Abstract
Objectives
To determine the sensitivity and positive predictive value (PPV) of gadobenate-enhanced MR imaging for the detection of liver metastases.
Methods
This systematic review and meta-analysis was conducted according to PRISMA guidelines. A comprehensive search (EMBASE, PubMed) was performed to identify relevant articles up to December 2017. Studies eligible for inclusion were performed using appropriate methodology with complete verification by means of histopathology, intraoperative observation and/or follow-up, and sufficient information to permit determination of true-positive (TP), false-negative (FN), and false-positive (FP) values. Sources of bias were assessed using the QUADAS-2 tool. An inverse variance-weighted random-effects model was used to obtain sensitivity and PPV estimates. Information was analyzed and presented using Cochran’s Q statistic, funnel plots, and modified Deeks’ analysis.
Results
Ten articles (256 patients, 562 metastases) were included. Sensitivity estimates for pre-contrast (unenhanced) imaging, gadobenate-enhanced dynamic imaging, and combined unenhanced, dynamic, and delayed hepatobiliary phase imaging for detecting liver metastases on a per-lesion basis were 77.8% (95% CI 71.4–84.3%, 7 assessments), 88.1% (95% CI, 84.0–92.2%, 13 assessments), and 95.1% (95% CI 93.1–97.1%, 15 assessments), respectively. The addition of hepatobiliary phase images significantly improved the detection of liver metastases. The overall PPV was 90.9% (95% CI 86.6–95.1%, 11 assessments). Deeks’ funnel analysis revealed no association between sample size and sensitivity (β = 0.02, p = 0.814) indicating no significant publication bias.
Conclusions
Gadobenate-enhanced MR imaging has high sensitivity and PPV for the detection of liver metastases on a per-lesion basis. The sensitivity and PPV for detection is comparable to reported values for the pure liver-specific agent gadoxetate.
Key Points
• Gadobenate dimeglumine is a hepatobiliary MR contrast agent that permits acquisition of contrast-enhanced liver images during the immediate post-injection dynamic phase, like any extracellular agent, and in the delayed hepatobiliary phase, after specific uptake by the hepatocytes.
• The hepatobiliary phase improves detection of liver metastases when compared either to pre-contrast unenhanced images alone or to pre-contrast + gadobenate-enhanced dynamic phase images.
• The meta-analysis showed an overall sensitivity of 95.1% and PPV of 90.9% of gadobenate-enhanced MRI for the detection of metastases, when based on the evaluation of all available acquisitions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate determination of the number and location of liver metastases is crucial to the staging of extra-hepatic metastatic cancer in order to better guide patient management decisions for improved therapeutic outcome [1, 2]. Of the non-invasive imaging modalities available for the detection of liver metastases, contrast-enhanced MRI with liver-specific contrast agents offers improved diagnostic performance as compared with other imaging modalities [1,2,3,4,5,6]. Currently, two gadolinium-based contrast agents (GBCAs) with liver-specific properties are available: gadoxetate trisodium (Primovist/Eovist; Bayer Healthcare [7]) and gadobenate dimeglumine (MultiHance; Bracco [8]). These agents gain their liver-specific properties from aromatic substituents on their chelating molecules [9,10,11,12,13] but differ in that whereas ~ 50% of the administered dose of gadoxetate is taken up by functioning hepatocytesin patients with normal renal function, this percentage is lower for gadobenate at 3–5% of the administered dose [9,10,11,12]. A consequence of the greater and more rapid uptake of gadoxetate is that this agent is exclusively dedicated to liver imaging [7]. Conversely, whereas gadobenate is approved in Europe only for liver imaging [8], it has several extra-hepatic indications elsewhere in the world [14] and whole body approval in China.
Several meta-analyses have reported sensitivities of > 90% for the detection of liver metastases on gadoxetate-enhanced MRI [15,16,17,18]. However, to our knowledge, despite numerous studies that have evaluated gadobenate for the detection of liver metastases, no meta-analysis of diagnostic performance has yet been performed. Moreover, as noted recently in an ESGAR consensus statement on liver MRI and the use of liver-specific contrast agents [19], very few studies have directly compared gadobenate and gadoxetate for diagnostic performance and no data are available about diagnostic superiority for one agent over the other. This is especially true for metastasis detection which is a primary application of liver-specific contrast agents.
Our purpose was to perform a meta-analysis of sensitivity and PPV data for the detection of liver metastases on gadobenate-enhanced MRI and to interpret these findings relative to those reported for gadoxetate.
Methods
This systematic review was conducted according to the recommendations of the PRISMA guidelines (Table 1 [20]).
Data sources and searches
A systematic and comprehensive search was performed for publications through December 2017 using MEDLINE and EMBASE databases. The search was conducted using the search terms: “MultiHance” OR “gadobenate” OR “Gd-BOPTA” and liver MRI. Conference proceedings identified in the search, references cited within eligible articles, or meta-analysis reports were assessed for potential inclusion if they met the eligibility criteria. The results were limited to human data, and excluded conference abstracts, reviews, case reports, editorials, comments, conference reviews, news, congresses and letters.
Eligibility criteria
A study was considered eligible for inclusion if it had prospective or retrospective enrollment of patients referred for gadobenate-enhanced MRI for the detection of focal liver lesions including liver metastases; was performed using appropriate methodology with adequate description of the MRI procedure; had complete verification by means of a relevant and adequate reference standard test (typically histology, intraoperative ultrasound [IOUS], and/or additional follow-up diagnostic imaging); and provided specific lesion detection information in absolute numbers of metastases so as to permit determination of true-positive (TP), false-negative (FN), and false-positive (FP) values.
A study was not eligible for inclusion if it utilized other contrast agents in addition to gadobenate; if it did not meet the research objectives of this study; or if there was evidence of duplicated articles or overlap of patient enrollment at the same institution by the same authors.
Data extraction and quality appraisal
Data extraction from eligible studies was performed by one physician and one statistician. Inconsistencies were resolved by discussion and consensus. Meta-analysis was based on individual reader findings for studies involving multiple blinded readers. The following data were extracted into a prospectively defined excel form: (1) study characteristics: authors, journal, year of publication, study design; (2) study population characteristics: type of liver disease and lesion, mean age and standard deviation if available, gender; (3) purpose of MRI (detection or characterization of liver lesion), field strength, imaging review methods (consensus review or multiple reader independent review), blinded or unblinded image review; (4) reference standard details; (5) diagnostic performance outcome: number of metastases detected by reference standard, lesion size. The number of TP lesions, FN lesions, and FP lesions as well as sensitivity and positive predictive value (PPV) for lesion detection were extracted from the tables, text, or figures as applicable. Because the number of “true negative” lesions was not reported in 8 of the 10 papers included in the meta-analysis, specificity could not be calculated.
Assessment of study quality
Study quality, including risk of bias and applicability, was assessed according to Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) guidelines [21]. Assessment was independently performed by two reviewers. Discrepancies were resolved by consensus.
Statistical methods
The numbers of TP, FN, and FP lesions in each study were extracted on a per-lesion basis. If only sensitivity and/or PPV values were reported in a study, TP, FN, and FP were calculated. For the purposes of the analysis, if zero FN or FP lesions were reported, a 0.5 lesion was imputed for the continuity correction. Results from the assessment of all image sets combined were used for the primary meta-analysis. Subgroup analyses of pre-contrast unenhanced images alone and pre-contrast plus gadobenate-enhanced dynamic phase images alone were performed for all studies that reported appropriate data. Comparisons between the pooled assessments of sensitivity and PPV for metastasis detection were presented along with 95% confidence intervals (CI) using the same meta-analysis method.
An inverse variance-weighted random-effects model was used to calculate summary estimates of sensitivity and PPV and account for variance within and between studies [22] while random-effects models were used to allow for potential heterogeneity between studies [23]. Summary estimates calculated using the inverse variance-weighted random-effects model were compared with estimates calculated using a fixed-effect model.
Forest plots were prepared to display the individual sensitivity and PPV values and 95% CI from each assessment in each study, together with the pooled sensitivity and PPV based on the reviewers’ assessments of all studies combined and the relative weight that each study contributed.
Statistical heterogeneity was assessed using Cochran’s Q statistic of the chi-square test (p < 0.05 indicating significant heterogeneity), as well as the inconsistency index I2 statistic to quantify the magnitude of between-study heterogeneity of the individual studies [24]. I2 values of ≤ 50%, 51%–75%, and > 75% indicate low, moderate, and high heterogeneity, respectively [25].
Possible publication bias was visually examined from a funnel plot of the study sample size (y-axis) against sensitivity (x-axis) reported in each study. A modified Deeks’ test based on sensitivity values and sample size was used to test asymmetries of the funnel plots [26, 27]. A significant non-zero slope coefficient (p < 0.05) indicates potential publication bias due to an association between sample size and sensitivity.
All statistical analyses were 2-sided and were performed using SAS version 9.2 software (SAS Institute, Inc.).
Results
Study selection
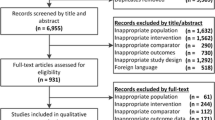
Among 354 post-approval publications that reported data on the use of gadobenate in liver MR imaging, ten [28,29,30,31,32,33,34,35,36,37] reported sensitivity data for the detection of hepatic metastases or presented sufficient information to enable extraction of the necessary data (Fig. 1). Five were original prospective studies [29,30,31, 35, 37] while five [28, 32,33,34, 36] were retrospective analyses. All but two studies [28, 36] were single-center. A total of 256 patients (mean age range 55–68 years, male 50%–72%) with 562 hepatic metastases confirmed by histology and/or IOUS or imaging follow-up were included (Table 2). Precise information on underlying primary malignancy was available in 9 studies [28,29,30,31,32, 34,35,36,37] and included colorectal cancer (n = 152), breast cancer (n = 18), stomach cancer (n = 20), pancreatic cancer (n = 9), renal cancer (n = 7), lung cancer (n = 6), “other” (n = 15), and “unknown” (n = 1). The remaining patients had underlying primary malignancy that was not defined.
All imaging studies but two [28, 29] were acquired using a 1.5-T scanner. Typical protocols included T2-weighted Turbo Spin-Echo or HASTE and 3D GRE including VIBE or THRIVE with the exception of two studies [28, 29]. Diffusion-weighted imaging (DWI) was not performed in any of the studies included in the meta-analysis. The nine studies [28, 30,31,32,33,34,35,36,37] in which dynamic phase imaging was performed typically saw arterial, portal-venous, and equilibrium phase images acquired. Seven studies [30,31,32,33,34,35, 37] utilized gadobenate at a dose of 0.1 mmol/kg bodyweight while two studies [29, 36] utilized a dose of 0.05 mmol/kg bodyweight. The final study [28] utilized an initial dose of 0.05 mmol/kg bodyweight for dynamic phase acquisitions and then infused a second 0.05 mmol/kg dose immediately after the dynamic scans prior to acquisition of delayed (60–120 min) hepatobiliary phase images. In three studies [32, 33, 35] hepatobiliary images were not acquired and sensitivity and PPV was determined from the assessment of dynamic phase images only. In the remaining seven studies, hepatobiliary phase images were acquired after a fixed delay of 60 [29,30,31] or 120 [37] min or at a variable time-point between 40 and 195 min [28, 34, 36] post-injection.
The distribution of the 11 signaling questions from the QUADAS-2 guidelines for risk of bias is shown in Table 3 while the overall score for each of the four domains for risk of bias and three domains for applicability concerns are shown in Fig. 2. All studies scored well for most of the signaling questions except for unclear information about blinded assessment of the reference standard for 70% of the studies. Overall, 80% of the studies had different reference standards across patients (i.e., a mix of histopathology and follow-up imaging). Other studies used histopathology only. Methodological shortcomings for the risk of bias were considered unclear most frequently for the reference standard domain (70%) and for the patient selection and index test domains (30%). A risk of bias in flow and timing was considered unclear in very few (20%) instances. Overall, no study had a sufficiently high risk of bias to warrant exclusion.
There was no significant association between sample size and sensitivity (β = 0.02, p = 0.814) indicating no significant publication bias. Visual observation of the modified funnel plot (Fig. 3) showed that published small sample size studies reported both low and high sensitivity values.
Detection of liver metastases
Individual study results are shown in Table 4 and Figs. 4 and 5. Sensitivity values ranged from 61.0 to 86.1% for pre-contrast unenhanced images (6 studies; 7 assessments), 76.3–98.0% for pre-contrast plus gadobenate-enhanced dynamic phase images alone (8 studies; 13 assessments), and 79.7–100.0% for combined pre-contrast, dynamic and hepatobiliary phase images (10 studies; 15 assessments) (Fig. 4). PPV values ranged from 51.9 to 99.3% (Fig. 5). The meta-analysis summary of pooled estimates of sensitivity were 77.8% (95% CI, 71.4–84.3%) for pre-contrast images; 88.1% (95% CI, 84.0–92.2%) for pre-contrast plus gadobenate-enhanced dynamic phase images alone; and 95.1% (95% CI 93.1–97.1%) for combined unenhanced, dynamic, and hepatobiliary phase images. The lack of overlap between the 95% CIs for the pooled combined assessments compared to other assessments indicates that the addition of hepatobiliary phase images significantly improves the detection of liver metastases following gadobenate administration. The pooled estimate for PPV was 90.9% (95% CI, 86.6–95.1%).
Significant (p < 0.035) heterogeneity was noted among studies. The I2 statistic was 55.8%, 68.8%, and 47.8% for unenhanced MRI, gadobenate-enhanced dynamic MRI, and combined MRI, respectively.
Discussion
Our meta-analysis showed an overall pooled sensitivity of 95.1% (95% CI 93.1%–97.1%) for the detection of liver metastases on gadobenate-enhanced MRI and a pooled PPV of 90.9% meaning that gadobenate-enhanced MRI provides a high rate of detected metastatic lesions with a low rate of FP lesions. Pooled estimates of sensitivity by subgroup (unenhanced, dynamic phase, and combined unenhanced, dynamic, and hepatobiliary phases; 77.8%, 88.1%, and 95.1%, respectively) revealed a clear benefit to the inclusion of gadobenate-enhanced hepatobiliary phase images.
The overall 95.1% sensitivity for the detection of liver metastases bears excellent agreement with sensitivities determined for gadoxetate (90.6–94.9% [15,16,17,18]) suggesting similar performances for the two hepatobiliary MR contrast agents in this application. Notably, the sensitivity for dynamic phase images alone (88.1%) bears excellent comparison with a pooled sensitivity of 73.5% reported previously for dynamic phase imaging with a purely extracellular fluid (ECF) GBCA [38] highlighting the value of gadobenate as an ECF agent in addition to a liver-specific agent. Of the 15 individual sensitivity determinations, just two series were below 91% based on evaluation of all available image sets [29, 33]. In the case of Baek et al [33], the relatively low sensitivity can be ascribed partly to the fact that hepatobiliary phase images were not acquired and partly to the relatively high proportion of patients with mucinous carcinoma. In this regard, it is known that hepatic metastasis from mucinous carcinomas may mimic benign lesions (e.g., hemangiomas or cysts) because of high signal intensity on T2-weighted images [39,40,41,42,43]. Although contrast-enhanced MRI is more reliable in showing rim enhancement, this may be very weak in the case of mucinous carcinomas resulting in misdiagnosis. Conversely, in the case of Del Frate et al [29] the relatively low sensitivity may reflect the small size of missed lesions (mean diameter 7 mm; range 5–10 mm) together with technical limitations including old MR imaging equipment, the use of a body coil and relatively poor spatial resolution (8-mm section thickness and a 20% overlap between multiple-breathhold volumes). These were deemed study limitations by the authors especially for the identification of small metastases.
As regards PPV, our value of 90.9% is not different to values obtained in previous single-center studies that used gadoxetate-enhanced MRI to detect colorectal metastatic lesions [44,45,46]. Clearly, a high PPV is fundamental for any imaging study since accurate lesion characterization is essential to avoid incorrect patient management.
A major goal of noninvasive liver imaging is to detect lesions ≤ 1 cm which may be overlooked during surgery [47, 48]. Unfortunately, subgroup analysis of lesion size was not performed in our study due to the limited data available. Among the studies included, only three [33,34,35] provided sensitivity findings for the detection of lesions ≤ 1 cm in diameter. In two of these studies [33, 35], hepatobiliary images were not acquired and results were based on the assessment of dynamic images alone. Marked differences between these two studies were noted in that whereas 27/30 (90%) small (≤ 1 cm) liver metastases from colorectal cancer were detected by Hekimoglu et al [35], a sensitivity of only 72.5% was noted by Baek et al [33], likely reflecting the more numerous mucinous tumors in the latter study. In comparison, Choi et al [34] reported a significantly (p = 0.008) higher sensitivity for the detection of small (≤ 1 cm) metastases on hepatobiliary phase images (28/31 [90.3%] lesions detected) than on pre-contrast or dynamic phase images (22/31 [70.9%] lesions detected). Of the six additional surgically confirmed metastases detected on hepatobiliary phase images, five were ≤ 1 cm in diameter.
Likewise, specificity for metastases detection could not be calculated even as a subgroup analysis due to the lack of true negative results in the majority of studies. Just two studies [33, 36] provided specificity values for gadobenate-enhanced MRI for characterization of FLLs including metastases. For dynamic phase imaging, both studies reported specificity values of ~ 95% or higher despite different assessment protocols involving separate [36] or combined [33] assessment of pre-contrast and dynamic phase images. The specificity of gadobenate-enhanced MRI obtained by Morana et al [36] for the assessment of hepatobiliary phase images alone was 87.6%. Lower specificity for the evaluation of hepatobiliary phase images alone (in the absence of unenhanced and dynamic phase images) is to be expected given the greater overlap of enhancement patterns between benign and malignant lesions on hepatobiliary images. Indeed, the hypointense appearance of lesions during the hepatobiliary phase merely reflects the lack of functioning hepatocytes, which can be observed in certain benign lesions (e.g., adenoma) as well. This emphasizes the need for combined assessment of hepatobiliary phase images together with unenhanced and dynamic phase images, as performed routinely in daily clinical practice.
The quality of studies included in our assessment was uniformly high. Based on QUADAS-2 guidelines [21] the principal methodological shortcoming was in the domain covering truth standard. However, this reflects the standard of practice in individual centers and the clinical management of individual patients. Notably, both Chen et al [15] and Vilgrain et al [16] noted similar heterogeneity in their meta-analyses of sensitivity for detection of liver metastases with gadoxetate. As in our analysis, histopathology, intraoperative observation, and/or follow-up were the reference standards. In common with our analysis, they also noted methodological shortcomings for the risk of bias, especially for patient selection and index test domains. There was no information to judge if a risk of bias in flow and timing was encountered in some studies, mainly due to a lack of information on the interval between MRI and reference standard technique. This situation is to be expected for clinical studies performed using different study designs, investigators, and assessment criteria. Our findings revealed a low concern for applicability indicating that our results with gadobenate can be extrapolated to all patients with liver metastases. To note is that the simplest way to investigate publication and other bias in meta-analyses is through visual inspection of the funnel plot of studies. The funnel plot included in our meta-analysis for the combined assessment of all available image sets shows a symmetrical distribution indicating the absence of publication bias. Moreover, the results of the modified Deeks’ test revealed that the reported sensitivities in publications were independent of the number of patients included in each study confirming the absence of publication bias (p = 0.814).
The main disadvantage of gadobenate for hepatobiliary phase imaging is the relatively long delay after acquisition of the dynamic images. Although the Summary of Product Characteristics (SPC) for gadobenate [8] recommends hepatobiliary phase acquisitions at between 40 and 120 min post-injection, it is established that the greatest diagnostic benefit is achieved at time-points between 90 and 180 min when normal liver parenchyma is more strongly enhanced [49,50,51,52]. This reflects the fact that just 3–5% of the injected dose of gadobenate is taken up by functioning hepatocytes meaning that a longer delay is required until the normal liver parenchyma is sufficiently enhanced. Therefore, patients are typically removed from the scanner after the initial dynamic acquisitions and then returned after 1–3 h for hepatobiliary phase imaging [10, 11]. Whereas this approach may be regarded as inconvenient in terms of management of patient throughput, our meta-analysis showed that the most sensitive scan for detecting liver metastases is the T1-weighted hepatobiliary acquisition obtained at 1 to 2 h post-injection. Therefore, a protocol involving injection of 0.05 mmol/kg MultiHance away from the magnet followed at 1 to 2 h post-injection by acquisition of T1-weighted hepatobiliary images together with T2-weighted sequences and DWI [53] may satisfy the imaging need for accurate detection and characterization of liver metastases. Notably, Schneider et al [54] previously demonstrated the feasibility of this approach, noting that any unclear incidental lesions detected on the T1-weighted hepatobiliary scan could be reliably characterized by means of a second 0.05 mmol/kg MultiHance injection followed by immediate acquisition of conventional dynamic images. Such a protocol, particularly if combined with conventional T2 and DWI sequences, may prove advantageous for screening patients for liver metastases and should be the subject of further study.
Our study has several limitations. Firstly both prospective and retrospective studies were included with two gadobenate doses and different imaging sequence parameters and timings. Secondly, there was heterogeneity between studies reflecting differences in reference standard. Thirdly, the studies included were performed over a period of 12 years from as far back as 2000; it is possible even better results might have been obtained today given DWI, newer MRI systems and sequences, and improved post-processing tools. Notably, Vilgrain et al [16] showed that the pooled sensitivity for detection of metastases with gadoxetate increased from 90.6% on gadoxetate-enhanced MRI alone to 95.5% with the inclusion of DWI sequences. Future studies should prospectively compare gadobenate-enhanced MRI with state-of-the-art T2/DWI for metastasis detection as well as evaluate the added benefit of combined hepatobiliary phase images and DWI. Fourthly, the lack of true negative results in the majority of studies precluded calculation of the specificity for metastases detection. Fifthly, the impact of neoadjuvant chemotherapy (NAC) on the diagnostic performance of gadobenate-enhanced MRI could not be assessed because of the lack of relevant data in the current literature. However, a previous meta-analysis showed that in the NAC setting, MRI appears to be the most appropriate imaging modality for preoperative assessment of patients with colorectal liver metastases [55, 56].
In conclusion, our meta-analysis of 10 studies with 15 independent assessments found an overall sensitivity of 95.1% (95% CI 93.1%–97.1%) and PPV of 90.9% (95% CI 86.6%–95.1%) for the detection of liver metastases with gadobenate. These data are not dissimilar to those reported for gadoxetate.
Abbreviations
- CI:
-
Confidence interval
- DWI:
-
Diffusion-weighted imaging
- FN:
-
False negative
- FP:
-
False positive
- GBCA:
-
Gadolinium-based contrast agent
- IOUS:
-
Intraoperative ultrasound
- MRI:
-
Magnetic resonance imaging
- NAC:
-
Neoadjuvant chemotherapy
- PET/CT:
-
Positron emission tomography/computerized tomography
- PPV:
-
Positive predictive value
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- QUADAS:
-
Quality assessment of diagnostic accuracy studies
- TP:
-
True positive
References
Lincke T, Zech CJ (2017) Liver metastases: detection and staging. Eur J Radiol 97:76–82
Kaur H, Hindman NM, Al-Refaie WB et al (2017) ACR Appropriateness Criteria® suspected liver metastases. J Am Coll Radiol 14(5S):S314–S325
Asato N, Tsurusaki M, Sofue K et al (2017) Comparison of gadoxetic acid-enhanced dynamic MR imaging and contrast-enhanced computed tomography for preoperative evaluation of colorectal liver metastases. Jpn J Radiol 35:197–205
Jhaveri KS, Fischer SE, Hosseini-Nik H et al (2017) Prospective comparison of gadoxetic acid-enhanced liver MRI and contrast-enhanced CT with histopathological correlation for preoperative detection of colorectal liver metastases following chemotherapy and potential impact on surgical plan. HPB (Oxford) 19:992–1000
Schulz A, Viktil E, Godt JC et al (2016) Diagnostic performance of CT, MRI and PET/CT in patients with suspected colorectal liver metastases: the superiority of MRI. Acta Radiol 57:1040–1048
Hänle MM, Thiel R, Saur G, Mason RA, Pauls S, Kratzer W (2011) Screening for liver metastases in women with mammary carcinoma: comparison of contrast-enhanced ultrasound and magnetic resonance imaging. Clin Imaging 35:366–370
Primovist European Package Insert. Available at: https://www.medicines.org.uk/emc/medicine/15927. Accessed 10 Feb 2018
MultiHance European Package Insert. Available at: www.medicines.org.uk/emc/medicine/6132. Accessed 10 Feb 2018
Morana G, Grazioli L, Testoni M, Caccia P, Procacci C (2002) Contrast agents for hepatic magnetic resonance imaging. Top Magn Reson Imaging 13:117–150
Seale MK, Catalano OA, Saini S, Hahn PF, Sahani DV (2009) Hepatobiliary-specific MR contrast agents: role in imaging the liver and biliary tree. Radiographics. 29:1725–1748
Goodwin MD, Dobson JE, Sirlin CB, Lim BG, Stella DL (2011) Diagnostic challenges and pitfalls in MR imaging with hepatocyte-specific contrast agents. Radiographics. 31:1547–1568
Feuerlein S, Gupta RT, Boll DT, Merkle EM (2012) Hepatocellular MR contrast agents: enhancement characteristics of liver parenchyma and portal vein after administration of gadoxetic acid in comparison to gadobenate dimeglumine. Eur J Radiol 81:2037–2041
Hope TA, Fowler KJ, Sirlin CB et al (2015) Hepatobiliary agents and their role in LI-RADS. Abdom Imaging 40:613–625
MultiHance U.S. Package Insert. Available at: www.accessdata.fda.gov/drugsatfda_docs/label/2018/021357s014,021358s013lbl.pdf. Accessed 10 Feb 2018
Chen L, Zhang J, Zhang L et al (2012) Meta-analysis of gadoxetic acid disodium (Gd-EOB-DTPA)-enhanced magnetic resonance imaging for the detection of liver metastases. PLoS One 7:e48681
Vilgrain V, Esvan M, Ronot M, Caumont-Prim A, Aubé C, Chatellier G (2016) A meta-analysis of diffusion-weighted and gadoxetic acid-enhanced MR imaging for the detection of liver metastases. Eur Radiol 26:4595–4515
Vreugdenburg TD, Ma N, Duncan JK, Riitano D, Cameron AL, Maddern GJ (2016) Comparative diagnostic accuracy of hepatocyte-specific gadoxetic acid (Gd-EOB-DTPA) enhanced MR imaging and contrast enhanced CT for the detection of liver metastases: a systematic review and meta-analysis. Int J Colorectal Dis 31:1739–1749
Choi SH, Kim SY, Park SH et al (2018) Diagnostic performance of CT, gadoxetate disodium-enhanced MRI, and PET/CT for the diagnosis of colorectal liver metastasis: systematic review and meta-analysis. J Magn Reson Imaging 47:1237–1250
Neri E, Bali MA, Ba-Ssalamah A et al (2016) ESGAR consensus statement on liver MR imaging and clinical use of liver-specific contrast agents. Eur Radiol 26:921–931
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F (2000) Methods for meta-analysis in medical research. Wiley, New York
Borenstein M, Hedges LV, Higgins JPT, Rothstein H (2009) Introduction to meta-analysis, 1st edn. Wiley, West Sussex
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analysis. BMJ. 327(7414):557–560
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
van Enst WA, Ochodo E, Scholten RJ, Hooft L, Leeflang MM (2014) Investigation of publication bias in meta-analysis of diagnostic test accuracy: a meta-epidemiological study. BMC Med Res Methodol 14:70
Pirovano G, Vanzulli A, Marti-Bonmati L et al (2000) Evaluation of the accuracy of gadobenate dimeglumine-enhanced MR imaging in the detection and characterization of focal liver lesions. AJR Am J Roentgenol 175:1111–1120
del Frate C, Bazzocchi M, Mortele KJ et al (2002) Detection of liver metastases: comparison of gadobenate dimeglumine-enhanced and ferumoxides-enhanced MR imaging examinations. Radiology. 225:766–772
Kim YK, Lee JM, Kim CS (2004) Gadobenate dimeglumine-enhanced liver MR imaging: value of dynamic and delayed imaging for the characterization and detection of focal liver lesions. Eur Radiol 14:5–13
Kim YK, Lee JM, Kim CS, Chung GH, Kim CY, Kim IH (2005) Detection of liver metastases: gadobenate dimeglumine-enhanced three-dimensional dynamic phases and one-hour delayed phase MR imaging versus superparamagnetic iron oxide-enhanced MR imaging. Eur Radiol 15:220–228
Lee HY, Lee JM, Kim SH et al (2008) Detection and characterization of focal hepatic lesions: comparative study of MDCT and gadobenate dimeglumine-enhanced MR imaging. Clin Imaging 32:287–295
Baek SE, Park MS, Hong HS et al (2010) Characterisation of small hypoattenuating hepatic lesions in multi-detector CT (MDCT) in patients with underlying extrahepatic malignancy: added value of contrast-enhanced MR images. Eur Radiol 20:2853–2861
Choi JY, Choi JS, Kim MJ et al (2010) Detection of hepatic hypovascular metastases: 3D gradient echo MRI using a hepatobiliary contrast agent. J Magn Reson Imaging 31:571–578
Hekimoglu K, Ustundag Y, Dusak A et al (2011) Small colorectal liver metastases: detection with SPIO-enhanced MRI in comparison with gadobenate dimeglumine-enhanced MRI and CT imaging. Eur J Radiol 77:468–472
Morana G, Grazioli L, Kirchin MA et al (2011) Solid hypervascular liver lesions: accurate identification of true benign lesions on enhanced dynamic and hepatobiliary phase magnetic resonance imaging after gadobenate dimeglumine administration. Invest Radiol 46:225–239
Brismar TB, Kartalis N, Kylander C, Albiin N (2012) MRI of colorectal cancer liver metastases: comparison of orally administered manganese with intravenously administered gadobenate dimeglumine. Eur Radiol 22:633–641
Hardie AD, Naik M, Hecht EM et al (2010) Diagnosis of liver metastases: value of diffusion-weighted MRI compared with gadolinium-enhanced MRI. Eur Radiol 20:1431–1441
Ueda K, Matsui O, Nobata K, Takashima T (1996) Mucinous carcinoma of the liver mimicking cavernous hemangioma on pre- and postcontrast MR imaging. AJR Am J Roentgenol 166:468–469
Kanematsu M, Kondo H, Goshima S et al (2006) Imaging liver metastases: review and update. Eur J Radiol 58:217–228
Lacout A, El Hajjam M, Julie C, Lacombe P, Pelage JP (2008) Liver metastasis of a mucinous colonic carcinoma mimicking a haemangioma in T2-weighted sequences. J Med Imaging Radiat Oncol 52:580–582
McFarland EG, Mayo-Smith WW, Saini S, Hahn PF, Goldberg MA, Lee MJ (1994) Hepatic hemangiomas and malignant tumors: improved differentiation with heavily T2-weighted conventional spin-echo MR imaging. Radiology 193:43–47
Ito K, Mitchell D, Outwater E, Szklaruk J, Sadek A (1997) Hepatic lesions: discrimination of nonsolid, benign lesions from solid, malignant lesions with heavily T2-weighted fast spin-echo MR imaging. Radiology 204:729–737
Scharitzer M, Ba-Ssalamah A, Ringl H et al (2013) Preoperative evaluation of colorectal liver metastases: comparison between gadoxetic acid-enhanced 3.0-T MRI and contrast-enhanced MDCT with histopathological correlation. Eur Radiol 23:2187–2196
Berger-Kulemann V, Schima W, Baroud S et al (2012) Gadoxetic acid-enhanced 3.0 T MR imaging versus multidetector-row CT in the detection of colorectal metastases in fatty liver using intraoperative ultrasound and histopathology as a standard of reference. Eur J Surg Oncol 38:670–676
Sofue K, Tsurusaki M, Tokue H, Arai Y, Sugimura K (2011) Gd-EOB-DTPA-enhanced 3.0 T MR imaging: quantitative and qualitative comparison of hepatocyte-phase images obtained 10 min and 20 min after injection for the detection of liver metastases from colorectal carcinoma. Eur Radiol 21:2336–2343
Nordlinger B, Sorbye H, Glimelius B et al (2008) Perioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC intergroup trial 40983): a randomised controlled trial. Lancet 371:1007–1016
Goéré D, Elias D (2008) Resection of liver metastases from noncolorectal non-endocrine primary tumours. Eur J Surg Oncol 34:281–288
Grazioli L, Morana G, Caudana R et al (2000) Hepatocellular carcinoma: correlation between gadobenate dimeglumine-enhanced MRI and pathologic findings. Invest Radiol 35:25–34
Grazioli L, Morana G, Federle MP et al (2001) Focal nodular hyperplasia: morphologic and functional information from MR imaging with gadobenate dimeglumine. Radiology. 221:731–739
Grazioli L, Morana G, Kirchin MA, Schneider G (2005) Accurate differentiation of focal nodular hyperplasia from hepatic adenoma at gadobenate dimeglumine-enhanced MR imaging: prospective study. Radiology. 236:166–177
Fu GL, Du Y, Zee CS et al (2012) Gadobenate dimeglumine-enhanced liver magnetic resonance imaging: value of hepatobiliary phase for the detection of focal liver lesions. J Comput Assist Tomogr 36:14–19
Mürtz P, Sprinkart AM, Reick M et al (2018) Accurate IVIM model-based liver lesion characterisation can be achieved with only three b-value DWI. Eur Radiol 28(10):4418–4428
Schneider G, Altmeyer K, Kirchin MA et al (2007) Evaluation of a novel time-efficient protocol for gadobenate dimeglumine (Gd-BOPTA)-enhanced liver magnetic resonance imaging. Invest Radiol 42:105–115
Sivesgaard K, Larsen LP, Sørensen M et al (2018) Diagnostic accuracy of CE-CT, MRI and FDG PET/CT for detecting colorectal cancer liver metastases in patients considered eligible for hepatic resection and/or local ablation. Eur Radiol. https://doi.org/10.1007/s00330-018-5469-0
van Kessel CS, Buckens CF, van den Bosch MA, van Leeuwen MS, van Hillegersberg R, Verkooijen HM (2012) Preoperative imaging of colorectal liver metastases after neoadjuvant chemotherapy: a meta-analysis. Ann Surg Oncol 19:2805–2813
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hongyan Chen.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because it is a meta-analysis on published literature.
Ethical approval
Institutional Review Board approval was not required because it is a meta-analysis on published literature.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, L., Yu, X., Huo, L. et al. Detection of liver metastases on gadobenate dimeglumine-enhanced MRI: systematic review, meta-analysis, and similarities with gadoxetate-enhanced MRI. Eur Radiol 29, 5205–5216 (2019). https://doi.org/10.1007/s00330-019-06110-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06110-1