Abstract
Objectives
To evaluate the image quality and lesion conspicuity of virtual-monochromatic-imaging (VMI) with dual-layer DECT (DL-DECT) for reduced-iodine-load multiphasic-hepatic CT.
Methods
Forty-five adults with renal dysfunction who had undergone hepatic DL-DECT with 300-mgI/kg were included. VMI (40–70-keV, DL-DECT-VMI) was generated at each enhancement phase. As controls, 45 matched patients undergoing standard 120-kVp protocol (120-kVp, 600-mgI/kg, and iterative reconstruction) were included. We compared the size-specific dose estimate (SSDE), image noise, CT attenuation, and contrast-to-noise ratio (CNR) between protocols. Two radiologists scored the image quality and lesion conspicuity.
Results
SSDE was significantly lower in DL-DECT group (p < 0.01). Image noise of DL-DECT-VMI was almost constant at each keV (differences of ≤15%) and equivalent to or lower than of 120-kVp. As the energy decreased, CT attenuation and CNR gradually increased; the values of 55-60 keV images were almost equivalent to those of standard 120-kVp. The highest scores for overall quality and lesion conspicuity were assigned at 40-keV followed by 45 to 55-keV, all of which were similar to or better than of 120-kVp.
Conclusions
For multiphasic-hepatic CT with 50% iodine-load, DL-DECT-VMI at 40- to 55-keV provides equivalent or better image quality and lesion conspicuity without increasing radiation dose compared with standard 120-kVp protocol.
Key Points
• 40-55-keV yields optimal image quality for half-iodine-load multiphasic-hepatic CT with DL-DECT.
• DL-DECT protocol decreases radiation exposure compared with 120-kVp scans with iterative reconstruction.
• 40-keV images maximise conspicuity of hepatocellular carcinoma especially at hepatic-arterial phase.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multiphasic hepatic computed tomography (CT) plays an important role in the diagnosis, follow-up, and post-treatment surveillance of hepatic diseases, but it requires administration of a relatively large amount of iodinated contrast medium (CM) for appropriate detection and characterisation [1, 2]. Although the causal relationship between administration of intravenous CM and acute kidney injury is controversial [3], the minimisation of iodine load without loss of image quality may still be desirable for patients with hepatic diseases such as chronic hepatitis, cirrhosis, or malignant tumours, because these are associated with multiple risk factors for the development of kidney injury [4,5,6,7].
Low tube voltage (kVp) scanning is a well-established technique for reducing the iodine dose, because the iodine attenuation increases as the mean X-ray spectra is closer to the iodine k-edge (33-keV). Although the image noise increases because of reduced X-ray photons, a compensatory increase in the tube current and use of iterative reconstruction (IR) instead of filtered-back projection can suppress the high quantum mottle. The utility of these techniques has been demonstrated primarily in CT angiography (CTA) [8], but also in multiphasic hepatic CT [9]. As a matter of course, however, this approach does not allow for retrospective optimisation of the iodine contrast according to the demand of each examination and each organ of interest once the image acquisitions are completed.
Dual-energy CT (DECT) can provide reconstruction of virtual monochromatic imaging (VMI) at arbitrary X-ray energies (keV), based on the two different energy datasets. By taking advantage of the greater iodine contrast in lower energy images [10,11,12], a few investigators have suggested the utility of VMI generated from tube-based DECT systems for the reduction of iodine load in CT angiography (CTA) [13,14,15]. However, for multiphasic hepatic CT, this strategy has not been fully established, probably because the increased noise at low keV images and inherent decline in contrast due to the reduced iodine load degrade low-contrast lesion detectability and subjective image quality [16,17,18,19,20,21,22]. Although increasing the tube current can compensate for the image noise, the radiation exposure is of concern, as hepatic CT usually requires multiphase acquisitions for the accurate lesion assessment.
Recently, a dual-layer DECT (DL-DECT) has become commercially available [23,24,25]. This system simultaneously measures high- and low-energy projection data in the two detector layers, at the exact same spatial and angular location. This allows the VMI reconstruction in the projection domain, without the need for temporal and angular interpolation, which may theoretically yield an accurate beam-hardening correction and the cancelation of anti-correlated noise in photoelectric and Compton scatter images [26,27,28,29]. Additionally, DL-DECT allows the implementation of dedicated model-based IR techniques, leading to a further reduction in image noise [30]. Therefore, we hypothesised that low energy VMI with DL-DECT may not only improve image quality and lesion conspicuity, it may also allow a substantial decrease in the iodine load of multiphasic hepatic CT, without increasing radiation exposure in comparison with standard 120-kVp acquisitions.
In the present study, we aimed to evaluate the image quality and lesion conspicuity of multiphasic hepatic CT performed on DL-DECT with a 50% iodine load, and to define the optimal monoenergetic levels by comparisons with polychromatic 120-kVp acquisitions with a full iodine load and iterative reconstruction.
Materials and methods
This retrospective study received the approval of our institutional review board, and the requirement for written informed consent was waived.
Patients
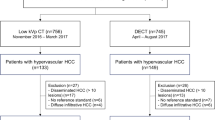
We identified 45 consecutive adults with renal dysfunction (estimated glomerular filtrating ratio [eGFR] < 60 mL/min/1.73 m2) who had undergone multiphasic hepatic CT on DL-DECT (IQon spectral CT; Philips healthcare, Best, The Netherlands) for the suspicion, diagnosis or follow up of hepatic tumours between December 2016 and February 2017 (DL-DECT group). All acquisitions were performed with a 50% reduced iodine load, which in our institution is a standard of care for patients with renal dysfunction. We also identified 866 adults who had undergone conventional 120-kVp protocol for the same clinical indications as the DL-DECT group between January and November 2016. They were scanned on a single-energy MDCT (Brilliance 64; Philips Healthcare), which was implemented at our institution before the introduction of DL-DECT. From these, we retrieved patients matched for body mass index (BMI; a maximum difference of 10% was accepted), age, and sex with the DL-DECT group. When multiple relevant cases were identified for a single DL-DECT patient, the patient whose body weight (BW) was closest to the corresponding DL-DECT patient was included as the control (120-kVp group). No cases were excluded because of motion artefacts or procedural errors in either group.
For the lesion analysis, we identified 49 hypervascular hepatocellular carcinomas (HCCs) in 19 patients (26 lesions in nine patients in the DL-DECT group, and 23 lesions in ten patients in the 120-kVp group). The diagnoses were conducted with the consensus of two radiologists with 10 years and 21 years of experience in abdominal CT based on the typical image findings on multiphasic CT. These diagnoses were also confirmed on gadoxetic acid–enhanced MRI (n = 34) or CT hepatic angiography/CT arterial portography (n = 15) performed within the 4-weeks following the multiphasic hepatic CT and tumour marker level measurement [31]. Each group’s detailed patient demographics are shown in Table 1.
CT scanning parameters and CM infusion protocol for each group
The scanning parameters are shown in Table 2. A tube voltage of 120-kVp and tube current modulation were used for each protocol. For the 120-kVp and DL-DECT groups, 600 mg I/kg [2] and 300 mg I/kg (Omnipaque-300; Daiichi-Sankyo, Tokyo, Japan or Iopamiron-370; Bayer Healthcare, Osaka, Japan) were delivered respectively over 30 s, followed by 30 mL of a saline solution. To minimise the effects of iodine concentration, we used a fixed fractional dose for each protocol (20 and 10 mgI/kg/s for the 120-kVp and DL-DECT groups, respectively). Unenhanced and three-phase contrast-enhanced images were acquired at hepatic arterial, portal venous, and equilibrium phases (HAP, PVP, and EP). A bolus-tracking technique was used to time the start of the scanning. The trigger threshold was set to 150 HU at the abdominal aorta. HAP, PVP, and EP scans were started 18, 55, and 160 s later.
Image reconstruction
In the DL-DECT group, the spectral-based image data were post-processed on a dedicated workstation (Spectral Diagnostic Suite; Philips Healthcare) to generate the VMI at seven different energy levels (40–70 keV in 5-keV increments) with a spectral level of 3 (DL-DECT-VMI). The spectral reconstruction algorithm uses a model-based IR developed for DL-DECT that offers seven denoising levels, with higher levels yielding more noise reduction. For this study, a moderate setting of level 3 was used, according to vendor recommendations. In the 120-kVp group, the images were reconstructed using a hybrid-IR (iDose4; Philips Healthcare) of level 3. The slice thickness and increment were both 5 mm.
Quantitative image analysis
Two board certified radiologists with 10 and 21 years of experience in abdominal CT performed the quantitative analysis. The aortic attenuation (HUaorta) during the HAP, and the hepatic attenuation (HUliver) during the PVP and EP, were measured by placing circular regions-of-interest (ROI). We also measured the CT attenuation of the spinal-erector muscle (HUmuscle) at each phase. We defined image noise as the standard deviation (SD) of the HUaorta during the HAP, and the SD of the HUliver during the PVP and EP. All ROIs were placed by consensus of the two operators, and measurements were performed twice to ensure consistency, with the averaged values being used for the analysis. Contrast-to-noise ratio (CNR) was calculated with the following formulas:
For the lesion analysis, the CT attenuation of the tumour and surrounding hepatic parenchyma were measured by placing ROIs in each phase. The tumour-to-liver contrast (TLC) during each enhancement phase was calculated as the difference between the CT attenuation of the tumour and the surrounding hepatic parenchyma. The tumour-to-liver CNR (TL-CNR) was calculated by dividing the TLC by the image noise.
Qualitative image analysis
Two board-certified radiologists with 7 and 14 years of experience who were blinded to the acquisition protocols independently performed qualitative analysis. The image sets, including the unenhanced, HAP, PVP, and EP of each patient, were presented in random order with a fixed window (window level and width, 50 and 350 HU, respectively). The radiologists evaluated the degree of vessel and organ contrast using the following five-point scale: 1 = poor, undiagnostic; 2 = suboptimal, low confidence; 3 = average; 4 = better than average; 5 = excellent. The noise and streak artefacts were rated as; 1 = undiagnostic; 2 = major; 3 = moderate; 4 = minor; 5 = not perceivable. Finally, the overall quality was rated as: 1 = undiagnostic; 2 = suboptimal and low confidence; 3 = average; 4 = above average and improved confidence; and 5 = excellent. For the lesion analysis, the conspicuity of HCC was evaluated according to the following five-point scale: 1 = undetectable, 2 = detectable but potentially missed, 3 = detectable and probably not missed, 4 = most likely will identify lesion, 5 = detectable without diagnostic compromise. The conspicuity of the ‘washout sign’ was evaluated using the more clearly depicted phase of either the PVP or EP. Inter-reader disagreements were resolved by consensus during a joint reading to determine the final score.
Radiation dose measurement for each protocol
The CT dose index (CTDIvol) was recorded at each phase, and the size-specific dose estimate (SSDE) was also calculated to take into consideration corrections according to the size of the patients. In each patient, the effective diameter (√ anterior-posterior diameter [cm] × lateral diameter [cm]) at the mid-liver level was measured on axial CT images to determine the conversion factor, and then the CTDIvol was multiplied by the conversion factor for SSDE determination [32]. The averaged values of three enhancement phases were used for the analysis.
Statistical analysis
Statistical analyses were performed with the statistical software R (version 2.6.1; www.r-project.org/). All numerical values were expressed as mean ± SD, and the normality of the distributions were confirmed with the Kolmogorov–Smirnov test. We used a two-tailed Student’s t-test to compare the CTDIvol, SSDE, BW, BMI, effective diameter, eGFR and iodine load between the two patient groups. Fisher’s exact test was used to measure differences between categorical variables. We used one-way ANOVA for multiple comparisons of the quantitative values. If a significant difference was found, pairwise comparisons were performed with the Dunnett test, with the values obtained from the 120-kVp images serving as the control. The visual scores were compared using the Kruskal-Wallis test. If a significant difference was found, pairwise comparisons were performed with a Steel’s test, with the values obtained from the120-kVp images serving as the control. The association between BMI and image noise or CNR at PVP was evaluated with Pearson’s correlation coefficient. The Kappa coefficients assessing inter-rater reliability were defined as: less than 0.20 = poor, 0.21–0.40 = fair, 0.41–0.60 = moderate, 0.61–0.80 = substantial, and 0.81–1.00 = near-perfect. Differences of p < 0.05 were considered statistically significant.
Results
Estimated radiation dose and iodine load for each protocol
The CTDIvol and SSDE in the DL-DECT group were significantly lower than in the 120-kVp group (CTDIvol: 12.3±2.3 vs 13.4±2.3 mGy, p < 0.01; SSDE: 17.3±2.2 vs 19.0±2.6 mGy, p < 0.01). The iodine load of the DL-DECT protocol was substantially reduced compared with the 120-kVp protocol (17.4±3.2 vs 35.5±6.5 g I, p < 0.01).
Quantitative image analysis
The image noise on DL-DECT-VMI showed a subtle increase as the energy level decreased, but remained at a low level (differences of ≤15%). When compared with the 120-kVp, it was significantly lower at 60–70 keV for the HAP and EP, and at 65–70 keV for the PVP (Fig. 1a–c). The aortic and hepatic attenuation of DL-DECT-VMI revealed a steep increase as the energy decreased, and at 55- or 60-keV it reached a level almost equivalent to that of 120-kVp (Fig. 1d–f). Similarly, the CNR showed a gradual increase as the keV levels decreased. Compared with 120-kVp, the CNRs of the aorta and hepatic parenchyma on DL-DECT-VMI were significantly higher at 40–55 keV and 40–50 keV, respectively, (Fig. 1g–i). A slightly higher correlation between BMI and noise was found in DL-DECT-VMI than in 120-kVp, whereas no statistically significant correlation was observed between BMI and CNR in either group (Fig. 2).
Box-and-whisker plots showing the image noise (a–c), CT attenuation (d–f) and CNR (g–i) of DL-DECT-VMI and conventional 120-kVp images during the HAP, PVP and EP. Boxes show the upper and lower quartiles, with median values being shown by the horizontal lines within the boxes. The whiskers represent maximum and minimum values. *DL-DECT > 120-kVp (p < 0.05), **DL-DECT > 120-kVp (p < 0.01), †DL-DECT < 120-kVp (p < 0.05), ††DL-DECT < 120-kVp (p < 0.01)
Qualitative image analysis
A summary of the qualitative image analysis is shown in Table 3. Compared with the 120-kVp, the iodine contrast of DL-DECT-VMI was rated as inferior at 60–70 keV (p < 0.01), equivalent at 50 and 55 keV (p = 0.27 and 0.73, respectively), and superior at 40- and 45-keV (p < 0.01). In comparison with 120-kVp, the noise on DL-DECT-VMI was rated as lower at 55–70 keV (p < 0.05), and equivalent at 40–50 keV (p = 0.1–1.0), whereas no significant difference was observed in streak artefact between any of the image sets (p = 0.09–1.0). The highest score for overall quality in DL-DECT-VMI was attained at 40-keV, which was followed by 45- and 50-keV, all of which were superior to 120-kVp (p < 0.05). There was no significant difference in overall quality between 55-keV and 120-kVp images (p = 0.92).
Lesion analysis
The absolute values of the TLC and TL-CNR of DL-DECT-VMI maximised at 40-keV. Compared with the 120-kVp, DL-DECT-VMI in the HAP showed significantly superior TLC at 40–50 keV (p < 0.01), and a significantly superior TL-CNR at 40- and 45-keV (p < 0.01). There were no significant differences in TLC and TL-CNR during the PVP and EP (PVP, p = 0.98; EP, p = 1.0; Table 4). In the qualitative analysis, the conspicuity score showed a similar tendency to the quantitative lesion analysis (Fig. 3). There was moderate to substantial inter-reader agreement with regard to image quality (κ = 0.59–0.74) and lesion conspicuity (κ = 0.73 and 0.64 for HAP and PVP, respectively). Representative cases are shown in Figs. 4 and 5.
An 80-year-old woman (body weight, 47 kg; BMI, 21.2 kg/m2) with renal dysfunction (eGFR: 37 mL/min/1.73 m2) underwent multiphasic hepatic CT with DL-DECT for the surveillance of chronic hepatitis C (Omnipaque 300; 42 mL at 1.4 mL/s; SSDE, 14.8 mGy). The upper, middle, and lower rows show the VMI (40–70 keV) during the HAP, PVP, and EP, respectively. The conspicuity of a small hypervascular HCC (arrows) gradually improves as the energy level decreases, especially in the HAP images
CT images of a 78-year-old woman (body weight, 63 kg; BMI, 22.3 kg/m2) with a history of HCC (arrows). The patient underwent initial scanning with 120-kVp (Omnipaque 300; 128 mL at 4.2 mL/s) and then a follow up study after 6 months with DL-DECT using a 50% iodine load (Omnipaque 300; 63 mL at 2.1 mL/s), because of deterioration in renal function (eGFR: 34 mL/min/1.73 m2). The upper, middle, and lower rows show the respective HAP, PVP, and EP images of each protocol. Lesion conspicuity in DL-DECT-VMI improves as energy decreases, without severe image noise elevation. Compared with the conventional 120-kVp images, an almost equivalent lesion conspicuity in the HAP, and iodine contrast in all phases, was attained at around 55–60 keV, with the DL-DECT-VMI allowing a 50% reduction in iodine load without increasing the radiation dose (SSDE: DL-DECT, 14.7 mGy vs. 120-kVp, 15.4 mGy)
Discussion
Our results demonstrated that in comparison with conventional 120-kVp multiphasic hepatic CT with IR, DL-DECT-VMI at 40–50 keV with a 50% iodine load yielded significantly greater arterial and hepatic attenuation. The image noise on DL-DECT-VMI remained at low levels across the energy settings, and equivalent to or lower than that of the 120-kVp images. Consequently, the CNR in the lower keV images was significantly greater than in the 120-kVp. These quantitative measurements were supported by the results of the visual assessment. Furthermore, the lesion analysis revealed that the conspicuity of VMI at 40–55 keV was comparable to or better than that of 120-kVp images.
To our knowledge, this is the first investigation to reveal the usefulness of DL-DECT-VMI for iodine dose reduction in multiphasic hepatic CT by comprehensively evaluating image quality, lesion conspicuity, and radiation dose using 120-kVp with IR and a full iodine dose as the reference standard [22, 33]. Our results are in line with recent reports on DL-DECT, which showed that the vascular CNR was maximised at 40-keV in the adult and paediatric populations [25, 34]. In addition, we could validate the applicability of low keV images for iodine dose reduction in clinical settings, the possibility of which was inferred in an ex-vivo phantom experiment by Tsang et al. [34]. The comparison with 120-kVp with IR instead of filtered-back projection is of clinical importance, as IR has already been implemented for abdominal CT at most institutions, to improve image quality or reduce radiation dose. In this context, we found that the noise on DL-DECT-VMI at reduced radiation doses could be equivalent to that of 120-kVp IR images, even at 40-keV. The almost homogeneous low noise levels across each keV setting, which are in contrast to the results of previous reports on different dual-energy technologies in abdominal CT [12, 19,20,21,22, 33] may be derived from the exploitation of anti-correlated noise suppression and the implementation of dedicated model-based IR in the projection domain, where the exactly matched high and low energy datasets can be post-processed without need for angular and temporal interpolation [24,25,26,27,28,29,30, 34,35,36,37,38].
In the lesion analysis, we found that the subjective and objective conspicuity of HCC during the HAP was highest at 40-keV, followed by 45- and 50-keV, with it being equivalent to 120-kVp at 55-keV. The relatively large difference in iodine concentration between HCC and the surrounding hepatic parenchyma during the HAP may help to emphasise lesion conspicuity at lower monoenergetic levels. The TLC during PVP and EP improved slightly as the energy decreased, and was almost equivalent to that of 120-kVp at 55-keV, although neither the degree of improvement nor the difference from 120-kVp images were statistically significant. Possible reasons for the disparities between the HAP and PVP/EP include the fact that the iodine concentration difference between HCC and surrounding hepatic parenchyma during PVP/EP is relatively small, and that the TLC during PVP/EP is less affected by the iodine load than it is during the HAP [39]. Our findings suggest that a further iodine load or radiation dose reduction may be possible for hepatic DL-DECT, especially for lesions showing hypervascularity.
In the present study, we evaluated the image quality of DL-DECT-VMI using 120-kVp images as the reference standard, but comparisons with low kVp images could be an interesting research subject. Low kVp scans with IR allow for not only a reduction in iodine load, but also a considerable radiation dose reduction, especially for thin patients [40]. In contrast, DECT allows for spectral-based imaging techniques such as virtual non-contrast imaging, iodine maps, and effective Z maps, as well as optimisation of iodine contrast according to the demand for each examination and each organ of interest, or reduction of artefacts by reconstruction of VMI at arbitrary monoenergetic levels [23, 24]. Moreover, although the dual-energy information is only available at 120-kVp or 140-kVp scans on DL-DECT system, the spectral analysis is retrospectively operable for all these acquisitions, without presetting the ‘dual-energy mode’. Given these advantages, it should be clarified whether spectral-based imaging with DL-DECT is superior in diagnostic accuracy to low-kVp scans, and whether it improves the long-term patient outcomes.
In this study, the control group was retrieved from cases scanned with a different single-energy CT system, because the number of cases having undergone 120-kVp scans on the novel DL-DECT system was insufficient to perform matched-pair analysis. Therefore, inherent differences in scanner properties, such as the behaviour of tube current modulation or image processing algorithms, may have somewhat influenced the radiation dose and image quality. With regard to the image processing, the VMI is synthesised using a dedicated spectral reconstruction algorithm that takes into account anti-correlated noise features and utilises the IR technique. The image reconstruction process in DL-DECT and single-energy CT is not completely equivalent, mainly because of the differences in detector technology. Nevertheless, we believe that comparisons on image quality and radiation dose were performed under as fair conditions as possible, because we used the same corresponding denoising strength (level 3) for both protocols, which provides the same degree of noise reduction (unpublished data).
Several potential limitations need to be acknowledged in this study. First, the numbers of patients and lesions were relatively small, as this study covered the initial clinical experience of a novel DL-DECT system. Further large-scale studies will be needed to validate our results. Second, our patients’ body size is smaller than that of Western individuals. Generally, in large-bodied patients, image noise is increased and CNR is decreased in comparison to small-bodied patients, especially in low energy images [19, 41, 42]. We also found a weak correlation between image noise and BMI in the DL-DECT group. However, even in patients with a relatively large BMI, the increase in noise and decrease in CNR in the lower keV images were not very serious, and remained almost equivalent to or better than those of 120-kVp. Because this study did not include patients with a BMI > 30 kg/m2, whether our findings would also apply to such populations should be addressed in future studies. Third, we could not compare the diagnostic performance due to the lack of a pathological and imaging reference standard; rather, we focused on evaluating the image quality, lesion conspicuity and radiation dose in each protocol. Finally, we evaluated image quality using relatively thick slices (5 mm) that had relatively low image noise. In our institution, hepatic CT images were routinely reconstructed at 5 mm slice intervals to avoid excessive data loads derived from the multiphasic acquisitions, and thinner slices were selectively reconstructed for limited anatomical areas where detailed assessment was necessary. However, prior investigations on DL-DECT have shown that image noise could be kept at an almost constant level across each keV, even at thinner image slices (0.67–3 mm) [24, 25, 34]. Thus, our results might be applicable for images at various slice thicknesses, although further clinical study is needed to address the effect of slice thickness on image quality.
In conclusion, for multiphasic hepatic CT, VMI generated from DL-DECT maximises the subjective diagnostic confidence, quantitative image quality, and lesion conspicuity at 40-keV, owing to the highest iodine contrast and an acceptable image noise level. When compared with conventional 120-kVp with an iterative reconstruction algorithm, DL-DECT-VMI at 40–55 keV yields equivalent or better image quality and lesion conspicuity, regardless of the 50% iodine load reduction and reduced radiation dose.
Abbreviations
- CM:
-
Contrast medium
- CNR:
-
Contrast-to-noise ratio
- CTDIvol :
-
volume CT dose index
- DECT:
-
Dual-energy CT
- DL-DECT:
-
Dual-layer dual-energy CT
- eGFR:
-
Estimated glomerular filtration rate
- EP:
-
Equilibrium phase
- HAP:
-
Hepatic arterial phase
- HCC:
-
Hepatocellular carcinoma
- IR:
-
Iterative reconstruction
- PVP:
-
Portal venous phase
- ROI:
-
Region of interest
- SSDE:
-
Size-specific dose estimate
- TLC:
-
Tumour-to-liver contrast
- TL-CNR:
-
Tumour-to liver contrast-to-noise ratio
- VMI:
-
Virtual monochromatic imaging
References
Heiken JP, Brink JA, McClennan BL, Sagel SS, Crowe TM, Gaines MV (1995) Dynamic incremental CT: effect of volume and concentration of contrast material and patient weight on hepatic enhancement. Radiology 195:353–357
Yamashita Y, Komohara Y, Takahashi M et al (2000) Abdominal helical CT: evaluation of optimal doses of intravenous contrast material--a prospective randomized study. Radiology 216:718–723
McDonald JS, McDonald RJ, Carter RE, Katzberg RW, Kallmes DF, Williamson EE (2014) Risk of intravenous contrast material-mediated acute kidney injury: a propensity score-matched study stratified by baseline-estimated glomerular filtration rate. Radiology 271:65–73
Launay-Vacher V, Oudard S, Janus N et al (2007) Prevalence of Renal Insufficiency in cancer patients and implications for anticancer drug management: the renal insufficiency and anticancer medications (IRMA) study. Cancer 110:1376–1384
Garcia-Compean D, Jaquez-Quintana JO, Maldonado-Garza H (2009) Hepatogenous diabetes. Current views of an ancient problem. Ann Hepatol 8:13–20
Stacul F, van der Molen AJ, Reimer P et al (2011) Contrast induced nephropathy: updated ESUR Contrast Media Safety Committee guidelines. Eur Radiol 21:2527–2541
Cicin I, Erdogan B, Gulsen E et al (2014) Incidence of contrast-induced nephropathy in hospitalised patients with cancer. Eur Radiol 24:184–190
Mangold S, Wichmann JL, Schoepf UJ et al (2016) Automated tube voltage selection for radiation dose and contrast medium reduction at coronary CT angiography using 3(rd) generation dual-source CT. Eur Radiol 26:3608–3616
Taguchi N, Oda S, Utsunomiya D et al (2016) Using 80 kVp on a 320-row scanner for hepatic multiphasic CT reduces the contrast dose by 50 % in patients at risk for contrast-induced nephropathy. Eur Radiol. https://doi.org/10.1007/s00330-016-4435-y
Albrecht MH, Scholtz JE, Husers K et al (2016) Advanced image-based virtual monoenergetic dual-energy CT angiography of the abdomen: optimization of kiloelectron volt settings to improve image contrast. Eur Radiol 26:1863–1870
Albrecht MH, Scholtz JE, Kraft J et al (2015) Assessment of an Advanced Monoenergetic Reconstruction Technique in Dual-Energy Computed Tomography of Head and Neck Cancer. Eur Radiol 25:2493–2501
Lv P, Lin XZ, Chen K, Gao J (2012) Spectral CT in patients with small HCC: investigation of image quality and diagnostic accuracy. Eur Radiol 22:2117–2124
Delesalle MA, Pontana F, Duhamel A et al (2013) Spectral optimization of chest CT angiography with reduced iodine load: experience in 80 patients evaluated with dual-source, dual-energy CT. Radiology 267:256–266
Agrawal MD, Oliveira GR, Kalva SP, Pinho DF, Arellano RS, Sahani DV (2016) Prospective Comparison of Reduced-Iodine-Dose Virtual Monochromatic Imaging Dataset From Dual-Energy CT Angiography With Standard-Iodine-Dose Single-Energy CT Angiography for Abdominal Aortic Aneurysm. AJR Am J Roentgenol 207:W125–w132
Shuman WP, Chan KT, Busey JM, Mitsumori LM, Koprowicz KM (2016) Dual-energy CT Aortography with 50% Reduced Iodine Dose Versus Single-energy CT Aortography with Standard Iodine Dose. Acad Radiol 23:611–618
Kanal KM, Chung JH, Wang J et al (2011) Image noise and liver lesion detection with MDCT: a phantom study. AJR Am J Roentgenol 197:437–441
Schindera ST, Torrente JC, Ruder TD et al (2011) Decreased detection of hypovascular liver tumors with MDCT in obese patients: a phantom study. AJR Am J Roentgenol 196:W772–W776
Yu L, Li H, Fletcher JG, McCollough CH (2010) Automatic selection of tube potential for radiation dose reduction in CT: a general strategy. Med Phys 37:234–243
Marin D, Ramirez-Giraldo JC, Gupta S et al (2016) Effect of a Noise-Optimized Second-Generation Monoenergetic Algorithm on Image Noise and Conspicuity of Hypervascular Liver Tumors: An In Vitro and In Vivo Study. AJR Am J Roentgenol 206:1222–1232
Bellini D, Gupta S, Ramirez-Giraldo JC et al (2017) Use of a Noise Optimized Monoenergetic Algorithm for Patient-Size Independent Selection of an Optimal Energy Level During Dual-Energy CT of the Pancreas. J Comput Assist Tomogr 41:39–47
Caruso D, De Cecco CN, Schoepf UJ et al (2017) Can dual-energy computed tomography improve visualization of hypoenhancing liver lesions in portal venous phase? Assessment of advanced image-based virtual monoenergetic images. Clin Imaging 41:118–124
Lv P, Liu J, Chai Y, Yan X, Gao J, Dong J (2017) Automatic spectral imaging protocol selection and iterative reconstruction in abdominal CT with reduced contrast agent dose: initial experience. Eur Radiol 27:374–383
van Hamersvelt RW, Schilham AM, Engelke K et al (2017) Accuracy of bone mineral density quantification using dual-layer spectral detector CT: a phantom study. Eur Radiol. https://doi.org/10.1007/s00330-017-4801-4
Hickethier T, Baessler B, Kroeger JR et al (2017) Monoenergetic reconstructions for imaging of coronary artery stents using spectral detector CT: In-vitro experience and comparison to conventional images. J Cardiovasc Comput Tomogr 11:33–39
Doerner J, Hauger M, Hickethier T et al (2017) Image quality evaluation of dual-layer spectral detector CT of the chest and comparison with conventional CT imaging. Eur J Radiol 93:52–58
Kalender WA, Klotz E, Kostaridou L (1988) An algorithm for noise suppression in dual energy CT material density images. IEEE Trans Med Imaging 7:218–224
Alvarez RE, Macovski A (1976) Energy-selective reconstructions in X-ray computerized tomography. Phys Med Biol 21:733–744
Maass C, Baer M, Kachelriess M (2009) Image-based dual energy CT using optimized precorrection functions: a practical new approach of material decomposition in image domain. Med Phys 36:3818–3829
Maass C, Meyer E, Kachelriess M (2011) Exact dual energy material decomposition from inconsistent rays (MDIR). Med Phys 38:691–700
Chang W, Lee JM, Lee K et al (2013) Assessment of a model-based, iterative reconstruction algorithm (MBIR) regarding image quality and dose reduction in liver computed tomography. Invest Radiol 48:598–606
Choi JY, Lee JM, Sirlin CB (2014) CT and MR imaging diagnosis and staging of hepatocellular carcinoma: part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 273:30–50
Christner JA, Braun NN, Jacobsen MC, Carter RE, Kofler JM, McCollough CH (2012) Size-specific dose estimates for adult patients at CT of the torso. Radiology 265:841–847
Clark ZE, Bolus DN, Little MD, Morgan DE (2015) Abdominal rapid-kVp-switching dual-energy MDCT with reduced IV contrast compared to conventional MDCT with standard weight-based IV contrast: an intra-patient comparison. Abdom Imaging 40:852–858
Tsang DS, Merchant TE, Merchant SE, Smith H, Yagil Y, Hua CH (2017) Quantifying potential reduction in contrast dose with monoenergetic images synthesized from dual layer detector spectral CT. Br J Radiol. https://doi.org/10.1259/bjr.20170290:20170290
Lehmann LA, Alvarez RE, Macovski A et al (1981) Generalized image combinations in dual KVP digital radiography. Med Phys 8:659–667
Yu L, Leng S, McCollough CH (2012) Dual-energy CT-based monochromatic imaging. AJR Am J Roentgenol 199:S9–s15
Zhao X, Hu JJ, Zhao YS, Zhang HT, Zhang P (2014) Iterative dual energy material decomposition from spatial mismatched raw data sets. J Xray Sci Technol 22:745–762
Dong X, Niu T, Zhu L (2014) Combined iterative reconstruction and image-domain decomposition for dual energy CT using total-variation regularization. Med Phys 41:051909
Fujigai T, Kumano S, Okada M et al (2012) Optimal dose of contrast medium for depiction of hypervascular HCC on dynamic MDCT. Eur J Radiol 81:2978–2983
Nakaura T, Nakamura S, Maruyama N et al (2012) Low contrast agent and radiation dose protocol for hepatic dynamic CT of thin adults at 256-detector row CT: effect of low tube voltage and hybrid iterative reconstruction algorithm on image quality. Radiology 264:445–454
Leng S, Yu L, Fletcher JG, McCollough CH (2015) Maximizing Iodine Contrast-to-Noise Ratios in Abdominal CT Imaging through Use of Energy Domain Noise Reduction and Virtual Monoenergetic Dual-Energy CT. Radiology 276:562–570
Husarik DB, Gordic S, Desbiolles L et al (2015) Advanced virtual monoenergetic computed tomography of hyperattenuating and hypoattenuating liver lesions: ex-vivo and patient experience in various body sizes. Invest Radiol 50:695–702
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yasuyuki Yamashita.
Conflict of interest
The authors of this manuscript declare no relationships with any companies.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Methodology
• retrospective
• case-control study
• performed at one institution
Rights and permissions
About this article
Cite this article
Nagayama, Y., Nakaura, T., Oda, S. et al. Dual-layer DECT for multiphasic hepatic CT with 50 percent iodine load: a matched-pair comparison with a 120 kVp protocol. Eur Radiol 28, 1719–1730 (2018). https://doi.org/10.1007/s00330-017-5114-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5114-3