Abstract
Objective
To retrospectively evaluate characteristics of and determine appropriate follow-up recommendations for BI-RADS category 3 lesions detected in preoperative MRI of breast cancer patients.
Methods
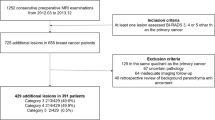
BI-RADS category 3 assessments were identified from the breast MRI database for 5,110 consecutive breast cancer patients who had undergone preoperative MRI and surgery. Patient and lesion characteristics, malignancy rate, and interval between lesion detection and cancer diagnosis were analysed. Histopathological results or imaging at or after 2-year follow-up were used as reference standards.
Results
Of the 626 lesions, morphological features included a single focus in 26.5% (n = 166), multiple foci in 47.1% (n = 295), mass in 21.7% (n = 136) and non-mass enhancement in 4.6% (n = 29). Cancer was found in 0.8% (5/626) at a median interval of 50 months (range, 29–66 months). Malignancy rate according to morphological feature was: 1.8% (3/166) in a single focus, 0.7% (1/136) in mass and 3.4% (1/29) in non-mass enhancement. All detected cancers were stage 0 or IA.
Conclusions
Annual follow-up might be adequate for BI-RADS category 3 lesions detected at preoperative MRI because of the 0.8% (5/626) malignancy rate, long interval between lesion detection and cancer diagnosis, and early stage of diagnosed cancers.
Key Points
• BI-RADS category 3 lesions on preoperative MRI had 0.8% malignancy rate.
• All cancer diagnoses from BI-RADS 3 occurred after 24-month follow-up.
• Annual follow-up might be adequate for BI-RADS 3 detected on preoperative MRI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It has been well established that Breast Imaging Reporting and Data System (BI-RADS) final assessment category 3 lesions, having malignancy rates of less than 2% for mammography, should be managed with short-term imaging follow-up (typically at 6, 12 and 24 months) rather than biopsy [1, 2]. Short-term follow-up is advantageous because it avoids the risks and costs of invasive tissue sampling for the majority of benign lesions. In addition, the few malignancies detected at follow-up imaging have been small and at an early stage [1–6].
In the field of breast magnetic resonance (MR) image interpretation, previous studies have used various criteria for BI-RADS category 3 assessments in different populations, with the reported incidence of BI-RADS category 3 assignment ranging from 6% to 8.5% and their malignancy rate ranging from 0.9% to 4.3% [7–10]; these results are comparable with those from mammography. Similar to mammography screening, short-term follow-up (at 6, 12 and 24 months) has been recommended for category 3 lesions detected at MR imaging; however, there has been a lack of evidence regarding short-term follow-up for BI-RADS category 3 lesions detected at MR imaging [11]. Considering the high cost, high false-positive rate and intolerability of MR examinations, appropriate management recommendations should be further investigated. Previous studies have shown that 10.9% of patients undergoing preoperative MR imaging after the diagnosis of breast cancer have coincidental lesions with BI-RADS category 3 [12]. Unlike women undergoing screening MR imaging, women receiving preoperative MR imaging subsequently undergo surgery, chemotherapy or radiation therapy, which may lead to decreased screening sensitivity as well as decreased tumour growth. Therefore, the purpose of our study was to retrospectively evaluate characteristics of and determine appropriate follow-up recommendations for BI-RADS category 3 lesions detected at preoperative MR imaging of patients with newly diagnosed breast cancers.
Materials and methods
Subject population
Our Institutional Review Board approved this retrospective analysis, and informed consent was waived. Between January 2007 and December 2012, prospectively recorded BI-RADS category 3 assessments were identified from the breast MR imaging database. Of the 5,110 consecutive women who had undergone preoperative MR examinations and curative surgery for breast cancer, 683 (13.4%) women had BI-RADS category 3 lesions. Among them, 57 women were excluded due to unavailability of 2-year follow-up data (n = 45) or total mastectomy including BI-RADS category 3 lesions (n = 12). We excluded cases with total mastectomy as their reference standard was not available. Histopathological mapping or surgical excision after localization was not routinely performed for BI-RADS category 3 lesions. Finally, 626 BI-RADS category 3 lesions in 626 women (median age, 47 years; range, 23–81 years) comprised our study population (Table 1). Of the 626 women, 7.8% (49/626) had familial history of breast cancer (n = 43) or were BRCA mutation carriers (n = 6).
MR imaging evaluation
All MR examinations were performed using a 1.5-T MR imager (Signa; GE Medical System, Milwaukee, WI, USA) with a dedicated eight-channel bilateral breast coil (GE Medical System). Sagittal fat-suppressed T2-weighted fast spin-echo MR imaging was performed using the following image parameters: repetition time msec/echo time msec, 5,500–7,150/85.2; matrix, 256 × 160; field of view, 200 × 200 mm; section thickness, 1.5 mm; no gap. Dynamic contrast-enhanced MR examinations included one pre-contrast and five post-contrast bilateral sagittal image acquisitions using a fat-suppressed T1-weighted three-dimensional fast spoiled gradient-echo sequence with parallel imaging (6.5/2.5; matrix, 256 × 160; flip angle, 10°; field of view, 200 × 200 mm; section thickness, 1.5 mm; no gap). The acquisition time of each post-contrast series was 76 s. Five post-contrast image series were obtained at 91, 180, 360, 449 and 598 s after the start of contrast administration. A dose of 0.1 mmol/kg gadobutrol (Gadovist, Bayer Healthcare, Berlin, Germany) was injected into an antecubital vein using an automated injector (Spectris Solaris; Medrad Europe, Maastricht, The Netherlands) at a rate of 2 ml/s, followed by a 20-ml saline flush.
MR imaging interpretation
MR imaging was prospectively interpreted by one of five radiologists with 7–15 years of experience in breast MR interpretation and intervention according to the fourth edition of BI-RADS lexicon on a Picture Archiving and Communication System (PACS) [11]. The following characteristics indicated a BI-RADS category 3 assessment: (1) an oval or round mass with circumscribed margin and without suspicious kinetics; (2) focal or regional non-mass enhancements (NME) with internal homogeneous or stippled pattern; (3) isolated and dominant focus without suspicious kinetics; and (4) multiple bilateral foci, including prominent foci. Multiple bilateral and diffusely distributed foci represented background parenchymal enhancement and were considered BI-RADS category 2 [13]. However, multiple bilateral foci with some asymmetrical distribution or lesions including several prominent foci were considered BI-RADS category 3. Kinetic features were assessed by drawing a region of interest over the most suspicious portion of the lesion to measure the signal intensity change through dynamic images on a PACS. High-resolution PACS monitors were used for interpretation in conjunction with patients’ clinical history and other breast imaging examinations including mammography or ultrasound (US). One day before surgery, all patients routinely underwent preoperative mammography and US in addition to MR examinations. The BI-RADS final assessment category was determined and recorded based on MR images in conjunction with mammography and US findings [11].
To evaluate interobserver variability of MR image interpretations, three fellowship-trained breast radiologists independently reanalysed MR images according to the BI-RADS Atlas [11] without knowledge of the original MR image interpretations and histopathological information.
Follow-up protocol
For BI-RADS category 3 lesions detected at preoperative MR imaging, 6-, 12- and 24-month follow-up MR imaging was recommended. When the lesion was determined have a correlative mammography or US finding, follow-up was performed with mammography or US. If the lesion was stable for 24 months, it was downgraded to BI-RADS category 2. Annual mammography with US was performed thereafter. If the BI-RAS category 3 lesion exhibited increase in size or change in shape during follow-up, a biopsy was performed.
Data and statistical analysis
The patient and lesion characteristics, all available images, histopathology results, and the interval between lesion detection and cancer diagnosis were reviewed. Rate of malignancy from BI-RADS category 3 lesions was calculated. Independent sample t tests or Fisher’s exact tests were used to compare characteristics between women with subsequently breast cancer diagnosis and women without cancer.
In addition, hypothetical changes in the frequency and malignancy rate of BI-RADS category 3 lesions were calculated to identify an adequate definition of BI-RADS category 3 assessment to reduce false-positive findings and to achieve malignancy rate less than 2%.
Interobserver variability for interpretation of MR images of three radiologists was evaluated by calculating the Fleiss kappa (k) coefficient. A kappa statistic of 0.2 or less was considered slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–0.99, almost perfect agreement [14]. All statistical analyses were performed using statistical software (SPSS, version 20.0; SPSS, Chicago, IL, USA). A P value of less than .05 was considered a significant difference.
Results
Of the 626 BI-RADS category 3 lesions, 166 (26.5%) had a single focus, 295 (47.1%) had multiple foci, 136 (21.7%) had masses, and 29 (4.6%) had NME on initial MR images (Table 2). A case of bilateral multiple foci was counted as one lesion. During follow-up, percutaneous biopsy or surgical excision was performed for 37 (5.9%) lesions due to interval change. Among them, 32 (86.5%) were benign and 5 (13.5%) were cancers.
With regard to the characteristics of malignant cases, 80% (4 of 5) were invasive ductal carcinoma (median tumour size, 0.6 cm; range, 0.1-1.0 cm) and 20% (1 of 5) were ductal carcinoma in situ (Table 3). Eighty% of them (4/5) were found in the contralateral breast and 20% were in the ipsilateral breast (Table 3). Three cancers presented as increased masses at follow-up US. The other two cancers presented as increased microcalcifications at follow-up mammography. No cancer was found at follow-ups prior to 24 months after initial MR images. Two cancers were diagnosed at a 25 month to 48 month follow-up interval. The other three cancers were diagnosed at a 49 month to 72 month follow-up interval. Thus, the malignancy rate was 0.8% (5 of 626).
The cancers originally presented on preoperative MR images as a focus in 3 cases (Fig. 1), a mass in one case and a NME in one case (Table 2). No cancer was found in the remaining 589 lesions at a median of 53 months (mean 53 months; range 25-82 months) imaging follow-up; of the 589 lesions, 148 disappeared and 441 decreased or showed stability (Fig. 2). When the finding of multiple foci (Fig. 3) was reclassified as category 2 assessment, the frequency of BI-RADS category 3 assessment changed from 13.4% (683 of 5110) to 7.6% (388 of 5110) and malignancy rate changed from 0.8% (5 of 626) to 1.5% (5 of 331).
Post-contrast-enhanced axial MR images in a 66-year-old woman who underwent breast-conserving surgery for invasive breast cancer in the right breast. This case indicates a malignant case arising from BI-RADS category 3 lesion. (a) Preoperative breast MR image demonstrates a focus in the left breast that was assessed to be a BI-RADS category 3. (b) At 54-month-follow-up, the focus appears larger. Core needle biopsy and surgical histopathology revealed a 0.7-cm invasive ductal carcinoma
Post-contrast-enhanced sagittal MR images in a 46-year-old woman who underwent breast conserving surgery, radiation therapy and adjuvant chemotherapy with tamoxifen for invasive breast cancer in the left breast. This case indicates a decreased size of the case initially classified as BI-RADS category 3. (a) Preoperative breast MR image demonstrates an 8-mm enhancing mass in the left breast that was assessed to be BI-RADS category 3. (b) At 12-month-follow-up MR examination, the mass had decreased to 7 mm. (c) At 42-month-follow-up MRI, the mass had further decreased to 5 mm
Post-contrast-enhanced sagittal MR images in a 48-year-old woman who underwent breast-conserving surgery, radiation therapy and adjuvant chemotherapy for invasive breast cancer in the right breast. This case indicates a disappeared case initially classified as BI-RADS category 3. (a) Preoperative breast MR image of right breast demonstrates multiple foci with prominent foci in the left breast that was assessed to be BI-RADS category 3. (b) At 7-month-follow-up MRI, the multiple foci disappeared. (c) At 45-month-follow-up MRI, no cancer was found
The overall agreement for interpretation of lesion morphologic features was substantial (k = 0.63). Substantial agreement for mass shape (k = 0.61), mass margin (k = 0.78), and almost perfect agreement for distribution of NME was (k = 0.89) found.
Discussion
Our results showed that the malignancy rate of BI-RADS category 3 lesions detected at preoperative breast MR imaging was 0.8% (5/621), and cancers were detected at a median of 50 months (range, 29–66 months) imaging follow-up.
Our study’s 0.8% malignancy rate of BI-RADS category 3 lesions is in accordance with the less than 2% malignancy rate suggested for BI-RADS category 3 assessment in the field of screening mammography [1–4, 15]. However, our result is lower than that in previous studies using MR images, in which the malignancy rates ranged from 0.9–4.3% [7–11]. Grimm et al. reported a 4.3% malignancy rate in a study including 57.5% high–risk screening [9]. Spick et al. reported a 0.9% malignancy rate in a study including patients who were not at high risk for breast cancer and had no personal history of breast cancer [8], which is closer to our result. Another recent study reported that the malignancy rate of BI-RADS category 3 lesions was greater in women with a personal breast cancer history or germline mutation than women without such risk factors (3.8% vs. 0%) [10]. In that study, no malignancy was found in the 27 preoperative MR examinations to evaluate disease extent [10]. Based on our results and those of previous studies, the malignancy rate for BI-RADS category 3 lesions is higher for high-risk screening than in the preoperative MRI setting for newly diagnosed cancer patients.
Although the BI-RADS Atlas has not suggested different management recommendations based on the indications of breast MR examinations, women with BI-RADS category 3 lesions on MR images have heterogeneous risk for the occurrence of another breast cancer; thus, consideration of tailored follow-up recommendations might be warranted. In our study, five cancers arising from BI-RADS category 3 lesions were detected during a long interval period (median, 50 months, range, 29–66 months) between initial detection and cancer diagnosis. Notably, no cancer was found at less than 24 months follow-up. However, previous studies including high-risk populations have reported that the majority of cancers from BI-RADS category 3 lesions were detected during a 24-month follow-up period [7–10, 16]. In addition, researchers have found a tumour growth rate of approximately 5 mm per year; thus, a 6-month follow-up is important for high-risk women with a germline mutation having a small enhancing lesion on MR imaging [17]. Contrastingly, as the majority of our study population were newly diagnosed breast cancer patients receiving systemic chemotherapy or endocrine therapy to reduce second breast cancer occurrence, short-term follow-up imaging for BI-RADS category 3 lesions detected on preoperative MRI might not be beneficial. Moreover, although 7.8% (49/626) of our population had a familial history of breast cancer or were BRCA mutation carriers, no cancer was found in this population. This might have been associated with the effect of adjuvant therapy.
All detected cancers from BI-RADS category 3 lesions in our study were node negative T1 invasive cancers (median tumour size, 0.6 cm; range, 0.1–1.0 cm) or ductal carcinoma in situ (DCIS), which is comparable to the results of other studies. In addition, there was no difference in malignancy rate according to the lesion type on MRI in our study. Of the five cancers, three presented with a focus, one presented with a mass and one presented with NME. Although Grimm et al. reported that non-mass enhancements assessed as BI-RADS category 3 were significantly more likely to be malignant [9], other previous studies found that no significant morphological characteristics were predictive of malignant BI-RADS category 3 lesions on MR imaging [ 7, 8, 10, 11]. In our study, no cancer was found in the lesions presenting with multiple foci. Thus, as a previous study recommended [12], when the multiple foci in our study had been re-classified as BI-RADS category 2, the frequency rate changed from 13.4% (683/5,110) to 7.6% (388/5,110); this is in line with recent BI-RADS Atlas recommendations that the frequency of BI-RADS category 3 should be less than 10% [14].
Our study has several limitations. First, because this was a retrospective study from a single institution and a relatively small number of patients with very small number of malignant cases were included, we cannot draw a solid conclusion. Second, follow-up MR imaging was not routinely performed in our study. If correlative findings were shown on mammography and US at the time of BI-RADS category 3 diagnosis, follow-ups were performed with mammography or US.
In conclusion, annual follow-up rather than short-term follow-up might be adequate for BI-RADS category 3 lesions detected on preoperative MRI based on the low malignancy rate, long interval between lesion detection and cancer occurrence, and early stage of detected cancers identified in this study. In addition, our results confirmed that although lesions with bilateral multiple foci exhibited several prominent foci or asymmetrical distribution, they were compatible with BI-RADS category 2 assessment. Considering the cost and availability of MR examinations, the use of BI-RADS category 3 on preoperative MR imaging should be further restricted.
References
Sickles EA (1991) Periodic mammographic follow-up of probably benign lesions: results in 3,184 consecutive cases. Radiology 179:463–468
Varas X, Leborgne F, Leborgne JH (1992) Nonpalpable, probably benign lesions: role of follow-up mammography. Radiology 184:409–414
Varas X, Leborgne JH, Leborgne F, Mezzera J, Jaumandreu S, Leborgne F (2002) Revisiting the mammographic follow-up of BI-RADS category 3 lesions. AJR Am J Roentgenol 179:691–695
Vizcaino I, Gadea L, Andreo L et al (2001) Short-term follow-up results in 795 nonpalpable probably benign lesions detected at screening mammography. Radiology 219:475–483
Chae EY, Cha JH, Shin HJ, Choi WJ, Kim HH (2016) Reassessment and follow-up results of BI-RADS category 3 lesions detected on screening breast ultrasound. AJR Am J Roentgenol 206:666–672
Chung CS, Giess CS, Gombos EC et al (2014) Patient compliance and diagnostic yield of 18-month unilateral follow-up in surveillance of probable benign mammographic lesions. AJR Am J Roentgenol 202:922–927
Lourenco AP, Chung MT, Mainiero MB (2014) Probably benign breast MRI lesions: frequency, lesion type, and rate of malignancy. J Magn Reson Imaging 39:789–794
Spick C, Szolar DH, Baltzer PA et al (2014) Rate of malignancy in MRI-detected probably benign (BI-RADS 3) lesions. AJR Am J Roentgenol 202:684–689
Grimm LJ, Anderson AL, Baker JA et al (2015) Frequency of malignancy and imaging characteristics of probably benign lesions seen at breast MRI. AJR Am J Roentgenol 205:442–447
Chikarmane SA, Birdwell RL, Poole PS, Sippo DA, Giess CS (2016) Characteristics, malignancy rate, and follow-up of BI-RADS category 3 lesions identified at breast MR imaging: implications for MR image interpretation and management. Radiology. doi:10.1148/radiol.2016151548:151548
Ikeda DM, Hylton NM, Kuhl CK et al (2003) ACR BI-RADS® magnetic resonance imaging. In: ACR BI-RADS® atlas, breast imaging and reporting and data system, Reston, VA, American College of Radiology
Weinstein SP, Hanna LG, Gatsonis C, Schnall MD, Rosen MA, Lehman CD (2010) Frequency of malignancy seen in probably benign lesions at contrast-enhanced breast MR imaging: findings from ACRIN 6667. Radiology 255:731–737
Eby PR, DeMartini WB, Gutierrez RL, Lehman CD (2010) Probably benign lesions detected on breast MR imaging. Magn Reson Imaging Clin N Am 18:309–321
Fleiss JL (1971) Measuring nominal scale agreement among many raters. Psychol Bull 76:378–382
Gruber R, Jaromi S, Rudas M et al (2013) Histologic work-up of non-palpable breast lesions classified as probably benign at initial mammography and/or ultrasound (BI-RADS category 3). Eur J Radiol 82:398–403
Eby PR, DeMartini WB, Gutierrez RL, Saini MH, Peacock S, Lehman CD (2009) Characteristics of probably benign breast MRI lesions. AJR Am J Roentgenol 193:861–867
Gilbert FJ, Warren RM, Kwan-Lim G et al (2009) Cancers in BRCA1 and BRCA2 carriers and in women at high risk for breast cancer: MR imaging and mammographic features. Radiology 252:358–368
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Nariya Cho.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Methodology
-
retrospective
-
observational
-
performed at one institution
Rights and permissions
About this article
Cite this article
Gweon, H.M., Cho, N., Kim, SY. et al. Management for BI-RADS category 3 lesions detected in preoperative breast MR imaging of breast cancer patients. Eur Radiol 27, 3211–3216 (2017). https://doi.org/10.1007/s00330-016-4721-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4721-8