Bick U, Wortler K, Rummeny E, Bongartz G (2001) Differentiation between benign and malignant findings on MR-mammography: usefulness of morphological criteria. Eur Radiol 11:1645–1650
Meissnitzer M, Dershaw DD, Feigin K, Bernard-Davila B, Barra F, Morris EA (2017) MRI appearance of invasive subcentimetre breast carcinoma: benign characteristics are common. Br J Radiol 90:20170102
Baum F, Fischer U, Vosshenrich R, Grabbe E (2002) Classification of hypervascularized lesions in CE MR imaging of the breast. Eur Radiol 12:1087–1092
Price ER, Sickles EA, Yitta S et al (2018) Use of the probably benign (BI-RADS category 3) assessment for masses on breast MRI: is it transferable to general clinical practice? Breast J 24:109–114
Fujiwara K, Yamada T, Kanemaki Y et al (2018) Grading system to categorize breast MRI in BI-RADS 5th edition: a multivariate study of breast mass descriptors in terms of probability of malignancy. AJR Am J Roentgenol 210:W118–w127
Baltzer PAT, Dietzel M, Kaiser WA (2013) A simple and robust classification tree for differentiation between benign and malignant lesions in MR-mammography. Eur Radiol 23:2051–2060
Funding
This study has received funding by National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2017R1D1A1B03035995).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Vivian Youngjean Park, MD, PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise (Kyunghwa Han, PhD).
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Lee, S.E., Lee, J.H., Han, K. et al. BI-RADS category 3, 4, and 5 lesions identified at preoperative breast MRI in patients with breast cancer: implications for management. Eur Radiol 30, 2773–2781 (2020). https://doi.org/10.1007/s00330-019-06620-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06620-y