Abstract
Purpose
To determine the feasibility of a prototype device combining 3D-automated breast ultrasound (ABVS) and digital breast tomosynthesis in a single device to detect and characterize breast lesions.
Methods
In this prospective feasibility study, the FUSION-X-US prototype was used to perform digital breast tomosynthesis and ABVS in 23 patients with an indication for tomosynthesis based on current guidelines after clinical examination and standard imaging. The ABVS and tomosynthesis images of the prototype were interpreted separately by two blinded experts. The study compares the detection and BI-RADS® scores of breast lesions using only the tomosynthesis and ABVS data from the FUSION-X-US prototype to the results of the complete diagnostic workup.
Results
Image acquisition and processing by the prototype was fast and accurate, with some limitations in ultrasound coverage and image quality. In the diagnostic workup, 29 solid lesions (23 benign, including three cases with microcalcifications, and six malignant lesions) were identified. Using the prototype, all malignant lesions were detected and classified as malignant or suspicious by both investigators.
Conclusion
Solid breast lesions can be localized accurately and fast by the Fusion-X-US system. Technical improvements of the ultrasound image quality and ultrasound coverage are needed to further study this new device.
Key Points
-
The prototype combines tomosynthesis and automated 3D-ultrasound (ABVS) in one device.
-
It allows accurate detection of malignant lesions, directly correlating tomosynthesis and ABVS data.
-
The diagnostic evaluation of the prototype-acquired data was interpreter-independent.
-
The prototype provides a time-efficient and technically reliable diagnostic procedure.
-
The combination of tomosynthesis and ABVS is a promising diagnostic approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mammography is the main pillar of breast cancer screening programs, leading to improved treatment options and reduced mortality [1,2,3], but sensitivity is reduced in populations with dense breast tissue [4, 5]. Performing a supplemental breast ultrasound in women with BI-RADS® density C or D breast tissue detects an additional approximately 3.5/1000 malignancies occult to mammography [6,7,8].
Both mammography and ultrasound have undergone continued development in the last few years. Tomosynthesis, a 3D-procedure using low-dose digital x-ray projections, increases sensitivity and specificity of breast cancer detection compared to 2D-mammography [9,10,11,12]. Automated 3D-ultrasound imaging of the whole breast (ABVS) has the potential to overcome the examiner-dependency of hand-held ultrasound (HHUS) and to reduce the time of examination and interpretation [13,14,15,16,17]. Both techniques have been shown to potentially improve breast cancer screening in select populations such as women with dense breast tissue ([18,19,20,21]. However, few reports have been published on the combination of ultrasound and mammography in a single system [22,23,24,25]. The aim of this study was to evaluate the diagnostic utility of the FUSION-X-US prototype combining tomosynthesis and ABVS in one device for the detection and classification of breast lesions.
Material and methods
The study protocol was approved by the local ethics committee (Medical Faculty Heidelberg, reference number S-074/2015), and was compliant with the Health Information Portability and Accountability Act of 1996 (HIPAA), with written informed consent from every patient enrolled in the study.
Equipment
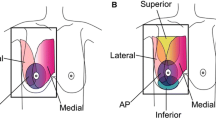
The X-US-prototype is based on the ACUSON S2000 ABVS and the Mammomat Inspiration (Siemens Healthcare GmbH, Erlangen, Germany), which are both approved by the US Food and Drug Administration (FDA). The 14-MHz high-frequency linear ultrasound transducer is integrated into a compression device and can be automatically moved over the breast surface, covering a volume of up to 30 x 15 x 6 cm3 in a single scan. The contact area is a gauze, providing good ultrasound coupling and less x-ray absorption compared to a normal mammography compression plate. After standard breast positioning in mediolateral (ML), mediolateral-oblique (MLO) or craniocaudal (CC) orientation, standard compression is applied by lowering the compression device for 3D-mammographic imaging. Then, coupling lotion is spread on the gauze and the automated ultrasound is performed. The patient´s position is not changed between tomosynthesis and ABVS, so both examinations are performed in the same projection. The data are processed in a separate computer and the DICOM-Header is updated to add the correct 3D-image position, so the regions of interest can be analysed side-by-side in the corresponding set of images (see Figs. 1, 2 and 3).
Schematic view of the X-US prototype. An ultrasound transducer is included into a prototype compression plate of a standard MAMMOMAT Inspiration. During normal x-ray imaging (mammography or tomosynthesis) the transducer is parked outside the x-ray field at the edge of the compression plate. Right after acquisition of the x-ray images, the transducer moves automatically from right to left to perform the ultrasound scan
The prototype used in this study is a research device and is not commercially available.
Study design
The study was performed between November and December 2015 with patients referred to the breast unit for radiological examination of breast lesions. Patients were eligible for the study if they were female, at least 18 years old, and presented for a diagnostic work-up of previous radiological findings that led to the indication for tomosynthesis for additional diagnostic work-up. Pregnancy and inability to give informed consent were exclusion criteria. Patients were recruited non-selectively, depending on the availability of the prototype device and the trained staff. All patients in the study received the standard diagnostic workup consisting of physician-performed clinical examination, 2D-digital mammography (Mammomat Inspiration, Siemens Healthcare GmbH, Erlangen, Germany) and hand-held 2D-ultrasound using an ACUSON S2000 or S3000 ultrasound unit (Siemens Medical Solutions, Mountain View, CA, USA) using an 18-MHz transducer. Tomosynthesis and ABVS were obtained at the same setting using the FUSION-X-US prototype. Mammography was performed in more than one projection (usually two or three projections: craniocaudal (CC), mediolateral-oblique (MLO), mediolateral (ML)), depending on the position of the tumour and the form of the breast. Tomosynthesis was performed in one projection in addition to mammography, and subsequently ABVS-scan was performed in the same orientation. The projection chosen for tomosynthesis and ABVS depended on the clinical situation. In total, two cases were scanned in MLO orientation and 21 cases were scanned in ML view. In nine cases with suspicious imaging findings, a sonographically-guided biopsy for a histopathological workup according to current guidelines was performed [26]. The final result of the entire diagnostic workup was defined as the index reference. Since a histopathological examination (biopsy) was performed in cases with unclear imaging findings, we regarded the result of the standard workup as gold standard.
Besides being used for the diagnostic workup, tomosynthesis and ABVS images were also evaluated separately by two independent, experienced physicians both with 9 years of experience with ABVS and 6 years with tomosynthesis. The investigators were blinded to the results of the standard workup. Firstly, the blinded images from tomosynthesis were presented to the investigators. Then, the corresponding blinded ABVS images were shown in second window for a side-by-side view of tomosynthesis and ABVS images. By this two-step-approach, we aimed to evaluate the additional benefit of the side-by-side evaluation (tomosynthesis and ABVS) over the ‘standard’ interpretation of tomosynthesis images alone. Lesions were classified according to BI-RADS®, version 5 [27]. The investigators were allowed to provide a free-text comment on their classification. The area of the breast covered in ABVS was compared to the coverage in tomosynthesis by measuring the largest extension of the breast in each imaging modality. Localization and size of the lesions described in the reports of the diagnostic workup were matched with the findings described by the investigators in the study setting.
The main outcome measure was the detection rate of malignant lesions for both investigators using the FUSION-X-US prototype. Secondary outcome measures were the detection rate of benign lesions, the time for the interpretation of the images and the coverage of the breast surface in ABVS and tomosynthesis by the prototype.
Statistical analysis
This was an explorative study based on purely descriptive statistics. Resulting p-values are not adjusted for multiplicity and must be interpreted descriptively. The duration of the interpretation of the images by both investigators and the difference in the coverage of the breast in tomosynthesis and ABVS were tested for significance using the paired t-test (software: Graph Pad Prism, Version 5, 2007, Graph Pad Software Inc., La Jolla, CA, USA). The primary endpoint (detection rate of malignant lesions using the prototype) was analysed descriptively (case-by-case) and by reporting simple summary measures. Due to the low number of cases within the investigated subpopulations, common asymptotic confidence intervals for the observed rates are not reasonable and thus not reported.
Results
During the study period, 495 tomosyntheses were performed. Twenty-three patients were screened for the study. They all fulfilled the inclusion criteria and were recruited. The patients´ ages ranged from 30 to 79 years (mean: 53.6 years). Breast density ranged from ACR A to D, with most breasts (15/23, 65.2 %) being ACR B (see Supplementary Table 1: Cohort description). In the routine workup, 29 lesions (23 benign lesions, including three with microcalcifications, and six malignant lesions) were found.
Technically, the prototype worked reliably and the scanning process took 25 s for the tomosynthesis scan and 80 s for ABVS. Tomosynthesis and ABVS slices were correctly correlated by the software in all cases. The mean duration for interpretation of the tomosynthesis was 122.7 s (SD 95.7 s; investigator 1), and 151.3 s (SD 55.3 sec; investigator 2), respectively. For the interpretation of ABVS, the mean duration was 149.4 s (SD 69.6 s) and 141.2 s (SD 44.1 s), respectively. The mean duration did not differ significantly between the two investigators for tomosynthesis (p=0.221) or ABVS (p=0.638; Fig. 4).
The coverage of the breast differed between tomosynthesis and ABVS. The average area of the breast covered in ABVS (99.7 cm2, SD 25.4) was significantly smaller than in tomosynthesis (150.3 cm2; SD 37.9; p<0.001).
In the standard workup, the classification of malignant lesions did not differ between HHUS and mammography except for one case (mammography BIRADS 4, sonography BIRADS 5). In the study setting, all six malignant lesions were identified by both investigators in tomosynthesis (Table 1). However, only in a few cases (3/6, 50.0 %, investigator 1; 4/6, 66.6 %, investigator 2) the lesion was also seen in ABVS. Most benign lesions were correctly identified by both investigators in ABVS (investigator 1: 78.3 % [18/23], investigator 2: 82.6 % [19/23]). Investigator 1 identified 47.8 % (11/23), and investigator 2 identified 34.8 % (8/23) of the lesions in both tomosynthesis and ABVS. All three cases containing microcalcifications (benign) were identified by investigator 1 (3/3, 100.0 %) in tomosynthesis, while one case was missed by investigator 2 (2/3, 66.6 %). No lesion was detected only in ABVS (0/29, 0.0%).
All malignant lesions (6/6, 100.0%) were classified as either unclear (BI-RADS® 0), potentially malignant (BI-RADS® 4a-c) or highly suspicious (BI-RADS® 5, Table 2), so no malignant lesion was missed in the prototype setting. In two cases (2/6, 33.3 %), the area of interest with the tomosynthesis finding was not covered by ABVS, so no corresponding lesion was described in ABVS (BI-RADS® 1). In case number 3, a malignant lesion was not described in ABVS, although the area of interest was covered in ABVS.
Investigator 1 correctly classified 11 benign lesions (11/23, 47.8 %) in tomosynthesis and nine lesions (9/23, 39.1 %) in ABVS as BI-RADS® 2 (Supplementary Table 2). In seven cases (7/23, 30.4 %), both ABVS and tomosynthesis resulted in a BI-RADS® 2 classification. In the remaining cases, lesions were classified as BI-RADS® 0. In two cases, investigator 1 noted a free-text comment, explaining that he classified the lesions as BI-RADS® 0 due to lack of information on the clinical history of the patient, and that if he had been given the information that the patients had been operated on the breast, he would have classified their lesion as a scar (BI-RADS 2), otherwise as likely malignant (BI-RADS 4c).
Investigator 2 correctly classified eight lesions (8/23, 34.8 %) in tomosynthesis and six lesions (6/23, 26.1 %) in ABVS as benign (BI-RADS® 2). In two cases (2/23, 8.7%), both ABVS and tomosynthesis resulted in a BI-RADS® 2 classification.
In six cases (2/23, 8.7 % [investigator 1], 4/23, 17.4 % [investigator 2]), a lesion that was classified as unclear or suspicious (BI-RADS® 0, 4b or 5) in tomosynthesis, the ABVS classification was BI-RADS® 2. In contrast, two lesions (2/23, 8.7 % [investigator 2]) that were BI-RADS® 2 in tomosynthesis were falsely classified as suspicious (BI-RADS® 0, respectively BI-RADS® 4a) in ABVS. Thus, two correct tomosynthesis results (2/23, 8.7 %) were falsely questioned by ABVS.
Figure 5 depicts a screenshot of one of the cases in which the ABVS image led to the correct identification of a benign lesion as a fibroadenoma (BI-RADS® 2), which had been classified as suspicious (BI-RADS® 4b) in tomosynthesis.
Screenshots showing a benign solid lesion on corresponding images of tomosynthesis in mediolateral orientation (upper left), 3D-automated breast volume sonography (ABVS) reconstruction (upper right-hand side) and 2D-ABVS ultrasound image (note: the bottom of the image is oriented towards the ultrasound transducer)
Discussion
The FUSION-X-US prototype was designed to combine the advantages of tomosynthesis and ABVS in a single device, allowing both imaging procedures to be performed in one workflow. The potential benefits include a reduction in the duration of the examination, the possibility to directly correlate the localization of findings from both imaging modalities and to improve the detection rate of malignant lesions compared to the standard mammographic breast cancer screening. Since the ultrasound scanning process is fully automatic, a higher interobserver reliability is expected than for HHUS [15].
In our study, the total scanning time was 105 s (25 s for tomosynthesis and 80 s for ABVS) and the time for interpretation of both images was less than 5 min for both investigators, with no significant difference. Thus, even tomosynthesis and ABVS together are faster than HHUS alone (with a reported median duration of 9 min per breast [8]). Interobserver reliability was high, since all malignant lesions were found by both investigators.
For the scanning process, no change of position of the patient was necessary, which was more convenient for the patient and allowed the images of tomosynthesis and ABVS to be directly correlated.
This study was powered as a descriptive feasibility study showing the technical reliability and the possibility of a user-independent workflow using side-by-side review of tomosynthesis and ABVS images. Our analysis did not show any clear benefit of the additional ABVS scan. This study identified some ultrasound technical problems (discussed below) that can be resolved with some modifications. Further studies with these modifications are needed to determine the true impact of this system. A larger study with higher case numbers is needed to confirm the diagnostic utility.
The proportion of patients with malignant lesions (six out of 23) is high, not due to a selection process during recruitment but due to the fact that only patients with an indication for tomosynthesis were included. This implies that most patients had radiological findings requiring further diagnostic workup. Based on this collective, we recruited patients non-selectively. All patients meeting the inclusion criteria were recruited for the study, if the prototype was available during the time of their visit. Therefore, the inclusion criteria (indication for tomosynthesis) led to an enrichment of malignant lesions in the patient cohort.
There were some technical limitations in the use of the prototype: On average, only 66.0 % of the area covered by tomosynthesis was covered by ABVS, so not all regions of interest could be examined in both modalities. This might explain why some of the lesions were only seen in tomosynthesis and not in ABVS. One reason for the limited coverage of ABVS is the fact that the ultrasound transducer was not optimized for this study setup. The active area of the transducer is embedded into a static metal housing with a thickness of 1 cm on both the anterior and posterior sides, leading to a loss of tissue coverage of 1 cm multiplied by the length of the breast in scanning direction and an additional loss of 0.5 cm at the lateral or medial side of the compression plate. Further investigations to use beam steering and customized ultrasound transducers with a thinner housing should help to overcome this challenge.
According to the developers, ultrasound coverage and ultrasound image quality will be increased in the next prototype based on the clinical results presented in this study. Likely, this will also lead to an improved detection rate.
The relatively high proportion of lesions (both malignant and benign) classified as unclear (BI-RADS 0) remains a critical aspect. Among the six malignant lesions, investigator 1 classified three lesions in tomosynthesis and two lesions in ABVS as BI-RADS 0. However, the study setting was very different from the clinical situation: With more information, including the patient history, which was not provided in this study setting, the investigators would likely have classified more lesions unambiguously.
Image quality of the prototype device was lower than in a stand-alone ABVS system, potentially contributing to the high rate of BI-RADS® 0 cases in ABVS. The software for the ultrasound measurements was optimized for standard ABVS measurements and not for the special setting of the prototype, resulting in suboptimal image quality. In future studies, a parameter optimization for the ultrasound imaging should be performed by taking into account breast compression and individual breast thickness.
In summary, the FUSION-X-US prototype allows digital tomosynthesis and ABVS images to be obtained in one workflow using a single device for the detection and characterization of breast lesions. To evaluate the diagnostic accuracy of the device and a potential benefit of ABVS as supplemental imaging to tomosynthesis for the detection of malignant lesions, further studies with a larger number of patients are needed. Technically, image quality (ABVS) and coverage of the breast need to be improved.
Abbreviations
- ABVS:
-
Automated breast volume sonography
- BI-RADS:
-
Breast Imaging-Reporting and Data System
- CC:
-
Craniocaudal
- FDA:
-
Food and Drug Administration
- HHUS:
-
Hand-held ultrasound
- HIPAA:
-
Health Information Portability and Accountability Act of 1996 (HIPAA)
- ML:
-
Mediolateral
- MLO:
-
Mediolateral-oblique
- SD:
-
Standard deviation
References
Gotzsche PC, Jorgensen KJ (2013) Screening for breast cancer with mammography. Cochrane Database Syst Rev Jun 4;:CD001877
Kerlikowske K (1997) Efficacy of screening mammography among women aged 40 to 49 years and 50 to 69 years: Comparison of relative and absolute benefit. J Natl Cancer Inst Monogr 1997:79–86
Nystrom L, Rutqvist LE, Wall S et al (1993) Breast cancer screening with mammography: Overview of Swedish randomised trials. Lancet 341:973–978
Carney PA, Miglioretti DL, Yankaskas BC et al (2003) Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med 138:168–175
Buist DSM, Porter PL, Lehman C, Taplin SH, White E (2004) Factors contributing to mammography failure in women aged 40-49 years. J Natl Cancer Inst 96:1432–1440
Kolb TM, Lichy J, Newhouse JH (1998) Occult cancer in women with dense breasts: Detection with screening US--diagnostic yield and tumor characteristics. Radiology 207:191–199
Kolb TM, Lichy J, Newhouse JH (2002) Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: An analysis of 27,825 patient evaluations. Radiology 225:165–175
Berg WA, Blume JD, Cormack JB et al (2008) Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 299:2151–2163
Alakhras M, Bourne R, Rickard M, Ng KH, Pietrzyk M, Brennan PC (2013) Digital tomosynthesis: A new future for breast imaging? Clinical radiology 68:e225–e236
Houssami N, Zackrisson S (2013) Digital breast tomosynthesis: The future of mammography screening or much ado about nothing? Expert Rev Med Devices 10:583–585
Skaane P (2017) Breast cancer screening with digital breast tomosynthesis. Breast cancer 24:32–41
Patterson SK, Roubidoux MA (2014) Update on new technologies in digital mammography. Int J Womens Health 6:781–788
Giger ML, Inciardi MF, Edwards A et al (2016) Automated Breast Ultrasound in Breast Cancer Screening of Women With Dense Breasts: Reader Study of Mammography-Negative and Mammography-Positive Cancers. AJR 206:1341–1350
Halshtok-Neiman O, Shalmon A, Rundstein A, Servadio Y, Gotleib M, Sklair-Levy M (2015) Use of Automated Breast Volumetric Sonography as a Second-Look Tool for Findings in Breast Magnetic Resonance Imaging. Isr Med Assoc J 17:410–413
Golatta M, Franz D, Harcos A et al (2013) Interobserver reliability of automated breast volume scanner (ABVS) interpretation and agreement of ABVS findings with hand held breast ultrasound (HHUS), mammography and pathology results. Eur J Rad 82:e332-e336.
Golatta M, Baggs C, Schweitzer-Martin M et al (2015) Evaluation of an automated breast 3D-ultrasound system by comparing it with hand-held ultrasound (HHUS) and mammography. Arch Gynecol Obstet 291:889–895
Vourtsis A, Kachulis A (2017) The performance of 3D ABUS versus HHUS in the visualisation and BI-RADS characterisation of breast lesions in a large cohort of 1,886 women. Eur Radiol. https://doi.org/10.1007/s00330-017-5011-9
Ciatto S, Houssami N, Bernardi D et al (2013) Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): A prospective comparison study. Lancet Oncol 14:583–589
Skaane P, Bandos AI, Gullien R et al (2013) Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology 267:47–56
Wojcinski S, Gyapong S, Farrokh A, Soergel P, Hillemanns P, Degenhardt F (2013) Diagnostic performance and inter-observer concordance in lesion detection with the automated breast volume scanner (ABVS). BMC Med Imaging 13:36
Wilczek B, Wilczek HE, Rasouliyan L, Leifland K (2016) Adding 3D automated breast ultrasound to mammography screening in women with heterogeneously and extremely dense breasts: Report from a hospital-based, high-volume, single-center breast cancer screening program. Eur J Radiol 85:1554–1563
Kapur A, Carson PL, Eberhard J et al (2004) Combination of digital mammography with semi-automated 3D breast ultrasound. Technol Cancer Res Treat 3:325–334
Padilla F, Roubidoux MA, Paramagul C et al (2013) Breast mass characterization using 3-dimensional automated ultrasound as an adjunct to digital breast tomosynthesis: a pilot study. J Ultrasound Med 32:93–104
Richter K, Winzer KJ, Frohberg HD et al (1998) Combination of mammography with automated ultrasound (Sono-X) in routine diagnosis? Zentralbl Chir 123:37–41
Sinha SP, Roubidoux MA, Helvie MA et al. (2007) IEEE Engineering in Medicine and Biology Society Annual Conference. 2007:1335–8
Wockel A, Kreienberg R (2008) First Revision of the German S3 Guideline 'Diagnosis, Therapy, and Follow-Up of Breast Cancer'. Breast Care (Basel) 3:82–86
Sickles EA, D’Orsi CJ, Bassett LW, et al (2013) ACR BI-RADS mammography. In: D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA, (ed) Breast Imaging Reporting and Data System: ACR BI-RADS—breast imaging atlas. 5th edn. Reston, VA. J Am Coll Radiol 272(2):309–315
Funding
This study has received funding by Siemens Health Care GmbH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is PD Dr. Michael Golatta.
Conflict of interest
The prototype was provided by Siemens Healthcare GmbH. M. Radicke was the contact person for technical lead. Siemens did not have any influence on the results or evaluation of the study.
M. Golatta received payment for lectures from Siemens Ultrasound. R. Barr has equipment grants from Siemens ultrasound, Philips Ultrasound, B and K Ultrasound, and Hitachi-Aloka. He is on the speakers bureau for Philips Ultrasound and Bracoo Diagnostics. He is on the advisory panels of Bracco Diagnostics and Lantheus Medical. He receives royalties from Thieme Publishers.
Statistics and biometry
Prof. Geraldine Rauch kindly provided statistical advice for this manuscript, she has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic
• performed at one institution
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Schaefgen, B., Heil, J., Barr, R.G. et al. Initial results of the FUSION-X-US prototype combining 3D automated breast ultrasound and digital breast tomosynthesis. Eur Radiol 28, 2499–2506 (2018). https://doi.org/10.1007/s00330-017-5235-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5235-8