Abstract
Objectives
To evaluate the effectiveness of CT before TAVI using variable helical pitch (VHP) scanning and its diagnostic performance for coronary artery disease (CAD).
Methods
Sixty patients (84.4 ± 4.6 years) scheduled for TAVI underwent CT using VHP scanning with the contrast material (CM) volume calculated as scanning time × weight [kg] × 0.06 mL. Retrospective electrocardiography (ECG)-gated scanning was utilized to examine the thorax, and non-ECG-gated scanning of the abdomen immediately followed. We analyzed CT attenuation values of the coronary arteries, aorta, iliac and femoral arteries. The coronary CT angiography images were evaluated for the presence of stenosis (≥50 %); invasive coronary angiography served as a reference standard.
Results
The average attenuations of all of the arteries were greater than 400 HU. We could evaluate the peripheral access vessels and dimensions of the ascending aorta, aortic root, and aortic annulus in all patients. The average volume of CM was 38.7 ± 8.5 mL. On per-patient and vessel analysis, CT showed 91.7 % and 89.5 % sensitivity, and 91.3 % and 97.4 % negative predictive value (NPV).
Conclusions
CT using VHP scanning with an average CM volume of 38.7 mL is useful before TAVI and had a high sensitivity and NPV in excluding obstructive CAD.
Key Points
• TAVI-planning CT using variable helical pitch (VHP) scanning is useful.
• The average volume of contrast material was 38.7 ± 8.5 mL.
• The average attenuations of all the arteries were >400 HU.
• This CT had a high sensitivity and NPV for excluding obstructive CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transcatheter aortic valve implantation (TAVI) has been increasingly common and accepted as an alternative to surgical aortic valve implantation in the elderly and high-risk patients [1–3].
Computed tomography (CT) imaging before TAVI is necessary to evaluate the access route (transapical or transfemoral), aortic annual dimensions, aortic valve structure and calcifications [4]. We can also predict the orthogonal view on the aortic annuals plane called the perpendicular view. CT protocols before TAVI vary and depend on the CT scanner. In the guidelines of CT imaging prior to TAVI [4], the aortic root must be imaged with electrocardiogram (ECG) gating to allow for motion-free imaging. However, it is not necessary to image the entire aorta and iliofemoral arteries in ECG gating. For these sections, non-gated acquisitions may be preferable because of lower radiation exposure and because of faster volume coverage that requires lower volumes of iodinated contrast material (CM). The volume of CM is of concern in many candidates for TAVI because the candidates frequently have impaired renal function [4]. Previous studies have reported that the chronic kidney disease (CKD) stage before TAVI affects the clinical outcome [5, 6]. Therefore, the volume of CM should be minimized as low as possible in CT imaging before TAVI.
Recently, a promising CT technique of variable helical pitch (VHP) scanning was introduced for clinical use. VHP scanning allows a seamless change of pitch during one continuous acquisition and enables the combination of ECG-gated and non-ECG-gated acquisitions within one scan. Due to the seamless change of pitch, reduction in CM is expected.
On another front, TAVI candidates are elderly and have a high prevalence of coronary artery disease (CAD) [7]. A high NPV (93.8 %) for excluding the obstructive CAD of TAVI candidates with dual-source CT system has been reported in a previous study [8]. If we also show a high NPV in CT imaging before TAVI using VHP scanning, the need for pre-procedural invasive coronary angiography (CAG) in patients who are CT negative for CAD may be reduced, and the total volumes of CM for such patients can be minimized. Furthermore, the overall cost for TAVI is still higher than that for surgical aortic valve replacement, and the high cost of care in TAVI patients is an increasing problem [9]. The reduction of invasive CAG as a negative result of TAVI planning CT can lead to a reduction of the total cost for TAVI.
The purpose of this study was to evaluate the effectiveness of CT before TAVI using VHP scanning and its diagnostic performance for CAD.
Materials and methods
Study population
Ninety patients with severe symptomatic AS who were receiving TAVI planning CT and underwent TAVI between April 4, 2014, and March 31, 2015, were considered for inclusion in this study. Patients were excluded if they were scanned with protocols that differed from the VHP scanning protocol described below (n = 30). Thus, a total of 60 patients were included in the final analysis. The patients comprised 17 men and 43 women with a mean age of 84.4 ± 4.6 years, a mean height of 148.7 ± 8.3 cm, a mean body weight of 49.4 ± 10.2 kg and a mean body mass index (BMI) of 22.2 ± 3.6 kg/m2. The excluded patients comprised 8 men and 22 women with a mean age of 83.5 ± 4.3 years, a mean height of 147.2 ± 9.1 cm, a mean body weight of 48.6 ± 10.9 kg and a mean BMI of 22.3 ± 4.1 kg/m2. Notably, there was no significant difference of the gender, age, height, weight, or BMI (P = 0.8676, 0.2585, 0.6405, 0.8338, and 0.7320, respectively, using a chi-square test for gender and a Mann–Whitney U test for age, height, weight and BMI) between the included and excluded patients. All of the included patients underwent both CT and invasive CAG within 2 months before the TAVI procedure and underwent the TAVI procedure using a balloon-expandable Edwards SAPIEN XT heart valve (Edwards Lifesciences, Irvine, CA, USA).This study was approved by our institutional review board, and written informed consent was obtained from each participant.
CT protocol
All CT examinations were performed using a 320-detector row CT scanner (Aquilion ONE/ViSION Edition, Toshiba Medical Systems, Otawara, Japan). No premedication for heart rate control or vasodilatation was added for CT acquisition. CT examinations were performed using the following parameters: peak tube voltage, 100 kV; tube current, 185–580 mA (determined based on a pre-specified BMI protocol); rotation speed, 0.275 s; and slice collimation, 0.5 × 100 mm. We used VHP scanning, which allows a seamless change in the scan pitch during one continuous acquisition and enables a combination of gated and non-gated acquisitions within one scan. A pitch of 0.15–0.17 was chosen for ECG-gated thoracic imaging depending on the patient’s heart rate, and 0.87 was used for non ECG-gated abdominal scans. Retrospective ECG-gated scanning was utilized to examine the thorax and covered the structures from approximately 2 cm above the apex to the base of the heart. Non-ECG-gated scanning of the abdomen and pelvis (to the level of the proximal thigh) followed the thorax scan without delay (Fig. 1). A double-channel injection system (Dual Shot; Nemoto, Tokyo, Japan), equipped with a high-pressure-resistant extension tube (Injector tube; Top, Tokyo, Japan), a 22G indwelling needle (Supercath; Medikit, Tokyo, Japan) and right antecubital venous access were used. The volume of CM (Iopamiron 370 mg/mL iodine concentration; Bayer, Osaka, Japan: or 350 mg/mL) was determined by the scanning time (approximately 13 s, depending on the patient’s habitus and heart rate) × weight × 0.06 mL. CM was injected at a rate of the weight × 0.06 mL/s followed by 20 mL of the saline solution at a rate of the weight × 0.06 mL/s. Scanning was automatically started with a 3-s delay after the attenuation of a region of interest (ROI) placed in the ascending thoracic aorta reached the threshold of +150 Hounsfield units (HU).
Before contrast-enhanced CT scanning, all of the patients underwent unenhanced CT with prospective ECG gating for coronary artery calcium scoring.
Invasive CAG
Invasive CAG was performed by experienced cardiologists using standard techniques and the acquisition of standard projection planes. CAG images were classified into 16 segments according to the AHA classification. Stenosis severity was determined via clinical studies using quantitative coronary angiography. Greater than or equal to 50 % stenosis of each vessel was rated as positive.
Image analysis
Continuous 1-mm-thick CT images for the evaluation of the access route (from above the apex to the proximal thigh) were reconstructed using adaptive iterative dose reduction 3D (AIDR 3D) [10]. We analyzed CT attenuation values of the coronary arteries (the proximal portions of the left main trunk, left anterior descending artery, left circumflex branch and right coronary artery), aortic root, aortic arch, descending aorta, aorta at the diaphragm level, abdominal aorta at the renal artery level, aortic bifurcation, common iliac arteries, external iliac arteries and common femoral arteries.
For evaluation of the heart, 0.5-mm-thick CT images were reconstructed at 30 % (for aortic valve ring assessment), 45 % (end-systole), and 75 % (mid-diastolic) of the cardiac cycle. We did not use ECG editing. All coronary CT data were analyzed by two radiologists (with 5 and 3 years of experience in coronary CT angiographic imaging) in consensus for the presence and degree of stenosis for the left main trunk, left anterior descending artery, left circumflex branch and right coronary artery. Readers were blinded to the results of invasive CAG. Axial CT images and multi-planar reconstruction (MPR) images were used for coronary CT evaluation. The radiologists evaluated images for the presence of ≥50 % stenosis; invasive coronary angiography served as the reference standard. When a vessel was not evaluable because of motion artifacts (increased heart rate or arrhythmia, and incomplete breath holding) or heavy calcifications, it was classified as non-diagnostic and treated as positive for stenosis (≥50 %). We calculated the sensitivity, specificity, PPV and NPV for per vessel and per patient. We also calculated the diagnostic performance of TAVI-planning CT excluding non-diagnostic vessels resulting from heavy calcification and that of TAVI-planning CT excluding all non-diagnostic vessels. We assumed a high NPV (>90 %) for excluding significant coronary artery stenosis, consistent with a previous study [8].
The Agatston method for quantification of the coronary artery calcium level was used for the calculation of the coronary artery calcium scores on unenhanced CT [11].
Statistical analysis
The variables were expressed as the means ± standard deviation (SD). The normality of the CT attenuation values was assessed using the Shapiro–Wilk test.
Results
The clinical and CT baseline characteristics are summarized in Table 1.
The average CT scanning time from above the apex to the proximal thigh was 13.04 ± 0.99 s (range: 10.2–16.5 s), and the average volume of CM was 38.7 ± 8.5 mL (range: 25.9–60.1 mL). There was no patient with contrast-induced acute kidney injury. The average attenuations of all of the arteries were more than 400 HU (Table 2). All of the minimum CT attenuations of the arteries were >236.5 HU. We could evaluate the peripheral access vessels and dimensions of the ascending aorta, aortic root, and aortic annulus in all of the patients (Fig. 2). The procedural success rate was 100 % (transfemoral in 53 cases; transapical in 7 cases).
A 76-year-old female TAVI candidate with a height of 151 cm, a body weight of 50 kg, and a body mass index of 21.9 kg/m2. A. Volume-rendering image; B. Maximum intensity projection image; C. Curved planar reformation (CPR) image; D. Straightened CPR image; E. Cross-section image. The images were obtained using 40.5 ml of contrast materials
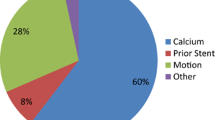
Two hundred forty coronary vessels in 60 patients were analyzed for the evaluation of CAD. In invasive coronary angiography as the reference standard, 15.8 % (38/240) of the coronary vessels were positive (stenosis ≥50 %), and 40.0 % (24/60) of patients were positive. Eighteen vessels (7.5 %) in 13 patients were classified as non-diagnostic and treated as positive for stenosis (≥50 %; motion artifacts due to increased heartrate or arrhythmia; 9 vessels, 8 patients, motion artifacts due to incomplete breath holding; 5 vessels, 3 patients, heavy calcification; 4 vessels, 3patients). On per-patient analysis, TAVI-planning CT had a sensitivity of 91.7 %, a specificity of 58.3 %, a PPV of 59.5 %, and an NPV of 91.3 % (Table 3). On per-vessel analysis, TAVI-planning CT had a sensitivity of 89.5 %, a specificity of 75.2 %, a PPV of 40.5 %, and an NPV of 97.4 % (Table 3). The diagnostic performances of TAVI-planning CT excluding non-diagnostic vessels resulting from heavy calcification and that excluding all non-diagnostic vessels are shown in Tables 4 and 5, respectively. An example of a TAVI candidate is shown in Fig. 3. We misdiagnosed two vessels (#4AV and #9) as non-stenosis (<50 %; percutaneous coronary intervention [PCI] was not performed for these vessels).
The mean calcium score was 1018.1 ± 1130.6. The mean CTDI volume was 19.6 ± 3.0 mGy, and the mean DLP was 1281.6 ± 195.7 mGy・cm. The effective dose was estimated as 19.1 ± 2.9 mSv, determined using the DLP measurements and appropriate normalized coefficients reported in a previous study concerning trunk CT (0.015 mSv/(mGy cm)) [12].
Discussion
Our study showed that CT imaging before TAVI using VHP scanning with an average volume of CM (38.7 ± 8.5 mL) is useful for a TAVI procedure that is accurate and safe, maintaining all of the average CT attenuations of the coronary and access route arteries greater than 400 HU; there was no patient with contrast-induced acute kidney injury after CT, and the procedural success rate was 100 %. In the previous study, the optimal vascular attenuation for stenosis detection in coronary CT angiography was thought to be approximately 350–400 HU [13, 14], and lower attenuation leads to the overestimation of stenosis [15]. Therefore, our study would have sufficiently good CT attenuation to evaluate all of the arteries. Two other previous studies have reported CT imaging before TAVI using dual-source CT systems with an average CM volume of 20 mL [16] and 40 mL [17]; however, to the best of our knowledge, this is the first detailed study conducted to demonstrate the usefulness of a single-source CT system using the VHP scan technique. Additionally, these two previous studies using dual-source CT systems did not refer to the diagnostic performance for obstructive CAD.
Our study revealed that TAVI-planning CT with VHP scanning had a high NPV for obstructive CAD. If we can exclude coronary artery stenosis by TAVI-planning CT and can avoid unnecessary invasive coronary angiography (23/60 [38 %] in the present study) in TAVI candidates, we could further reduce the total cost as well as the total volume of CM and radiation exposure. One previous study [8] has reported that TAVI-planning CT had a sensitivity of 98.6 %, a specificity of 55.6 %, a PPV of 85.7 %, and an NPV of 93.8 % on per-patient analysis for the evaluation of coronary artery stenosis, a finding that is almost equal to the values in our study, although the mean calcium scores in our study (1018.1) were numerically higher than those of this previous study (722). However, in the previous study, the total volume of CM was 60 mL (triphasic protocol: 40 mL of CM + 30 mL of 2:1 CM-to-saline mixture + 40 mL of saline chaser), and this value was greater than that in our study. We misdiagnosed two vessels (#4AV and #9) as non-stenosis (<50 %). However, PCI was not performed for these vessels. PCI for AS patients was usually performed only for severely stenotic lesions in proximal coronaries that subtend a large area of myocardium at risk [7]. Therefore, our misdiagnoses would not be so problematic.
The per vessel specificity, per patient specificity, per vessel PPV, and per patient PPV values in the present study were 75.2 %, 58.3 %, 40.5 %, and 59.5 %, respectively. Excluding vessels resulting from heavy calcification, the values were 76.4 %, 61.8 %, 41.3 %, and 61.8 %, respectively. In addition, excluding all non-diagnostic vessels (resulting from heavy calcification + motion artifacts), the values increased to 81.3 %, 70.0 %, 47.0 %, and 62.5 %. Therefore, the lower specificity and PPV in our study would be due to not only heavy calcification but also motion artifacts (increased heart rate, arrhythmia and incomplete breath holding). The TAVI candidates were elderly, and several patients found it difficult to hold their breath. Furthermore, the heart rates of the AS patients were difficult to control, even using β-blocker.
Because retrospective ECG-gated scanning for thoracic imaging was utilized, the radiation dose of the CT protocol in our study was higher than that of previous studies using dual-source CT [16, 17] that did not evaluate coronary artery stenosis. In the SCCT guideline of TAVI-planning CT, imaging of the aortic root and annulus in systole is said to be preferable over diastole because of the dynamic changes of the annulus and slightly larger annular sizes noted in systole [18, 19]. On the other hand, coronary imaging in mid-diastole is considered to be preferable over systole except that motion artifact has occurred. Therefore, if we evaluate coronary arteries in TAVI CT, it is necessary to acquire both the systole and diastole phases. In addition, if retrospective ECG-gated scanning is utilized, we can analyze both systolic and diastolic coronary CT angiography images. Furthermore, given the common advantage of the age of the patients being considered for TAVI, radiation exposure may be a lesser concern.
A lower kV setting or low keV monochromatic image is also useful for reducing CM and yielding higher HUs during scanning in TAVI planning CT [20, 21]. However, a lower kV setting increases the image noise, and incidental findings might be overlooked. In a previous report, significant non-cardiac findings were commonly observed in patients referred to TAVI planning CT [22]. Therefore, we did not use 80 kVp but instead used a 100-kVp setting in the present study.
There are some limitations in our study. First, the prevalence of stenosis of coronary arteries in our study was 40 %, and the NPV of CT coronary angiograms might be changed according to the prevalence of the study population. However, the previous study reported that the prevalence of CAD in AS patients was 40–75 % [7], and the prevalence of CAD in our study was within the range. Second, we used a 320-detector-row CT scanner with VHP scanning, and the diagnostic performance in our study may not be generalizable to other acquisition protocols and CT systems. However, we used a single-source CT system; if it is possible to use a scan protocol similar to that of the VHP scan in our study (currently, there are no other vendors offering VHP scan mode.), our results could be generalizable to many other single-source CT systems.
Conclusion
CT imaging using VHP scanning is useful before TAVI with an average CM volume of 38.7 mL in the restricted cohort examined in the present study, thus showing high sensitivity and NPV in excluding obstructive CAD.
Abbreviations
- CAD:
-
Coronary artery diseasec
- CAG:
-
Coronary angiography
- CM:
-
Contrast material
- CT:
-
Computed tomography
- ECG:
-
Electrocardiogram
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- TAVI:
-
Transcatheter aortic valve implantation
References
Webb JG, Wood DA (2012) Current status of transcatheter aortic valve replacement. J Am Coll Cardiol 60:483–492
Leon MB, Smith CR, Mack M et al (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Smith CR, Leon MB, Mack MJ et al (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364:2187–2198
Achenbach S, Delgado V, Hausleiter J, Schoenhagen P, Min JK, Leipsic JA (2012) SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr 6:366–380
Yamamoto M, Hayashida K, Mouillet G et al (2013) Prognostic value of chronic kidney disease after transcatheter aortic valve implantation. J Am Coll Cardiol 62:869–877
Yamamoto M, Hayashida K, Mouillet G et al (2013) Renal function-based contrast dosing predicts acute kidney injury following transcatheter aortic valve implantation. JACC Cardiovasc Interv 6:479–486
Goel SS, Ige M, Tuzcu EM et al (2013) Severe aortic stenosis and coronary artery disease--implications for management in the transcatheter aortic valve replacement era: a comprehensive review. J Am Coll Cardiol 62:1–10
Harris BS, De Cecco CN, Schoepf UJ et al (2015) Dual-source CT imaging to plan transcatheter aortic valve replacement: accuracy for diagnosis of obstructive coronary artery disease. Radiology 275:80–88
Toggweiler S (2014) How to reduce costs in transcatheter aortic valve implantation. Open Heart 1:e000203
Yamada Y, Jinzaki M, Hosokawa T et al (2012) Dose reduction in chest CT: comparison of the adaptive iterative dose reduction 3D, adaptive iterative dose reduction, and filtered back projection reconstruction techniques. Eur J Radiol 81:4185–4195
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
McCollough C, Cody D, Edyvean S et al (2008) The measurement, reporting, and management of radiation dose in CT. Rep AAPM Task Group 23:1–28
Fei X, Du X, Yang Q et al (2008) 64-MDCT coronary angiography: phantom study of effects of vascular attenuation on detection of coronary stenosis. AJR Am J Roentgenol 191:43–49
Hausleiter J, Meyer TS, Martuscelli E et al (2012) Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: the multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc Imaging 5:484–493
Cademartiri F, Maffei E, Palumbo AA et al (2008) Influence of intra-coronary enhancement on diagnostic accuracy with 64-slice CT coronary angiography. Eur Radiol 18:576–583
Azzalini L, Abbara S, Ghoshhajra BB (2014) Ultra-low contrast computed tomographic angiography (CTA) with 20-mL total dose for transcatheter aortic valve implantation (TAVI) planning. J Comput Assist Tomogr 38:105–109
Wuest W, Anders K, Schuhbaeck A et al (2012) Dual source multidetector CT-angiography before Transcatheter Aortic Valve Implantation (TAVI) using a high-pitch spiral acquisition mode. Eur Radiol 22:51–58
Toggweiler S, Gurvitch R, Leipsic J et al (2012) Percutaneous aortic valve replacement: vascular outcomes with a fully percutaneous procedure. J Am Coll Cardiol 59:113–118
Rodes-Cabau J, Webb JG, Cheung A et al (2010) Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk: acute and late outcomes of the multicenter Canadian experience. J Am Coll Cardiol 55:1080–1090
Kok M, Turek J, Mihl C et al (2015) Low contrast media volume in pre-TAVI CT examinations. Eur Radiol 1–10
Dubourg B, Caudron J, Lestrat J-P et al (2014) Single-source dual-energy CT angiography with reduced iodine load in patients referred for aortoiliofemoral evaluation before transcatheter aortic valve implantation: impact on image quality and radiation dose. Eur Radiol 24:2659–2668
Staab W, Bergau L, Lotz J, Sohns C (2014) Prevalence of noncardiac findings in computed tomography angiography before transcatheter aortic valve replacement. J Cardiovasc Comput Tomogr 8:222–229
Acknowledgments
The scientific guarantor of this publication is Masahiro Jinzaki. Masahiro Jinzaki received a grant from Toshiba Medical Systems Japan. The remaining authors (Shunsuke Matsumoto, Yoshitake Yamada, Masahiro Hashimoto, Teppei Okamura, Minoru Yamada, Fumiaki Yashima, Kentaro Hayashida, and Keiichi Fukuda) have no financial disclosures to make and had complete unrestricted access to the study data at all stages of the study. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper.
Institutional review board approval was obtained. Written informed consent was obtained from all patients in this study. No study subjects or cohorts have been previously reported. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Shunsuke Matsumoto and Yoshitake Yamada contributed equally to this work.
Rights and permissions
About this article
Cite this article
Matsumoto, S., Yamada, Y., Hashimoto, M. et al. CT imaging before transcatheter aortic valve implantation (TAVI) using variable helical pitch scanning and its diagnostic performance for coronary artery disease. Eur Radiol 27, 1963–1970 (2017). https://doi.org/10.1007/s00330-016-4547-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4547-4