Abstract
Objectives
To assess the efficacy and safety profile of stent-retriever thrombectomy (SRT) in acute anterior ischemic stroke patients with tandem occlusion.
Materials and methods
Using the MEDLINE database, we conducted a systematic review and meta-analysis of all studies that included patients with acute ischemic stroke attributable to tandem occlusion who received treatment with SRT between November 2010 and May 2015.
Results
The literature search identified 11 previous studies involving a total of 237 subjects out of whom 193 (81.4 %) were treated with acute stent placement for the extracranial internal carotid artery occlusion. Mean initial NIHSS score was 17, and median time from onset to recanalization was 283.5 min. Mean intravenous thrombolysis rate was 63.8 %. In the meta-analysis, the recanalization rate reached 81 % (95 % CI, 73–89). Meta-analysis of clinical outcomes showed a pooled estimate of 44 % (95 % CI, 33–55; 10 studies) for favourable outcome, 13 % (95 % CI, 8–20; 10 studies) for mortality, and 7 % (95 % CI, 2–13; eight studies) for symptomatic intracranial haemorrhage.
Conclusion
SRT with emergency carotid stenting is associated with acceptable safety and efficacy in acute anterior stroke patients with tandem occlusion compared to natural history. However, the best modality to treat proximal stenosis is based on an individual case basis.
Key Points
• Stent retriever thrombectomy of tandem occlusion is efficient and safe.
• Emergent carotid stenting during thrombectomy increase symptomatic intracranial haemorrhage without impact mortality.
• Thrombectomy of tandem anterior circulation occlusion may be the first therapeutic option
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute ischemic strokes due to tandem occlusions of the extracranial internal carotid artery (ICA) and the distal ICA and/or proximal middle cerebral artery (MCA) are associated with poor prognosis [1]. Recanalization rate of large vessel occlusion had been proven to improve significantly using stent retrievers as opposed to intravenous (IV) thrombolysis in several trials [2–6], which was the most powerful predictor of favourable outcome in stroke patients [7]. Since the publications of MR CLEAN, ESCAPE, EXTEND-IA, SWIFT PRIME, and REVASCAT, stent-retriever thrombectomy (SRT) is now the new standard of care in association with IV thrombolysis for stroke with distal ICA and/or proximal MCA occlusion [8]. However, endovascular treatment of tandem occlusion could be more difficult and take more time and could require emergency ICA stenting, which increases the risk of symptomatic intracranial haemorrhage (sICH) due to antiplatelet therapy. Pending the results of randomized trial including specifically the tandem occlusions and/or meta-analysis of tandem stroke patients included in MR CLEAN, ESCAPE, and REVASCAT trials, the benefit and safety of SRT still needs to be determined in stroke patients with acute tandem occlusions.
The aim of this study was to assess efficacy and safety outcomes for SRT in anterior circulation stroke patients with acute tandem occlusion. We, therefore, conducted a systematic review of all previous studies using this endovascular approach.
Materials and methods
Using the MEDLINE database and keywords terms of “tandem occlusion”, “carotid occlusion”, “acute stroke”, “acute carotid stenting”, “endovascular treatment”, we searched for studies published between 1 November 2010 and 1 May 2015 that included patients with acute ischemic stroke attributable to tandem occlusion who had received treatment with SRT regardless of the study design. We included only articles that used stent-retrievers for thrombectomy or those where we could extract the data on patients treated with stent-retrievers. Thus, articles with mixture of thrombectomy devices without specific outcome on patients treated with stent-retrievers were excluded. Only studies with > 5 cases of stroke associated with tandem occlusion were included in our analysis to minimize the chance of anecdotal outcomes. Two authors (RSH) identified potentially relevant articles at title or abstract level and obtained the full text for detailed review.
Data analysis
Each study had to report recanalization rates, functional neurological outcomes symptomatic intracerebral haemorrhage (sICH) rates, and mortality rates. Successful recanalization was defined as "thrombolysis in cerebral infarction" (TICI) ≥2b revascularization of the MCA. Favourable outcome was defined as modified Rankin Scale (mRS) ≤2 at 90 days. Mortality was evaluated at discharge or 90 days as determined by each author. According to European Cooperative Acute Stroke Study II (ECASS-II) [9], sICH was defined as any parenchymal hematoma, subarachnoid haemorrhage, or intraventricular haemorrhage associated with worsening of the National Institutes of Health Stroke Scale (NIHSS) score by ≥4 within 24 h.
Meta-analysis
The 95 % CIs of the estimates were built with the Wilson method. The estimate and the 95 % CI of the mean percentage over all the studies were obtained for each outcome using a logistic mixed model with a random effect on the intercept in order to take into account the heterogeneity between the studies. The meta-analyses were carried out using the metaprop Stata command on Stata/SE 14.1 (Statacorp LP, College Station TX, USA) [10]. We prepared this report with reference to MOOSE (meta-analyses of observational studies) guidelines.
Individual study quality assessment
The included studies being uncontrolled, individual study quality was assessed using a checklist published by the National Institutes of Health for before-after (pre-post) studies with no control group [11]. This 12-item checklist enables an assessment of uncontrolled studies and provides an overall quality rating. Quality assessment was performed independently by two authors (BG).
Results
A total of 180 citations were identified. After reviewing the records at title or abstract level, 35 articles were read in full and 11 were judged eligible for inclusion (Fig. 1) [12–22]. The subgroup of tandem stroke patients in MR CLEAN, ESCAPE, and REVASCAT trials were not included because of the unavailability of recanalization, favourable outcome, sICH, and mortality rates [2, 3, 5]. The included studies enrolled 237 patients (mean sample size, 21; range, 7–43). All of the studies were case series; most of them (n = 9) were classified as retrospective case series analysis. Studies used for analysis for each group, including methodological and baseline characteristics of the included studies, as well as treatment outcomes, are listed in Table 1.
All patients received thrombectomy with stent-retrievers, the Solitaire stent (Covidien) was used in all studies, and in four series a combination of devices (Solitaire; Revive, Codman Neurovascular; Trevo, Stryker; Preset, Phenox). A majority of patients (n = 193) were treated with acute stent for the ICA occlusion during the same procedure. In five articles the stenting was done after thrombectomy, and in five it was done in an antegrade manner prior to thrombectomy. Three authors used both techniques. [13, 16, 20] The admission mean NIHSS score was 17 (range, 14–20), and median time from onset to recanalization was 283.5 min (range, 200–302; eight studies). Mean intravenous (IV) thrombolysis rate was 63.8 % (range, 28.6-91.7; nine studies).
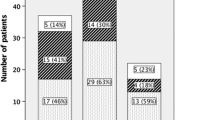
In the meta-analysis (237 patients), the overall recanalization rate was 81 % (95 % CI, 73–89), and clinical outcomes were favourable at 3 months in 44 % (95 % CI, 33–55; 10 studies). The recorded mortality was 13 % (95 % CI, 8–20; 10 studies) at 3 months follow-up, and the symptomatic intracranial haemorrhage was 7 % (95 % CI, 2–13; 8 studies) (Fig. 2). We found no evidence of major publication and selection bias by examining the funnel plots.
In the meta-analysis of tandem patients treated with acute ICA stenting (193 patients), the overall recanalization rate was 83 % (95 % CI, 73–91), and clinical outcomes were favourable at 3 months in 46 % (95 % CI, 35–58; nine studies). The recorded mortality was 13 % (95 % CI, 8–19; eight studies) at 3 months follow-up, and the symptomatic intracranial haemorrhage was 4 % (95 % CI, 0–10; six studies) (Fig. 3). We found no evidence of major publication and selection bias by examining the funnel plots. Antiplatelet therapy was noted in nine studies, and aspirin (250 to 500 mg) and clopidogrel (300 to 600 mg) was associated in six of them [12, 15–17, 20, 22]. In the study of Soize el al [17], a single IV bolus of 250 mg aspirin was administered after ICA stent deployment. In one study, tirofiban and eptifibatide was added to the association of aspirin and clopidogrel [14, 20], respectively. Acute carotid stent thrombosis was reported in only one study (one out of 24 patients) [22].
Quality assessment
Nine studies were retrospective whereas two were prospective. All were non-comparative. Studies had large heterogeneity in terms of methods for the assessment of outcomes (presence or not of an adjudication committee; presence or not of a centralized core laboratory; different antiplatelet regimen). Using the prespecified tool, the quality rating of studies was considered good in two studies, the other being rated as fair or poor. The main limitations of studies were as follows: no prespecification of selection criteria for the study population; no justification of sample size; no independent assessment of outcome measures across all study participants. Consequently, the risk of bias was significant in all but two studies.
Discussion
Efficacy of SRT in tandem occlusions
Pooled data from all of the studies included in our analysis suggest high successful recanalization rates and acceptable favourable outcome rates for acute tandem occlusion stroke patients treated with SRT. The overall recanalization rate was 81 % (95 % CI, 73–89), and the pooled estimate of favourable clinical outcome was 44 % (95 % CI, 33–55). Similar results were recently reported in a large series of 170 tandem anterior stroke patients included in four German databases between 2007 (before the introduction of stent-retrievers for mechanical thrombectomy) and 2014 with a recanalization rate of 77 %, and a favourable outcome in 36 % of cases [23]. High rate of recanalization (87 %) and favourable outcome (68 %) were reported in December 2015 in series of 47 consecutive stroke patients with carotid occlusion or high-grade stenosis and concomitant intracranial embolus treated with carotid stenting and intracranial SRT between September 2011 and December 2014 (median NIHSS 16, 85 % IV thrombolysis, mean time from stroke onset to recanalization 311 min) [24]. This series was not included in our meta-analysis because it was very recently published. The functional benefit at 3 months of SRT in association with IV thrombolysis over IV thrombolysis alone was recently proven in the setting of intracranial occlusions; however, the presence of extracranial ICA tandem occlusion seems not change those results, as the ESCAPE, MR CLEAN, and the EXTEND IA reported better outcome within this subgroup. In fact, the superiority of SRT persists significantly in the subgroup of patients with tandem occlusion in MR CLEAN (75 out of 233 patients; OR = 1.43, 95 % CI = 0.78-2.64), ESCAPE (21 out of 165 patients; OR = 9.64, 95 % CI = 2.62-35.49), and REVASCAT (19 out of 102 patients; OR = 4.3, 95 % CI = 1.5-12.5) [2, 3, 5]. In our study, bridging therapy was used in the majority of cases (63.8 %), a similar rate of thrombolysis in REVASCAT trial (68 %). A previous meta-analysis in 2012 including a majority of series without stent retrievers has suggested that an endovascular approach to stroke caused by acute ICA occlusion results in higher rates of favourable outcomes than treatment with IV thrombolysis alone [25], since the rate of recanalization of IV thrombolysis alone is very low for ICA (less than 10 %) [26]. In addition, in a subgroup analysis, distal ICA and tandem ICA and M1 occlusions showed greater recanalization and a trend toward better outcome with endovascular treatment in IMS III trial [27].
In our meta-analysis, recanalization and favourable outcome rates in tandem occlusion treated by SRT are in line with the results of MR CLEAN, ESCAPE, and REVASCAT trials [2, 3, 5]. This favourable outcome rate could be explained by a systematic use of stent-retrievers and an early recanalization. Although no tandem occlusion was treated in SWIFT and TREVO 2 trials, stent-retrievers achieved faster and more complete recanalization, and improve significantly the rate of favourable clinical outcomes in large vessel occlusion strokes compared to the previous generation of mechanical devices such as the MERCI retriever [28, 29]. In addition, early recanalization is the most powerful predictor of stroke outcome after either IV thrombolysis or either endovascular therapy with or without stent-retrievers [30–32]. Endovascular treatment of tandem occlusion can possibly take more time compared to that of intracranial occlusion alone. However, no published data compared the time to recanalization after thrombectomy between tandem occlusion and intracranial occlusion alone. In our study, the median time from onset to recanalization was relatively short (283.5 min), this may explain at least partially our favourable outcome rate.
Safety of SRT in tandem occlusions
Early administration of aspirin in acute stroke patients treated with thrombolysis is usually not recommended during the first 24 h because of the higher risk of sICH. In fact, in the randomized trial ARTIS trial, sICH occurred more frequently in the aspirin group compared to the standard treatment group (4.3 % versus 1.6 %, 95 % CI, 0.2-5.4; p = 0.04), and sICH was more often the cause of poor outcome in the aspirin group compared to the standard treatment group (11 vs. 1, p = 0 · 006) [33]. In our study, acute ICA stenting was performed in the majority of thrombectomy procedures in studies included in our analysis (81.4 %, 193 ICA stenting out of 237 tandem occlusions). According to our meta-analysis, emergency stent placement in the extracranial ICA in combination with anterior circulation thrombectomy is associated with a reasonable risk of sICH (7 %), which is probably related to early administration of antiplatelet therapy. In the study of Lescher et al, 39 consecutive patients were included and nine of them received cervical ICA stent placement. Surprisingly, no sICH occurred in ICA stent group whereas four patients (13 %) presented sICH. There was no significant difference in the occurrence of sICH in patients with antiplatelet therapy after stent placement although the majority of patients received IV thrombolysis (73 % versus 78 %) [19]. In a recent review of intra-arterial treatment of patients with acute ischemic stroke due to ICA occlusion, Kappelhof et al reported an overall sICH rate of 9 % for all cases ICA occlusion, and 16 % for tandem cases with no statistical differences [34]. In addition, in the population with extracranial ICA occlusion, stenting resulted in a higher recanalization rate (87 % vs. 48 %, p = 0.001), favourable outcome rate (68 % vs. 15 %, p < 0.001) and lower mortality (18 % vs. 41 %, p = 0.048) than intra-arterial thrombolysis. Two approaches of ICA stenting are available. In this review including 11 studies, six and five series reported retrograde and antegrade stenting technique, respectively. Lockau et al reported that the mean angiography time was significantly shorter in the "thrombectomy first" group (43.1 ± 30.8 vs. 110.8 ± 43.0 min, p < 0.001), and more patients had favourable outcomes after 3 months (52.0 vs. 33.3 %, p = 0.319) [20], whereas Stampfl et al found a median increase of the reperfusion time of 20 min when stenting was necessary [16]. To date, there is not enough good quality evidence in the literature to support acute stenting of carotid stenosis in the acute setting of tandem lesions in ischemic stroke. Operator judgment is advised on an individual case basis. A conservative approach would be balloon dilation of the stenosis to complete MCA thrombectomy and once patient stability and lack of hemorrhagic transformation of stroke is ascertained [9, 35, 36], carotid stenting must be employed or a carotid endarterectomy can be performed based on consensus opinion. Acute stent placement in carotid stenosis in the situation of tandem lesions in ischemic stroke may be potentially hazardous and hence sound operator judgment is recommended before embarking on such a procedure.
Thrombectomy using stent-retrievers in tandem occlusion patients did not impact negatively on mortality since our meta-analysis showed a pooled estimate of 13 % (95 % CI, 8–20; 10 studies). Before the demonstration of clinical benefit of SRT, the safety of endovascular approach were demonstrated in three randomized clinical trials in 2013 [37–39]. In fact, these trials showed The trial showed similar safety outcomes with endovascular therapy after IV thrombolysis, as compared with IV thrombolysis alone. However, stent-retrievers were used in only a small number of patients. In addition, our findings are consistent with data from the five positive trials (range, 9–21 %) [2–6]. In ESCAPE trial, the mortality was significantly reduced when the patients was reperfused by stent-retrievers compared to thrombolysis alone since the adjusted odds ratio was 0.5 (95 % CI, 0.3-0.8) [3]. The earlier time to reperfusion in this study may account for a relatively low mortality rate, especially in a severe group of acute ischemic stroke [1]. The effect of shorter interval from symptom onset to reperfusion was previously reported in a large collaborative pooled analysis of seven endovascular databases including 480 patients [40]. The adjusted odds ratio for each 30-minute time increase was 1.21 (95 % CI, 1.09-1.34; p < 0.001) for mortality, and the positive effect of onset-to-reperfusion time on mortality was stronger in patients with ICA occlusion than in patients with isolated MCA within 6 h [40].
Limitations
There are limitations of our study. The articles included in our systematic review were heterogeneous in terms of study design. Centres differ in their treatment protocols and interpretation and reporting of results, which should be considered when interpreting the results of our systematic analysis. We did not have access to the individual data of the studies and could not separate patients who were treated with acute carotid stenting from those who did not. This is a limit to appreciate the impact of SRT alone and with carotid stenting on clinical outcomes, especially for sICH rate. A range of antiplatelet protocols was used: Soize et al [17] administered a 250 mg IV bolus of aspirin after stent placement, whereas Lockau et al [20] gave a weight-adapted bolus of tirofiban followed by a continuous infusion for 24 h. The risk of acute instent-thrombosis seems very low since this phenomenon was reported in only one study in our analysis [22]. Recently, Sorkin et al reported a case of hyperacute (25 min later) carotid stent thrombosis successfully treated by intra-arterial bolus dose of eptifibatide. The patient was discharge 3 days post-revascularisation on dual antiplatelet therapy with an NIHSS score of 1 [41]. In the Danish series, eight (17 %) patients had acute stent thrombosis during procedure [24]. In seven of those patients, stent recanalization was achieved with local administration of GPIIb/IIIa inhibitor; in one patient recanalization was not attempted because of excellent collateral flow and complete intracranial recanalization. Thirty-nine (91 %) patients had patent carotid stents at 3-month follow-up while four (9 %) patients had occluded stents [24].
Conclusions
Our study supports that thrombectomy using stent-retrievers with emergency stenting of cervical ICA is associated with acceptable safety and efficacy in acute anterior stroke patients with tandem occlusion. The jury is still out about the best way to treat proximal stenosis in tandem lesions with anterior circulation acute ischemic stroke. Whether to treat by acute stenting or salvage balloon angioplasty to complete mechanical thrombectomy followed by delayed stenting or endarterectomy are decisions which should be made by the operator on an individual case basis bearing in mind the various pros and cons of each method of treatment.
References
Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J et al (2006) Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke 37:2301–2305
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ et al (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11–20
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 372:2285–2295
Kharitonova TV, Melo TP, Andersen G, Egido JA, Castillo J, Wahlgren N, SITS investigators (2013) Importance of cerebral artery recanalization in patients with stroke with and without neurological improvement after intravenous thrombolysis. Stroke 44:2513–2518
Grotta JC, Hacke W (2015) Stroke neurologist's perspective on the new endovascular trials. Stroke 46:1447–1452
Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D et al (1998) Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Lancet 352:1245–1251
Nyaga VN, Arbyn M, Aerts M (2014) Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72:39
U.S. department of Health and Human services-National Institutes of Health (NIH) (2014) Quality Assessment Tool for Before-After (Pre-Post) Studies With No Control Group
Papanagiotou P, Roth C, Walter S, Behnke S, Grunwald IQ, Viera J et al (2011) Carotid artery stenting in acute stroke. J Am Coll Cardiol 58:2363–2369
Machi P, Lobotesis K, Maldonado IL, Costalat V, Vendrell JF, Riquelme C et al (2012) Endovascular treatment of tandem occlusions of the anterior cerebral circulation with solitaire FR thrombectomy system. Initial experience. Eur J Radiol 81:3479–3484
Mpotsaris A, Bussmeyer M, Buchner H, Weber W (2013) Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: antegrade approach with wallstent and solitaire stent retriever. Clin Neuroradiol 23:207–215
Maurer CJ, Joachimski F, Berlis A (2014) Two in one: endovascular treatment of acute tandem occlusions in the anterior circulation. Clin Neuroradiol. Jul 3. [Epub ahead of print].
Stampfl S, Ringleb PA, Möhlenbruch M, Hametner C, Herweh C, Pham M et al (2014) Emergency cervical internal carotid artery stenting in combination with intracranial thrombectomy in acute stroke. AJNR Am J Neuroradiol 35:741–746
Soize S, Kadziolka K, Estrade L, Serre I, Barbe C, Pierot L (2014) Outcome after mechanical thrombectomy using a stent retriever under conscious sedation: comparison between tandem and single occlusion of the anterior circulation. J Neuroradiol 41:136–142
Cohen JE, Gomori JM, Rajz G, Itshayek E, Eichel R, Leker RR (2015) Extracranial carotid artery stenting followed by intracranial stent-based thrombectomy for acute tandem occlusive disease. J Neurointerv Surg 7:412–417
Lescher S, Czeppan K, Porto L, Singer OC, Berkefeld J (2015) Acute stroke and obstruction of the extracranial carotid artery combined with intracranial tandem occlusion: results of interventional revascularization. Cardiovasc Intervent Radiol 38:304–313
Lockau H, Liebig T, Henning T, Neuschmelting V, Stetefeld H, Kabbasch C et al (2015) Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results. Neuroradiology 57:589–598
Mishra A, Stockley H, Goddard T, Sonwalker H, Wuppalapati S, Patankar T (2015) Emergent extracranial internal carotid artery stenting and mechanical thrombectomy in acute ischaemic stroke. Interv Neuroradiol 21:205–214
Yoon W, Kim BM, Kim DJ, Kim DI, Kim SK (2015) Outcomes and prognostic factors after emergent carotid artery stenting for hyperacute stroke within 6 hours of symptom onset. Neurosurgery 76:321–329
Behme D, Mpotsaris A, Zeyen P, Psychogios MN, Kowoll A, Maurer CJ et al (2015 Aug) Emergency stenting of the extracranial internal carotid artery in combination with anterior circulation thrombectomy in acute ischemic stroke: a retrospective multicenter study. AJNR Am J Neuroradiol 20 [Epub ahead of print]
Steglich-Arnholm H, Holtmannspötter M, Kondziella D, Wagner A, Stavngaard T, Cronqvist ME et al (2015) Thrombectomy assisted by carotid stenting in acute ischemic stroke management: benefits and harms. J Neurol 262:2668–2675
Mokin M, Kass-Hout T, Kass-Hout O, Dumont TM, Kan P, Snyder KV et al (2012) Intravenous thrombolysis and endovascular therapy for acute ischemic stroke with internal carotid artery occlusion: a systematic review of clinical outcomes. Stroke 43:2362–2368
del Zoppo GJ, Poeck K, Pessin MS, Wolpert SM, Furlan AJ, Ferbert A et al (1992) Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke. Ann Neurol 32:78–86
Demchuk AM, Goyal M, Yeatts SD, Carrozzella J, Foster LD, Qazi E et al (2014) Recanalization and clinical outcome of occlusion sites at baseline CT angiography in the interventional management of stroke III trial. Radiology 273:202–210
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG et al (2012) Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet 380:1241–1249
Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA et al (2012) Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet 380:1231–1240
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E et al (2014) Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials. Lancet 384:1929–1935
Khatri P, Yeatts SD, Mazighi M, Broderick JP, Liebeskind DS, Demchuk AM et al (2014) Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol 13:567–574
Sheth SA, Jahan R, Gralla J, Pereira VM, Nogueira RG, Levy EI, et al (2015) Time to endovascular reperfusion and degree of disability in acute stroke. Ann Neurol Jul 7.. [Epub ahead of print]
Zinkstok SM, Roos YB (2012) ARTIS investigators. Early administration of aspirin in patients treated with alteplase for acute ischaemic stroke: a randomised controlled trial. Lancet 380:731–737
Kappelhof M, Marquering HA, Berkhemer OA, Majoie CB (2015) Intra-arterial treatment of patients with acute ischemic stroke and internal carotid artery occlusion: a literature review. J Neurointerv Surg 7:8–15
Mlynash M, Lansberg MG, De Silva DA, De Silva DA, Lee J, Christensen S, Straka M et al (2011) Refining the definition of the malignant profile: insights from the DEFUSE-EPITHET pooled data set. Stroke 42:1270–1275
Gory B, Sivan-Hoffmann R, Riva R, Labeyrie PE, Huguet N, Nighoghossian N et al (2015) Repeated Solitaire mechanical thrombectomy in an acute anterior stroke patient. Revue Neurologique 171:682–684
Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD et al (2013) Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 368:893–903
Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z et al (2013) A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 368:914–923
Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R et al (2013) Endovascular treatment for acute ischemic stroke. N Engl J Med 368:904–913
Mazighi M, Chaudhry SA, Ribo M, Khatri P, Skoloudik D, Mokin M et al (2013) Impact of onset-to-reperfusion time on stroke mortality: a collaborative pooled analysis. Circulation 127:1980–1985
Sorkin GC, Dumont TM, Mokin M, Eller JL, Natarajan SK, Levy EI et al (2015) Hyperacute carotid stent thrombosis during emergent revascularization treated with intraarterial eptifibatide after systemic administration of recombinant tissue plasminogen activator. J Vasc Interv Neurol 8:50–55
Acknowledgments
The scientific guarantor of this publication is Benjamin Gory, MD, MSc. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. Xavier Armoiry kindly provided statistical advice for this manuscript. Institutional Review Board approval was not required because it’s a systematic review. Written informed consent was not required for this study because it’s a systematic review of published articles. Approval from the institutional animal care committee was not required because it’s clinical research. Some study subjects or cohorts have been previously reported in Pubmed database. Methodology: retrospective, observational, multicenter study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Rotem Sivan-Hoffmann and Benjamin Gory contributed equally to this work.
Rights and permissions
About this article
Cite this article
Sivan-Hoffmann, R., Gory, B., Armoiry, X. et al. Stent-Retriever Thrombectomy for Acute Anterior Ischemic Stroke with Tandem Occlusion: A Systematic Review and Meta-Analysis. Eur Radiol 27, 247–254 (2017). https://doi.org/10.1007/s00330-016-4338-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4338-y