Abstract
Objectives
To investigate the usefulness of voxel-based analysis of standardized uptake values (SUVs) and apparent diffusion coefficients (ADCs) for evaluating soft-tissue tumour malignancy with a PET/MR system.
Methods
Thirty-five subjects with either ten low/intermediate-grade tumours or 25 high-grade tumours were prospectively enrolled. Zoomed diffusion-weighted and fluorodeoxyglucose (18FDG)-PET images were acquired along with fat-suppressed T2-weighted images (FST2WIs). Regions of interest (ROIs) were drawn on FST2WIs including the tumour in all slices. ROIs were pasted onto PET and ADC-maps to measure SUVs and ADCs within tumour ROIs. Tumour volume, SUVmax, ADCminimum, the heterogeneity and the correlation coefficients of SUV and ADC were recorded. The parameters of high- and low/intermediate-grade groups were compared, and receiver operating characteristic (ROC) analysis was also performed.
Results
The mean correlation coefficient for SUV and ADC in high-grade sarcomas was lower than that of low/intermediate-grade tumours (−0.41 ± 0.25 vs. −0.08 ± 0.34, P < 0.01). Other parameters did not differ significantly. ROC analysis demonstrated that correlation coefficient showed the best diagnostic performance for differentiating the two groups (AUC 0.79, sensitivity 96.0%, specificity 60%, accuracy 85.7%).
Conclusions
SUV and ADC determined via PET/MR may be useful for differentiating between high-grade and low/intermediate-grade soft tissue tumours.
Key Points
• PET/MR allows voxel-based comparison of SUVs and ADCs in soft-tissue tumours.
• A comprehensive assessment of internal heterogeneity was performed with scatter plots.
• SUVmax or ADCminimum could not differentiate high-grade sarcoma from low/intermediate-grade tumours.
• Only the correlation coefficient between SUV and ADC differentiated the two groups.
• The correlation coefficient showed the best diagnostic performance by ROC analysis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Soft-tissue tumours are characterized by a highly heterogeneous inner structure, consisting of a variety of interstitial tissues including collagen fibre and mucinous fluid, in addition to tumour cells [1, 2]. The assessment of the malignancy grade of soft-tissue tumours is important for determining treatment strategies and patient care. X-rays, computed tomography (CT) and magnetic resonance imaging (MRI) have all been widely used for such assessments [3,4,5], but such morphological imaging does not always facilitate the determination of the malignancy grade of the tumour.
Recently, several functional imaging techniques have been applied for the clinical assessment of soft-tissue tumours [6,7,8,9,10,11,12,13,14,15]. Fluorodeoxyglucose-positron emission tomography (18FDG-PET) is one such imaging modality that has been widely used. Reportedly, higher maximum standardized uptake values (SUVmax) are significantly associated with higher-grade tumours [6, 7]. However, it is often difficult to differentiate high-grade from low- and intermediate-grade tumours. Some low-grade tumours yield a high SUVmax relative to some high-grade tumours, and the two groups definitely overlap with regard to SUVmax range [6, 7]. Thus, solely SUVmax-based quantification methods are potentially problematic, as the assessment of soft tissue tumours with a single voxel measurement of SUVmax may not accurately reflect the malignancy grade or the metabolic activity of a whole tumour, even where a tumour has a highly heterogeneous appearance. Some researchers have also exploited the mean of SUV (SUVmean) as well as SUVmax, but there still remained considerable overlaps between low-grade and high-grade tumours, probably due to the inhomogeneity of soft-tissue tumours [8, 9].
Diffusion-weighted magnetic resonance imaging (DWI) is a magnetic resonance (MR) method based on the Brownian motion of water molecules. Apparent diffusion coefficient (ADC) values calculated via DWI obtained with a variety of b-factors have been reported to reflect cellular density in tissue [10, 11]. Mean ADC (ADCmean) and minimum ADC (ADCminimum) values have been used for the assessment of malignancy grade, as well as the evaluation of treatment effects in soft-tissue tumours [12,13,14,15]. However, it has not always proved accurate, as ADC values vary depending not only on cellular density but also the amounts of interstitial tissues such as collagen fibre, mucinous fluid and calcification, among others, in soft-tissue tumours.
The combined use of 18FDG-PET and ADC has recently been investigated in efforts to improve the diagnostic accuracy of methods relying solely on SUVmax, SUVmean, ADCmean and ADCminimum for the assessment of malignancy, and its usefulness has been reported for some types of tumours [16,17,18]. Regions of interest (ROIs) were placed in images derived via different modalities individually for the comparison of SUVmax, SUVmean, ADCmean and ADCminimum values inside the ROIs. However, in these studies there were limitations to the ROI-based methods utilized. First, a single voxel for SUVmax measurement rarely seems consistent with a point for the measurement of ADCminimum. Second, SUVmax represents a single voxel in a tumour, while ADCmean represents a whole tumour. Lastly, the ROI-based methods utilized cannot incorporate tumour heterogeneity when the tumour has a variety of different components, especially with SUVmean or ADCmean. Thus, even the combined use of SUVmax or SUVmean and ADCmean or ADCminimum cannot incorporate the heterogeneity of the whole tumour into the assessment of tumour malignancy. Therefore, there is an urgent need to develop a voxel-by-voxel comparison method for comprehensive assessment of soft-tissue tumours.
A hybrid PET/MR system has recently been developed that enables the acquisition of 18FDG-PET and DWI simultaneously, and precise image co-registration [19], and could potentially enable direct voxel-by-voxel comparison of SUV and ADC. We hypothesized that the comprehensive assessment of the heterogeneity of soft-tissue tumours via multiparametric voxel-based analysis could facilitate the diagnosis of malignancy of soft-tissue tumours.
The purpose of the present study was to investigate the feasibility and usefulness of voxel-based analysis of SUV and ADC in the evaluation of soft-tissue tumour malignancy with a PET/MR system.
Materials and methods
Study protocol
This single-institute prospective study was approved by the institutional review board. From October 2014 to March 2016, patients with known soft-tissue tumours who were scheduled to undergo PET/CT scanning were recruited consecutively. Written informed consent was obtained from all patients. Each patient underwent PET/MR scanning immediately after PET/CT scanning. Exclusion criteria were as follows: failure to obtain consent, incomplete scan or severe image artefact or distortion on DWI, a tumour volume too small to accommodate voxel-based analysis (<10.0 cm3) and history of treatment for the tumour. The pathological specimens were obtained by either biopsy or surgical resection, and diagnosed in the department of pathology at our institute. The subjects were then divided into high-grade and low/intermediate-grade tumour groups based on the WHO classification of tumours of soft tissue and bone 2013 [2].
Image acquisition
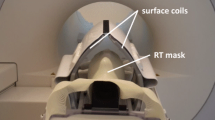
PET/MR imaging was performed with the Ingenuity TF PET/MR system (Philips Healthcare, Cleveland, OH, USA). The subjects were administered 4.0 MBq/kg of 18FDG and underwent PET/CT 60 min after injection as part of a clinical routine, and then PET/MR imaging was initiated 122 ± 15 min after the administration of 18FDG. After the scout image was taken and a three-dimensional (3D) T1-weighted image (T1WI) was acquired to correct attenuation [20], participants underwent PET imaging with 3D-ordered subset expectation maximization (3D-OSEM) and time of flight (TOF). The field of view (FOV) for the PET imaging was 576 mm × 576 mm. The sampling time was 5 min per station, and images were reconstructed with 23 mm voxels. After PET imaging, diagnostic MRI was performed. Any one coil among a 32-channel phased array body coil, a 16-channel neurovascular coil, 8-channel shoulder coil, small extremity coil, knee coil and ankle coil was used depending on the location of the target lesion. Transaxial two-dimensional (2D) fat-suppressed T2-weighted images (FST2WIs) and T1WIs were obtained using a turbo-spin echo sequence to cover entire tumour volume. A DWI method incorporating spatially-selective radiofrequency (RF) pulses called zoomed DWI (b = 0 and 800) [19] was then performed, and an ADC map was generated. The details of the sequence parameters are shown in Table 1. Other diagnostic MRI was performed when necessary, in the clinic. The total scan time was 50–60 min.
Image processing
The procedures for the construction of a scatter plot from the PET and MR data are described in Fig. 1. First, image registration with rigid transformation [21, 22] was performed between the FST2WI, the ADC map and the PET image on an Intellispace Portal workstation (version 6.0, Philips Healthcare). The FST2WI and the PET image were then resliced in accordance with the ADC map (5 or 6 mm) using Osirix MD software (version 6.5, Pixmeo, Geneva, Switzerland). Subsequent image processing was performed using Image J software (version 1.43, NIH, Bethesda, MD, USA). On FST2WIs, ROIs were manually drawn along the border of the tumour in all slices by consensus between two board-certified radiologists (K.S. and Y.W.) with 11 and 34 years of experience in radiology, respectively. Bulky fat tissue areas were carefully excluded from the ROIs because the signal intensity of fat tissue was too low to count on the DWI images using the fat-suppression technique, and ADC values derived from fat tissue could not be correctly measured. The ROIs were then copied onto the ADC maps and PET images. After extracting tumour area, in-plane image resolution was interpolated to 42 mm from 22 mm. Therefore, the processed PET imaging included 10–12 of the original 22 mm voxels. Voxels with ADC values less than 0.3 × 10−6 mm2/s or more than 3.5 × 10−6 mm2/s were regarded as outliers of ADC [23, 24], and excluded from the analysis. The ADCs and SUVs within the whole tumour ROIs were recorded along with the X-Y coordinates in a voxel-wise manner, and scatter plots of SUV versus ADC were generated for each tumour.
The procedures for constructing scatter plots from PET and MR data. (1) Perform image registration and reslice fat-suppressed T2-weighted image (FST2WI) and PET image in accordance with the apparent diffusion coefficient (ADC) map, then draw a region of interest (ROI) on the FST2WI and copy the ROI onto the ADC map and PET image. (2) Extract tumour area from the ADC map and PET image along with X-Y coordinates. (3) Convert in-plane resolution from 22 mm to 42 mm for all slices. The final resolution of a single voxel is 4 × 4 × 5 or 6 mm, including 10–12 original PET voxels of 23-mm resolution. (4) Make a voxel-wise scatter plot of the standardized uptake value (SUV) as a function of ADC. The red ellipse indicates the 95% area of bivariate normal distribution of SUV and ADC used to quantify intra-tumoral heterogeneity
Parameters derived from the scatter plots
From the scatter plot of SUV and ADC, tumour volume, SUVmax and ADCminimum were recorded as ‘conventional’ measurements. In addition, the elliptical 95% area of bivariate normal distribution of SUV and ADC was calculated using our in-house program and a commercial software package (MATLAB 2015a, MathWorks, Natick, MA, USA) to quantify intra-tumoral heterogeneity. The correlation coefficient between SUV and ADC was calculated using Pearson’s test.
Statistical analysis
Tumour volume, SUVmax, ADCminimum, tumour heterogeneity and correlation coefficient were compared between high-grade and low/intermediated-grade groups via the Mann–Whitney U-test. Receiver operating characteristic (ROC) analysis was performed, and cut-off values were determined via the Youden index [25] to calculate the sensitivity, specificity and accuracy of each parameter for differentiating high-grade tumours from low/intermediate-grade tumours. All statistical analysis was performed using JMP Pro (version 11.0.0, SAS Institute Inc., Cary, NC, USA) and P < 0.05 was considered statistically significant.
Results
Forty-six subjects were initially recruited in total, and 35 subjects (aged 13–84 years, 19 male and 16 female) were included in the final study sample. The final diagnoses were 25 high-grade tumours including osteosarcoma (n = 6), pleomorphic sarcoma (n = 4), high-grade liposarcoma (n = 4), myxofibrosarcoma (n = 3), malignant peripheral nerve sheath tumour (MPNST) (n = 2), leiomyosarcoma (n = 2), synovial sarcoma (n = 1), clear cell sarcoma (n = 1), chondrosarcoma (n = 1) and malignant epithelioid tumour (n = 1), and ten low or intermediate-grade tumours including giant cell tumour (n = 3), schwannoma (n = 2), atypical lipomatous tumour (n = 1), osteochondroma (n = 1), neurofibroma (n = 1), haemangioma (n = 1) and non-bacterial osteomyelitis (n = 1). With regard to locations, there were 13 lesions in the leg, eight in the back, seven in the hip/pelvis, four in the neck and three in the arm.
Comparisons of each measurement between high-grade and low/intermediate-grade tumours are shown in Fig. 2. The mean tumour volumes were 129.6 ± 150.6 cm3 for high-grade tumours and 94.5 ± 141.8 cm3 for low/intermediate-grade tumours, and the difference was not significant (P = 0.30). SUVmax tended to be higher in high-grade sarcomas, but the difference was not statistically significant (6.3 ± 3.9 vs. 4.2 ± 3.7, P = 0.06). ADCminimum showed substantial overlap, and did not differ significantly between the two groups (0.92 ± 0.34 vs. 0.91 ± 0.38 × 10−6 mm2/s, P = 0.93).
As indicated by the scatter plot of SUV and ADC, the correlation coefficient of high-grade tumours (−0.41 ± 0.25) was significantly lower than that of low/intermediate-grade tumours (−0.08 ± 0.34, P < 0.01), meaning high-grade tumours were more strongly inversely correlated with SUV and ADC. Heterogeneity represented by the 95% area of SUV and ADC distribution tended to be higher in high-grade tumours (3.98 ± 3.30), but the difference was not significant (2.30 ± 2.38, P = 0.11).
The diagnostic performance of each parameter for differentiating high-grade tumours from low or intermediate-grade tumours via ROC analysis is listed in Table 2. Only the correlation coefficient between SUV and ADC showed significant diagnostic ability (P < 0.05). Figures 3 and 4 show representative cases of high-grade and low-grade tumours. High-grade tumours (Fig. 3) were adequately classified in 24 of 25 cases by the correlation coefficient between SUV and ADC, with the highest sensitivity (96.0%). Four high-grade tumours including one chondrosarcoma, one osteosarcoma and two liposarcomas were adequately diagnosed with the correlation coefficient, but not with the SUV peak (Fig. 5). Thus, the inverse correlation showed the best diagnostic accuracy (30 of 35; 85.7%).
Synovial sarcoma (high-grade) of the knee in a 24-year-old woman. (a) Fat-suppressed T2-weighted image (FST2WI) demonstrated a heterogeneous, lobulated tumour around the knee joint. (b) Apparent diffusion coefficient (ADC) mapping revealed reduced ADC values, especially in the centre of the tumour. (c) The tumour showed higher FDG uptake in the centre of the tumour on the 18FDG-PET/FST2WI fusion image. (d) The scatter plot of the standardized uptake value (SUV) and ADC showed a strong inverse correlation and larger heterogeneity of SUV and ADC. All parameters except tumour volume could adequately indicate high-grade tumour. Volume: 56.9 cm3, SUVmax: 5.40, ADCminimum: 0.56 × 10−6 mm2/s, heterogeneity: 2.64, correlation coefficient: −0.53
Schwannoma (low-grade) of the neck in a 77-year-old man. (a) Fat-suppressed T2-weighted image (FST2WI) demonstrated a smooth and well demarcated tumour with the ‘target appearance’ in the neck. (b) Apparent diffusion coefficient (ADC) mapping did not show reduced ADC values. (c) 18FDG uptake was minimal, but a small hot spot was evident in the centre of the tumour on the 18FDG-PET/FST2WI fusion image. (d) The scatter plot of the standardized uptake value (SUV) and ADC showed a weak inverse correlation, and low heterogeneity of SUV and ADC. All parameters except SUVmax could adequately indicate low-grade tumour. Volume: 14.8 cm3, SUVmax: 3.30, ADCminimum: 1.35 × 10−6 mm2/s, heterogeneity: 0.73, correlation coefficient: −0.07
Myxoid liposarcoma (high-grade) of the thigh in a 65-year-old man. (a) Fat-suppressed T2-weighted image (FST2WI) demonstrated a large heterogeneous tumour consisting of a myxoid component and a septum-like solid component inside the gluteus maximus. (b) Apparent diffusion coefficient (ADC) mapping revealed a slightly reduced ADC value in the solid part. (c) The tumour exhibited only slight FDG uptake in the septum on the 18FDG-PET/FST2WI fusion image. (d) The scatter plot of the standardized uptake value (SUV) and ADC showed a strong inverse correlation and substantial heterogeneity of SUV and ADC. SUVmax and ADC minimum could not adequately indicate high-grade tumour. Volume: 284.3 cm3, SUVmax: 1.59, ADCminimum: 1.26 × 10−6 mm2/s, heterogeneity: 1.21, correlation coefficient: −0.57
Discussion
This preliminary study evaluated the internal heterogeneity and malignancy grade of soft tissue tumours via multiparametric voxel-based analysis. Using hybrid PET/MR imaging, precise image co-registration between an 18FDG-PET image and an ADC map facilitated the voxel-by-voxel comparison of SUV and ADC. The voxel-wise scatter plot of SUV and ADC enabled the quantification of the internal heterogeneity of soft tissue tumours. The correlation coefficient obtained from the scatter plot of SUV and ADC exhibited a better diagnostic performance for differentiating high-grade from low/intermediate-grade tumours than any single conventional parameter alone.
High-grade tumours demonstrated a stronger inverse correlation between SUV and ADC than low/intermediate-grade tumours in the current study, as has been reported in a previous study investigating the PET/MR system [26]. Many studies utilizing ROI-based methods to investigate various types of malignant tumours have reported inverse correlations between SUV and ADC [16,17,18, 26]. In a study using an ROI-based method, Schmidt et al. [26] reported that there was a strong inverse correlation between SUV and ADC in lung cancers, and when analysed by a voxel-based method all five of the lung cancers exhibited an inverse correlation between SUV and ADC. Thus, an inverse correlation between SUV and ADC may be a good marker for high malignancy grade in soft tissue tumours, as for other malignant tumours such as those of the lung, breast, head and neck regardless whether the analytical method utilized is voxel-based or ROI-based.
Voxel-based comparisons of SUV and ADC may provide more precise assessments of tumour malignancy than ROI-based analysis, because ROI-based methods may compare SUV and ADC in different portions of any given tumour. This may be particularly relevant in tumours with a substantially heterogeneous internal structure. In contrast, voxel-based methods can compare SUV and ADC in identical voxels, and take internal heterogeneity of the tumour into consideration.
In principle, malignant tumours exhibit high cell proliferation and high glucose metabolism. A voxel with a low ADC suggestive of an increased number of tumour cells theoretically implies high FDG uptake reflecting high cellular metabolism, resulting in the inverse correlation between SUV and ADC. In contrast, interstitial tissues of soft-tissue tumours such as collagen fibres, mucin, calcification and haemorrhage exhibit a wide range of ADC values and lower glucose metabolism, and thus there may not be a strong inverse correlation between SUV and ADC. Therefore, we presume that malignant tumours comprised predominantly of cellular components will generally exhibit stronger inverse correlations between SUV and ADC than benign tumours comprised predominantly of interstitial components. In the present study, the correlation coefficient between SUV and ADC showed very high sensitivity (96.0%) for differentiating high-grade from low/intermediate-grade tumours. The inverse correlation could help classify soft-tissue tumours with lower FDG uptake such as myxoid liposarcoma into high-grade tumours (Fig. 5). However, the high sensitivity provided false-positives in some of low/intermediate-grade tumours such as giant cell tumour or schwannoma that could have more cellular components, which subsequently resulted in relatively lower specificity (60.0%) [2, 6].
In addition to an inherent heterogeneous structure of soft tissue tumours, necrosis and subsequent inflammation will occur as high-grade tumours grow. Therefore, quantifying the internal heterogeneity of soft-tissue tumours could be crucial for assessing their malignancy. Voxel-based analysis can be utilized for assessing the internal heterogeneity of soft-tissue tumours. Histogram analysis has provided an index for measuring tumour heterogeneity based on individual images [27,28,29]. However, it cannot be used to assess tumour heterogeneity via a combination of two image resources such as 18FDG-PET and ADC-mapping. Voxel-based analysis can provide information on internal heterogeneity based on SUV and ADC in the tumour via both visual and semi-quantitative assessments, in the form of scatter plots. The elliptical 95% area of bivariate normal distribution of SUV and ADC may be a good index to use to semi-quantify the degree of scatter in these plots. In the current study this index contributed to the determination of tumour malignancy, but the accuracy of such determinations was not higher than the accuracy of those derived from conventional SUVmax or the correlation coefficient of SUV and ADC in soft tissue tumours. This is probably because some of the low- or intermediate-grade tumours also contained heterogeneous cellular and interstitial tissue, which is common in soft tissue tumours. The use of the elliptical 95% area of bivariate normal distribution of SUV and ADC for the determination of tumour malignancy should be further investigated in other tumours such as those of the brain, head and neck, lung, liver and pancreas.
Multiparametric voxel-based analysis should incorporate precise co-registration between the two parametric images. Since the PET/MR system has been developed and introduced into the clinic, its usefulness has been widely argued. The direct voxel-based comparison of functional images in this study is one of the unique ways to use the PET/MR system. Despite recent advances in image fusion software, it is still difficult to retrospectively generate well-matched fusion images using DWI and PET images acquired with different machines separately. This may be attributed to many factors such as flex and rotation of extremities, body distortion from coil weight, and distortion of DWI images from single-shot EPI sequences. The PET/MR system, especially a fully-integrated scanner [30] could compensate for these problems. We detected minor misregistrations due to small motions by patients in this study as the scanner used was a sequential type, but these were easily corrected by a simple image registration with rigid transformation [21, 22]. High-resolution PET imaging with 23 mm resolution was used in this study, and the clear border of the lesion from the reduced partial volume effect also facilitated accurate registration, and the appropriate determination of tumour ROIs. Also, the use of zoomed DWI [19] instead of conventional DWI could reduce the image distortion associated with conventional DWI.
This study had some limitations. Firstly, there was some subject selection bias. Only patients with clinically suspected high-grade malignant tumour who were referred to our department underwent PET/MR scanning. Therefore, the numbers of low- and intermediate-grade tumours were relatively small. The difference in study population may have contributed to the relatively lower diagnostic performance of SUV and ADC alone in this study compared to previous studies [6, 7, 31]. However, the correlation coefficient for SUV and ADC could differentiate the two groups correctly in this study. Further study is necessary to investigate the differences between low- and intermediate-grade or between subtypes of high-grade tumours with increased number of subjects. Secondly, ADC values calculated via diffusion-weighted images of b values 0 and 800 may be affected by tissue perfusion [32]. ADC values might be overestimated in tumours with higher perfusion, but this should apply equally to each voxel. Moreover, although we avoided bulky fat tissue, minor fat tissue may have compromised ADC values. ADC values derived from voxels containing contaminating fat could not be correctly measured, because the signal intensity of fat tissue was too low to count on DWI images using the fat-suppression technique. To avoid such voxel fat contamination, voxels with ADC values less than 0.3 × 10−6 mm2/s were not incorporated into the scatter plots. Thirdly, SUVs measured on the PET/MR system could be underestimated compared to PET/CT [33]. SUV measurement was performed with the segmentation algorithm for attenuation correction in the PET/MR system, which cannot separate cortical bone from soft tissue [20]. In addition, unlike Dixon-based MR attenuation correction adopted by other vendors [30], the MR attenuation correction based on 3D-T1-weighted imaging used in this study did not separately segment fat tissue from soft tissue. This might have overestimated the SUV of the tumours. However, these factors are also universal to all measurements in this study, and would not affect our overall conclusions. Finally, histopathological correlations were difficult to determine because some low-grade tumours did not undergo total surgical resection and some high-grade tumours received heavy-particle radiotherapy. Further investigation of histopathological correlations should be performed.
In conclusion, voxel-based analysis of SUV and ADC with a PET/MR system may be useful for differentiating high-grade from low- or intermediate-grade soft tissue tumours.
References
Clark MA, Fisher C, Judson I, Thomas JM (2005) Soft-tissue sarcomas in adults. N Engl J Med 353:701–711
Fletcher CDM (2013) WHO Classification of tumours of soft tissue and bone: IARC Press
Fayad LM, Jacobs MA, Wang X, Carrino JA, Bluemke DA (2012) Musculoskeletal tumors: how to use anatomic, functional, and metabolic MR techniques. Radiology 265:340–356
De Schepper AM, De Beuckeleer L, Vandevenne J, Somville J (2000) Magnetic resonance imaging of soft tissue tumors. Eur Radiol 10:213–223
Zhao F, Ahlawat S, Farahani SJ et al (2014) Can MR imaging be used to predict tumor grade in soft-tissue sarcoma? Radiology 272:192–201
Charest M, Hickeson M, Lisbona R, Novales-Diaz JA, Derbekyan V, Turcotte R (2009) FDG PET/CT imaging in primary osseous and soft tissue sarcomas: a retrospective review of 212 cases. Eur J Nucl Med Mol Imaging 36:1944–1951
Bastiaannet E, Groen H, Jager PL et al (2004) The value of FDG-PET in the detection, grading and response to therapy of soft tissue and bone sarcomas; a systematic review and meta-analysis. Cancer Treat Rev 30:83–101
Schulte M, Brecht-Krauss D, Heymer B et al (2000) Grading of tumors and tumorlike lesions of bone: evaluation by FDG PET. J Nucl Med 41:1695–701
Aoki J, Watanabe H, Shinozaki T, Tokunaga M, Inoue T, Endo K (1999) FDG-PET in differential diagnosis and grading of chondrosarcomas. J Comput Assist Tomogr 23:603–8
Gibbs P, Liney GP, Pickles MD, Zelhof B, Rodrigues G, Turnbull LW (2009) Correlation of ADC and T2 measurements with cell density in prostate cancer at 3.0 Tesla. Investig Radiol 44:572–576
Koral K, Mathis D, Gimi B et al (2013) Common Pediatric Cerebellar Tumors: Correlation between Cell Densities and Apparent Diffusion Coefficient Metrics. Radiology 268:532–537
Del Grande F, Subhawong T, Weber K, Aro M, Mugera C, Fayad LM (2014) Detection of soft-tissue sarcoma recurrence: added value of functional MR imaging techniques at 3.0 T. Radiology 271:499–511
Dudeck O, Zeile M, Pink D et al (2008) Diffusion-weighted magnetic resonance imaging allows monitoring of anticancer treatment effects in patients with soft-tissue sarcomas. J Magn Reson Imaging 27:1109–1113
Wang X, Jacobs MA, Fayad L (2011) Therapeutic response in musculoskeletal soft tissue sarcomas: evaluation by MRI. NMR Biomed 24:750–763
Soldatos T, Ahlawat S, Montgomery E, Chalian M, Jacobs MA, Fayad LM (2016) Multiparametric assessment of treatment response in high-grade soft-tissue sarcomas with anatomic and functional MR imaging sequences. Radiology 278:831–840
Baba S, Isoda T, Maruoka Y et al (2014) Diagnostic and prognostic value of pretreatment SUV in 18F-FDG/PET in breast cancer: comparison with apparent diffusion coefficient from diffusion-weighted MR imaging. J Nucl Med 55:736–742
Regier M, Derlin T, Schwarz D et al (2012) Diffusion weighted MRI and 18F-FDG PET/CT in non-small cell lung cancer (NSCLC): does the apparent diffusion coefficient (ADC) correlate with tracer uptake (SUV)? Eur J Radiol 81:2913–2918
Preda L, Conte G, Bonello L et al (2016) Combining standardized uptake value of FDG-PET and apparent diffusion coefficient of DW-MRI improves risk stratification in head and neck squamous cell carcinoma. Eur Radiol 26:4432–4441
Sagiyama K, Watanabe Y, Kamei R, Baba S, Honda H (2016) Comparison of positron emission tomography diffusion-weighted imaging (PET/DWI) registration quality in a PET/MR scanner: Zoomed DWI vs Conventional DWI. J Magn Reson Imaging 43:853–858
Sagiyama K, Watanabe Y, Kamei R, Shinyama D, Baba S, Honda H (2016) An improved MR sequence for attenuation correction in PET/MR hybrid imaging. Magn Reson Imaging 34:345–352
Maes F, Collignon A, Vandermeulen D, Marchal G, Suetens P (1997) Multimodality image registration by maximization of mutual information. IEEE Trans Med Imaging 16:187–198
Viola P, Wells WM III (1997) Alignment by Maximization of Mutual Information. Int J Comput Vis 24:137–154
Helenius J, Soinne L, Perkio J et al (2002) Diffusion-weighted MR imaging in normal human brains in various age groups. AJNR Am J Neuroradiol 23:194–199
Maeda M, Maier SE, Sakuma H, Ishida M, Takeda K (2006) Apparent diffusion coefficient in malignant lymphoma and carcinoma involving cavernous sinus evaluated by line scan diffusion-weighted imaging. J Magn Reson Imaging 24:543–548
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Schmidt H, Brendle C, Schraml C et al (2013) Correlation of simultaneously acquired diffusion-weighted imaging and 2-deoxy-[18F] fluoro-2-D-glucose positron emission tomography of pulmonary lesions in a dedicated whole-body magnetic resonance/positron emission tomography system. Investig Radiol 48:247–255
Donati OF, Mazaheri Y, Afaq A et al (2014) Prostate cancer aggressiveness: assessment with whole-lesion histogram analysis of the apparent diffusion coefficient. Radiology 271:143–152
Pope WB, Kim HJ, Huo J et al (2009) Recurrent glioblastoma multiforme: ADC histogram analysis predicts response to bevacizumab treatment. Radiology 252:182–189
Burger IA, Vargas HA, Apte A et al (2014) PET quantification with a histogram derived total activity metric: superior quantitative consistency compared to total lesion glycolysis with absolute or relative SUV thresholds in phantoms and lung cancer patients. Nucl Med Biol 41:410–418
Muzic RF, DiFilippo FP (2014) PET/MRI – Technical Review. Semin Roentgenol 49:242–54
Costelloe CM, Chuang HH, Madewell JE (2014) FDG PET/CT of primary bone tumors. AJR Am J Roentgenol 202:W521–W531
Iima M, Le Bihan D (2016) Clinical intravoxel incoherent motion and diffusion MR imaging: past, present, and future. Radiology 278:13–32
Heusch P, Buchbender C, Beiderwellen K et al (2013) Standardized uptake values for [18F] FDG in normal organ tissues: comparison of whole-body PET/CT and PET/MRI. Eur J Radiol 82:870–876
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yuji Watanabe
Conflict of interest
The authors of this manuscript declare relationships with the following companies: Y. Watanabe and S. Kawanami: Bayer Healthcare Japan, Modest, Research Grant; Philips Electronics Japan, Modest, Research Grant.
Funding
This study received funding by JSPS KAKENHI Grant Number JP16K19827 and the Fukuoka Foundation for Sound Health Cancer Research Fund.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic
• performed at one institution
Rights and permissions
About this article
Cite this article
Sagiyama, K., Watanabe, Y., Kamei, R. et al. Multiparametric voxel-based analyses of standardized uptake values and apparent diffusion coefficients of soft-tissue tumours with a positron emission tomography/magnetic resonance system: Preliminary results. Eur Radiol 27, 5024–5033 (2017). https://doi.org/10.1007/s00330-017-4912-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4912-y