Abstract
Objectives
To compare soft-tissue changes after total hip arthroplasty with posterior, direct-lateral, anterolateral, or anterior surgical approaches.
Methods
MRI of 120 patients after primary total hip arthroplasty (30 per approach) were included. Each MRI was assessed by two readers regarding identification of surgical access, fatty muscle atrophy (Goutallier classification), tendon quality (0 = normal, 1 = tendinopathy, 2 = partial tear, 3 = avulsion), and fluid collections. Readers were blinded to the surgical approach.
Results
Surgical access was correctly identified in all cases. The direct lateral approach showed highest Goutallier grades and tendon damage for gluteus minimus muscle (2.07-2.67 and 2.00-2.77; p = 0.017 and p = 0.001 for readers 1 and 2, respectively) and tendon (2.30/1.67; p < 0.0005 for reader 1/2), and the lateral portion of the gluteus medius tendon (2.77/2.20; p < 0.0005 for reader 1/2). The posterior approach showed highest Goutallier grades and tendon damage for external rotator muscles (1.97-2.67 and 1.57-2.40; p < 0.0005-0.006 for reader 1/2) and tendons (1.41-2.45 and 1.93-2.76; p < 0.0005 for reader 1/2). The anterolateral and anterior approach showed less soft tissue damage. Fluid collections showed no differences between the approaches.
Conclusions
MRI is well suited to identify surgical approaches after THA. The anterior and anterolateral approach showed less soft tissue damage compared to the posterior and direct lateral approach.
Key Points
• Identification of the surgical approach is well possible with MR imaging.
• Anterolateral/anterior approaches show less soft-tissue damage compared to lateral/posterior approaches.
• Posterior approaches show marked damage to external rotator tendons and muscles.
• After direct lateral approaches the gluteus minimus tendon/muscle show severe damage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of total hip arthroplasty (THA) increased over the last decade in most developed countries [1]. Because of an increasing elderly population and higher rate of obesity, use of THA is expected to increase even more [2]. The classic surgical approaches for THA are the posterior approach [3], the direct lateral approach [4], the anterolateral approach [5], and the anterior approach [6]. The soft tissue around the hip in THA has gained more attention with the development of minimally invasive soft tissue sparing surgical approaches. The soft tissue is not only important in regards to the surgical technique, but also in the work-up of patients with a painful hip arthroplasty [7]. First imaging step in evaluation of patients with hip pain after THA are radiographs [8]. Radiographs are useful to assess the bone and the prosthesis, but lack of visualization of soft tissue around the hip. Ultrasound can be a useful technique when assessing the postoperative hip for fluid collections, joint effusion, and abductor tendons [9]. With the development of advanced MRI techniques for metal artefact reduction, assessment of patients after THA has become feasible [10, 11]. MRI of hip arthroplasty can be used to assess complications associated with the prosthesis such as osteolysis [7], infection [12], and assessment of abductor tendons and muscles [13]. In clinical routine, often no information on the surgical approach is available when assessing MRI of patients with a total hip prosthesis. Therefore, the purpose of our study was to assess if it is possible to correctly identify the surgical approach by MR imaging and to compare damage to soft tissue around the hip joint after THA between the different surgical approaches to establish soft tissue damage profiles for each surgical approach on MRI.
Materials and methods
This retrospective study was approved by the local ethics committee. The following four surgical approaches for total hip arthroplasty were evaluated: posterior approach, direct lateral approach, anterolateral approach, and anterior approach.
Patients
The Picture Archiving and Communication System (PACS) was searched by one author for all MR hip examinations between January 2012 and March 2014 that mentioned prosthesis or total hip arthroplasty in the report. This search resulted in 238 patients. The following inclusion criteria were then applied: Patients were examined because of hip pain after primary total hip arthroplasty (THA) with no explanation for the pain on clinical examination and radiographs, information on the type of surgical approach available by clinical notes or surgical reports, no revision surgeries, dedicated hip imaging protocol (see MRI protocol), and MR imaging at least 3 months postoperatively. Metal-on-metal prostheses were included (only two patients). Patients with periprosthetic infections were excluded. Of the initial 238 patients, 105 were excluded for not meeting these criteria: 57 patients with no data on surgical approach because index surgery was performed at external institutions, 35 patients with revision surgeries, three patients with MR imaging within the first 3 months after surgery, three patients femoral head resurfacings, one patient with a tumour prosthesis, and three patients with periprosthetic infections.
Therefore, 133 patients were eligible. The 30 consecutive most current MR studies in each approach group were selected for the analysis.
MRI protocol
Examinations were performed on a 1.5 Tesla MR-scanner (Magnetom Avanto, Siemens, Erlangen, Germany). The imaging protocol consisted of a transverse STIR with an optimized inversion pulse [14] to reduce metal artefacts (TE/TR 31/4000 ms; slice thickness 7 mm; matrix 269 × 384; field-of-view 18 cm, readout bandwidth 450 Hz/pixel), a coronal STIR with slice-encoding for metal artefact correction (SEMAC) [11] (TE/TR 31/4000 ms; slice-thickness 4 mm; matrix 307 × 384; field-of-view 24 cm; slice-encoding steps 10, readout bandwidth 780 Hz/pixel), a coronal T2-weighted high-bandwidth sequence (TE/TR 58/4000 ms; slice-thickness 4 mm; matrix 282 × 512; field-of-view 22 cm; readout bandwidth 390 Hz/pixel), a transverse T1-weighted high-bandwidth sequence (TE/TR 8.6/600; slice-thickness 6 mm; matrix 410 × 512, field-of-view 20 cm, readout bandwidth 425 Hz/pixel), and a sagittal T1-weighted high-bandwidth sequence (TE/TR 7.3/550 ms; slice-thickness 4 mm; matrix 320 × 320; field-of-view 20 cm; readout bandwidth 435 Hz/pixel).
MRI assessment
A random number was assigned to each MR examination (Microsoft Excel, Version 2010, Microsoft Corporation, Redmond, WA, USA) and the MR examinations were assessed in an ascending order (with a random distribution of the different surgical approaches). All MR examinations were assessed by two musculoskeletal radiologists separately (C.A. and R.S.* - with 1 year and 5 years of experience in musculoskeletal imaging) after an initial training session. Both readers were blinded to the surgical approach. The surgical approach was assessed on MR images and categorized by both readers into either posterior, direct lateral, anterolateral, or anterior approach. To identify the surgical approach, scarring of soft tissue and susceptibility artefacts along the four potential surgical approaches on all available sequences were used as imaging criteria.
-
Muscles - Fatty atrophy of the following muscles was assessed using the Goutallier classification [15] (grade 0 = no fat; grade 1 = few fatty streaks; grade 2 = <50 % fat; grade 3 = 50 % fat, grade 4 = >50 % fat): iliopsoas, gluteus minimus (anterior, mid, and posterior portion), gluteus medius (anterior, mid, and posterior portion), gluteus maximus, tensor fasciae latae, piriformis, internal and external obturator, and quadratus femoris. Fatty atrophy was assessed on coronal T2-weighted, transverse T1-weighted, and sagittal T1-weighted images, depending on which plane best to show the muscle’s cross-section. For obliquely running muscles, multiple planes were taken into consideration before grading fatty atrophy.
-
Tendons - The following tendons were assessed: the hip abductor tendons (gluteus minimus, lateral and superoposterior portion of the gluteus medius) and hip external rotator tendons (piriformis, internal and external obturator tendon). A semi-quantitative tendon damage score was used: 0 = normal, 1 = tendinopathy, 2 = partial tear, 3 = non-anatomic insertion (complete tear/surgical detachment/osseous avulsion), with higher scores indicating higher tendon damage.
-
Fluids - In the periarticular soft tissue, extrabursal fluid collections were noted. Presence or absence of fluid within the trochanteric bursa and iliopsoas bursa was noted. Joint fluid around the prosthetic joint (joint effusion) was assessed on fluid sensitive sequences (detectable or undetectable).
-
Fascia lata defects - Defects in the fascia lata were assessed on transverse images and the length of the defect was measured in mm. Only large defects defined as ≥10 mm were counted.
-
Nerves - The femoral nerve, the sciatic nerve and the lateral femoral cutaneous nerve were assessed for scarring around the nerve, for the presence of nerve disruption, and presence of neuromas.
Statistics
Descriptive statistics were applied. Kruskal-Wallis test was applied to assess differences between the four approaches regarding fatty muscle degeneration and tendon damage score, p < 0.05 indicating a statistically significant difference. The approach with the highest mean tendon or muscle damage was compared to each other approach separately with Mann-Whitney U tests, with a threefold Bonferroni-adjusted p-value for tthese sub-analyses (p-values <0.01667). Differences between the four approaches regarding fluid collections, fluid within the trochanteric bursa, fluid within the iliopsoas bursa, and detectable joint effusion were assessed using a Chi-square test for independence. Post-hoc testing was performed with adjusted standardized residual analysis [16] with an eightfold Bonferroni-adjusted p-value (p < 0.006). Interreader agreement for the surgical approach detection, extrabursal fluid collections, fluid within the trochanteric and iliopsoas bursa, and detectable joint effusion was calculated using Kappa statistics. For these calculations IBM SPSS Statistics Version 22 (IBM Corp., Armonk, NY, USA) was used. Interreader agreement for fatty muscle degeneration and tendon damage score was assessed using linear weighted Kappa statistics using MedCalc Statistical Software version 14.12.0 (MedCalc Software bvba, Ostend, Belgium).
Results
Patient characteristics are shown in Table 1. All MRI examinations of these patients were acquired between January 2011 and March 2014.
All surgical approaches were correctly identified by both readers (Kappa k = 1.0), meaning 100 % agreement.
A comprehensive overview of the detailed results for changes in fatty muscle atrophy, tendon damage, fluid collections, bursae, and detectable joint effusions are given in Tables 2, 3, 4 and 5 and Figs. 2 and 4.
In the following paragraphs individual damage profiles are presented.
-
Posterior approach (Fig. 1)
Fig. 1 65-year-old woman 10 years after primary hip arthroplasty with gluteal pain. Transverse T1-weighted image (a) and a schematic illustration (b) of the posterior approach (white arrows (a), red arrow (b)). There are multiple small susceptibility artefacts along the posterior approach. As the external rotator tendons are released from the trochanter during surgery we commonly found marked damage to the external rotator tendons and muscles with the posterior approach - exemplary shown as fatty atrophy (Goutallier grade 2) of the internal obturator muscle (white open arrow in (a) and black/white striped in (b)
-
Muscles - For both readers, patients with a posterior approach showed statistically significantly higher fatty infiltration of the external rotator muscles (piriformis, internal and external obturator, and quadratus femoris muscle) compared to the other approaches (Table 2). Compared to each other approach individually, the piriformis muscle, the internal obturator muscle, the external obturator muscle, and the quadratus femoris muscle showed statistically significantly higher Goutallier grades with the posterior approach(p < 0.0005-0.010 for both readers). Two exceptions were the piriformis muscle for the posterior approach compared with the direct lateral approach (p = 0.162) and the quadratus femoris muscle, also compared with the direct lateral approach due to Bonferroni adjustment (p = 0.024), both for reader 2.
-
Tendons - Damage to the external rotator tendons was markedly higher with the posterior approach compared to the other approaches individually (p < 0.0005-0.001 for reader 1, and p < 0.0005-0.017 for reader 2) (Figs. 1 and 2). Non-anatomic insertion were found in 22/30 piriformis tendons, 21/30 internal obturator tendons, and 8/30 external obturator tendons by reader 1 (26/30, 25/30, and 14/30, respectively, for reader 2).
Fig. 2 3D bars represent mean tendon damage score for the external rotator tendons for each surgical approach for reader 1 (a) and reader 2 (b). There was a statistically significant difference between the surgical approaches with highest damage to the external rotator tendons found for the posterior approach (p < 0.0005 for both readers and each muscle), compared to the other approaches. On x-axis 1 = posterior (plum), 2 = direct lateral (green), 3 = anterolateral (teal), 4 = anterior (orange). P = piriformis tendon, IO = internal obturator tendon, EO = external obturator tendon
-
Fluids - Fluid collections generally were uncommon for all approaches. However, in the peritrochanteric region fluid collections were only found with the posterior approach, except in one patient with a direct lateral approach (Table 3). Fluid within the trochanteric bursa was found in 8/30 patients by reader 1, and 7/30 for reader 2 (Table 4). Fluid within the iliopsoas bursa was less common compared to the other approaches, although not statistically significantly different (Table 4). Joint effusion was commonly detected by both readers, but without a statistically significant difference compared to the other approaches (Table 5).
-
Other findings - No defects in the fascia lata of 10 mm width or more were found for the posterior approach. No damage to nerves was detected.
-
-
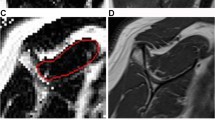
Direct lateral approach (Fig. 3)
Fig. 3 74-year-old woman 15 months after primary hip arthroplasty with hip pain. The direct lateral approach is well visible (white arrows) on the transverse T1-weighted image (a) and shown by the red arrow on the schematic illustration (b). There is a large gap in the fascia lata (*). There is a defect in the gluteus minimus muscle along the surgical approach (white arrows, a), which should not be mistaken as fatty infiltration of the muscle. On a more cephalad section (c) the gluteus medius muscle (white open arrow) shows only minor fatty infiltration (Goutallier grade 1). The gluteus minimus muscle (white arrowhead) shows more fatty infiltration (Goutallier grade 2). For the direct lateral approach, commonly the most severely damaged structure was the gluteus minimus muscle (black/white striped (b)) and tendon
-
Muscles - With the direct lateral approach, the mid and posterior portion of the gluteus minimus muscle showed higher Goutallier grades (both readers) compared to the other approaches (Table 2, Fig. 3). Post hoc analysis showed that Goutallier grades in the mid portion of the gluteus minimus muscle were statistically significantly higher compared to the posterior and anterior approach (p < 0.0005-0.010, both readers), but not for the anterolateral approach (p = 0.301 and p = 0.085, for readers 1 and 2, respectively). The posterior portion of the gluteus minimus muscle showed statistically significant higher Goutallier grades compared to the anterior approach (p = 0.002 and p = 0.012 for readers 1 and 2, respectively), but not compared to the anterolateral approach (p = 0.043 due to Bonferroni-adjustment, and p = 0.115). Compared to the posterior approach Goutallier grades were statistically significantly higher only for reader 1 (p = 0.005 for reader 1, p = 0.063 for reader 2). The anterior portion of the gluteus minimus muscle showed a high degree of fatty degeneration with all approaches. The gluteus medius muscle (all three portions) showed no statistically significant difference between the approaches regarding fatty degeneration (Table 2).
-
Tendons - The gluteus minimus tendon showed statistically significantly higher damage scores compared to the other approaches separately (p < 0.0005 for all comparisons and both readers) (Fig. 4). Also, damage to the lateral portion of the gluteus medius tendon was higher with the direct lateral approach (p < 0.0005 for all comparisons and both readers, while the mean damage score to the superoposterior insertion of the gluteus medius tendon was low and comparable to the other approaches (Fig. 4).
Fig. 4 3D-Bars represent mean damage score for the abductor tendons for each surgical approach for reader 1 (a) and reader 2 (b). There were statistically significant differences between the approaches for the gluteus minimus tendon and the lateral portion of the gluteus medius tendon (p < 0.0005, both readers) with highest damage with the direct lateral approach. For the superoposterior portion of the gluteus medius tendon, no difference was found between the surgical approaches (p = 0.140 and p = 0.282 for reader 1 and 2, respectively). On x-axis 1 = posterior (plum), 2 = direct lateral (green), 3 = anterolateral (teal), 4 = anterior (orange). Gmin = Gluteus minimus tendon, GmedL = Gluteus medius tendon lateral portion, GmedP = Gluteus medius tendon posterior portion
-
Fluids - Fluid collections were uncommon for the direct lateral approach (Table 3). Fluid within the trochanteric bursa was most commonly found (12/30 patients) by both readers for the direct lateral approach (Table 4). Fluid within the iliopsoas bursa was found in 7/30 patients and not statistically significantly different compared to the other approaches (Table 4). Joint effusion was commonly detected, comparable to the other approaches (Table 5).
-
Other findings - Fascia lata defects of 10 mm or more were most commonly found for the direct lateral approach (six patients for reader 1, five patients for reader 2). No damage to nerves was detected.
-
-
Anterolateral approach (Fig. 5)
Fig. 5 59-year-old man 8 months after primary hip arthroplasty with hip pain. The anterolateral approach (white arrow (a), red arrow (b)) is clearly identifiable between the gluteus medius muscle and tensor fasciae latae muscle on the transverse T1-weighted image (a) and the schematic illustration (b). With the anterolateral approach there was no individual muscle or tendon that was most commonly damaged compared to the other approaches
-
Muscles - No muscle showed highest fatty degeneration with the anterolateral approach compared to the other approaches (Table 2). The anterior and mid portion of the gluteus minimus showed high Goutallier grades, but less than with the direct lateral approach and comparable to the posterior and the anterior approach (Table 2).
-
Tendons - Mean tendon quality was good with the anterolateral approach, comparable to the anterior approach (Figs. 2 and 4).
-
Fluids - Fluid collections were less common compared to the other approaches, only two for reader 1 and one for reader 2 (Table 3). Also, fluid within the trochanteric bursa was rare and less common compared to the other approaches (three patients for both readers) (Table 4). Fluid within the iliopsoas bursa was found in about one third of the patients by both readers with the anterolateral approach, comparable to the anterior approach and slightly more than with the posterior and direct lateral approach (Table 4). Joint effusion was commonly detected by both readers (Table 5).
-
Other findings - Defects of 10 mm or more to the fascia lata were uncommon (three for reader 1, two for reader 2). No nerve damage was detected.
-
-
Anterior Approach (Fig. 6)
Fig. 6 66-year-old woman 23 months after primary hip arthroplasty with hip pain and an external snapping hip. A transverse T1-weighted image (a) and the schematic illustration (b) show the anterior approach. Scarring and susceptibility artefacts along the anterior approach (white arrow (a), red arrow (b)) between the rectus femoris muscle and the tensor fasciae latae muscle are readily identifiable. Note that there is fatty atrophy of the gluteus minimus (rated Goutallier grade 3 on more cephalad sections, not shown) and medius muscles (Goutallier grade 2) in this patient (a). No individual muscle or tendon was most commonly damaged with the anterior approach compared to the other approaches
-
Muscles - No muscle was most heavily fatty degenerated with the anterior approach compared to the other approaches (Table 2, Fig. 6). Muscle quality was comparable to the anterolateral approach and good on average, except the anterior portion of the gluteus minimus, which showed high Goutallier grades on all approaches.
-
Tendons - Tendon quality was generally good with the anterior approach and no tendon showed highest damage scores compared to the other approaches (Figs. 2 and 4).
-
Fluids - Fluid within the access route was slightly more commonly found with the anterior approach compared to the anterolateral approach (Table 3). Fluid within the trochanteric bursa was uncommon (Table 4). Fluid within the iliopsoas bursa was as frequently found as with the anterolateral approach and more commonly compared to the posterior and direct lateral approach (Table 4). Joint effusion, as with the other approaches, was found in most cases (Table 5).
-
Other findings - A defect in the fascia lata of 10 mm or more was only found in one patient by both readers. No damage to nerves was detected.
-
Interreader agreement
Interreader agreement for fatty muscle infiltration (k = 0.548, range 0.127-0.818) and tendon damage score (k = 0.497, range 0.149-0.689) was moderate. Moderate interreader agreement was also found for extrabursal fluid collections (k = 0.452). Interreader agreement for fluid in the trochanteric bursa and iliopsoas bursa was substantial (k = 0.636). There was moderate agreement for detectable joint effusion (k = 0.584).
Discussion
In this study we showed that it is feasible to identify correctly the surgical approach after primary total hip arthroplasty by MR imaging. The surgical approach was correctly identified by susceptibility artefacts and scar tissue in all patients by both readers. We also established individual damage profiles for the posterior, direct lateral, anterolateral, and anterior surgical approach for total hip arthroplasty. Damage to the gluteus minimus muscle, external rotator muscles, as well as damage to the gluteus minimus and medius tendons and the external rotator tendons was most dependent on the surgical approach.
When reading an MR examination of a patient after THA, the surgical approach should be actively identified. Knowledge about the surgical approach helps radiologists to assess the most commonly damaged structures in clinical routine imaging. It provides guidance to the radiologists not to miss or misinterpret findings along the surgical approach. Because MRI allows confident identification of the surgical approach after primary total hip arthroplasty, it is not necessary to enquire about the surgical approach if the approach is not mentioned on the study request.
Previous studies have reported different soft tissue findings with MR imaging depending on the surgical approach, but only two different approaches were compared at a time [17, 18].
With the posterior approach, the short external rotators are usually detached to expose to the joint. This explains the high level of fatty infiltration in the short external rotators and the non-anatomic insertions of the tendons found in our study. Modifications of the posterior approach have been reported in which the external rotators are reattached [19] or at least partially spared [20]. This might explain why not all patients with non-anatomic insertions of the external rotators in our study showed high fatty infiltration of the corresponding muscles, as after a repair functionality might still be intact.
The direct lateral approach, also known as transgluteal approach, showed highest damage to the abductor muscles and tendons in our study. With this approach the gluteus medius muscle is transected, which can result in abductor muscle and tendon damage [21].
The anterolateral approach makes use of the intermuscular plane between the tensor fasciae latae muscle and the gluteus medius muscle, allowing sparing the hip abductors when using this approach [22]. Interestingly, in our study there was no single muscle or tendon commonly damaged with the anterolateral approach compared to the other approaches, proving the soft tissue sparing effect of this approach.
The anterior approach for total hip arthroplasty also uses an intermuscular plane and, therefore, no tendons or muscles have to be detached or released [21]. Bremer et al. compared the anterior approach with the direct lateral approach regarding soft tissue damage after total hip arthroplasty and less muscle and abductor tendon damage for the anterior approach has been reported [17], which was confirmed by our study.
Overall, our results showed that the anterolateral and anterior approach resulted in less muscle and tendon damage compared to the posterior and direct lateral approach. The reason for this is the access via intermuscular planes and preservation of the tendons by the anterior and anterolateral approach. However, even with the anterior approach, there might be accidental damage to the external rotators during surgery [23]. Therefore, a thorough evaluation of the MR examinations is mandatory.
Queen et al. reported no difference regarding gait mechanism 6 weeks after surgery between different surgical approaches [24]. Another study showed no difference in clinical hip scores, dislocation, and revision rates 5 years after total hip arthroplasty between the posterior and anterolateral approach [25]. On the other hand, Pfirrmann et al. have been shown that abductor tendon defects were more common in symptomatic patients than in asymptomatic patients after total hip arthroplasty using a direct lateral approach [13]. Because of the retrospective nature of our study we were not able to assess the clinical significance of the MRI findings that were detected.
A limitation of our study was the use of the Goutallier classification system on the hip muscles. In the shoulder muscle quality is generally assessed on the sagittal plane showing the cross section of the corresponding muscle. In the hip several muscles run obliquely in relation to standard imaging planes. Therefore, the used standard imaging planes (coronal, transverse, and sagittal) did often not show a nice cross section of a muscle, which may have made the assessment of the fatty atrophy more difficult. For the evaluation of the surgical approach we used scarring and susceptibility artefacts. However, a potential bias may have been coexisting soft tissue damage, such as muscle atrophy or muscle/tendon disruption along the approach, which obviously could not be completely ignored by the readers. Another limitation is the different interval between surgery and MR examination for the different surgical approaches, as this might also have an influence on the fatty atrophy. The intervals are different because the surgical technique evolved over time, nowadays often favouring the anterior or anterolateral approach.
In conclusion, we showed that MRI is well suited to identify surgical approaches after primary THA. The anterior and anterolateral approach showed less soft tissue damage compared to the posterior and direct lateral approach. Fluid collections did not show a specific pattern.
Abbreviations
- THA:
-
Total hip arthroplasty
References
Pabinger C, Geissler A (2014) Utilization rates of hip arthroplasty in OECD countries. Osteoarthr Cartil 22:734–741
Nho SJ, Kymes SM, Callaghan JJ, Felson DT (2013) The burden of hip osteoarthritis in the United States: epidemiologic and economic considerations. J Am Acad Orthop Surg 21:S1–S6
Berstock JR, Blom AW, Beswick AD (2014) A systematic review and meta-analysis of the standard versus mini-incision posterior approach to total hip arthroplasty. J Arthroplasty 29:1970–1982
O'Brien DA, Rorabeck CH (2005) The mini-incision direct lateral approach in primary total hip arthroplasty. Clin Orthop Relat Res 441:99–103
Jerosch J, Theising C, Fadel ME (2006) Antero-lateral minimal invasive (ALMI) approach for total hip arthroplasty technique and early results. Arch Orthop Trauma Surg 126:164–173
Hallert O, Li Y, Brismar H, Lindgren U (2012) The direct anterior approach: initial experience of a minimally invasive technique for total hip arthroplasty. J Orthop Surg Res 7:17
Potter HG, Nestor BJ, Sofka CM, Ho ST, Peters LE, Salvati EA (2004) Magnetic resonance imaging after total hip arthroplasty: evaluation of periprosthetic soft tissue. J Bone Joint Surg Am 86-a:1947–1954
Henderson RA, Lachiewicz PF (2012) Groin pain after replacement of the hip: aetiology, evaluation and treatment. J Bone Joint Surg (Br) 94:145–151
Siddiqui IA, Sabah SA, Satchithananda K et al (2014) A comparison of the diagnostic accuracy of MARS MRI and ultrasound of the painful metal-on-metal hip arthroplasty. Acta Orthop 85:375–382
Hayter CL, Koff MF, Shah P, Koch KM, Miller TT, Potter HG (2011) MRI after arthroplasty: comparison of MAVRIC and conventional fast spin-echo techniques. AJR Am J Roentgenol 197:W405–W411
Sutter R, Ulbrich EJ, Jellus V, Nittka M, Pfirrmann CW (2012) Reduction of metal artifacts in patients with total hip arthroplasty with slice-encoding metal artifact correction and view-angle tilting MR imaging. Radiology 265:204–214
Aliprandi A, Sconfienza LM, Randelli F, Bandirali M, Di Leo G, Sardanelli F (2012) Magnetic resonance imaging of painful total hip replacement: detection and characterisation of periprosthetic fluid collection and interobserver reproducibility. Radiol Med 117:85–95
Pfirrmann CW, Notzli HP, Dora C, Hodler J, Zanetti M (2005) Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology 235:969–976
Ulbrich EJ, Sutter R, Aguiar RF, Nittka M, Pfirrmann CW (2012) STIR sequence with increased receiver bandwidth of the inversion pulse for reduction of metallic artifacts. AJR Am J Roentgenol 199:W735–W742
Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res :78–83
Beasley TM, Schumacker RE (1995) Multiple regression approach to analyzing contingency tables: post hoc and planned comparison procedures. J Exp Educ 64:79–93
Bremer AK, Kalberer F, Pfirrmann CW, Dora C (2011) Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg (Br) 93:886–889
Muller M, Tohtz S, Springer I, Dewey M, Perka C (2011) Randomized controlled trial of abductor muscle damage in relation to the surgical approach for primary total hip replacement: minimally invasive anterolateral versus modified direct lateral approach. Arch Orthop Trauma Surg 131:179–189
Browne JA, Pagnano MW (2012) Surgical technique: a simple soft-tissue-only repair of the capsule and external rotators in posterior-approach THA. Clin Orthop Relat Res 470:511–515
Kim YS, Kwon SY, Sun DH, Han SK, Maloney WJ (2008) Modified posterior approach to total hip arthroplasty to enhance joint stability. Clin Orthop Relat Res 466:294–299
Matta JM, Shahrdar C, Ferguson T (2005) Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res 441:115–124
Bertin KC, Rottinger H (2004) Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res :248-255
Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ (2006) Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res 453:293–298
Queen RM, Butler RJ, Watters TS, Kelley SS, Attarian DE, Bolognesi MP (2011) The effect of total hip arthroplasty surgical approach on postoperative gait mechanics. J Arthroplasty 26:66–71
Palan J, Beard DJ, Murray DW, Andrew JG, Nolan J (2009) Which approach for total hip arthroplasty: anterolateral or posterior? Clin Orthop Relat Res 467:473–477
Acknowledgments
An oral abstract of this manuscript was presented at the European Congress of Radiology 2015. The scientific guarantor of this publication is Christoph Agten. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agten, C.A., Sutter, R., Dora, C. et al. MR imaging of soft tissue alterations after total hip arthroplasty: comparison of classic surgical approaches. Eur Radiol 27, 1312–1321 (2017). https://doi.org/10.1007/s00330-016-4455-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4455-7