Abstract
Background
Acute large cerebral artery occlusions respond poorly to systemic thrombolysis with recombinant tissue plasminogen activator (rTPA) alone. The value of stent retriever–based mechanical thrombectomy in patients with additional extracranial occlusion of the internal carotid artery (ICA), who require acute a priori extracranial stenting in order to reach the intracranial obstruction site, is not well known. We determined the outcome after emergency revascularization in acute stroke with tandem occlusions of the anterior circulation.
Methods
According to specific inclusion/exclusion criteria, eligible stroke patients with large artery occlusions underwent mechanical recanalization with the Solitaire stent retriever. In case of a tandem occlusion, we performed an acute stenting with the Wallstent before thrombectomy. From October 2009 to March 2011, 50 patients were treated according to this protocol; time frames, clinical data, recanalization rates, and midterm outcome were recorded.
Results
Forty-one patients had a large artery occlusion in the anterior circulation and nine in the posterior circulation. Mechanical recanalization was successful in 35/41 cases (85 %). Six of 41 patients (15 %) died in the acute phase. In 17/41 patients (42 %), thrombectomy was preceded by an emergency stenting in the extracranial portion of the internal carotid artery (ICA). National Institutes of Health Stroke Scale (NIHSS)/modified Rankin Scale (mRS) scores showed significant improvement in both the stenting group and the nonstenting group; there were no significant differences between the groups. At 90 days, 54 % of patients with emergency stenting had a good outcome.
Conclusions
Acute extracranial stenting with the Wallstent combined with intracranial Solitaire-based thrombectomy is safe and may lead to an improvement in neurological outcome in patients with an otherwise poor prognosis under i.v. thrombolysis alone.
Zusammenfassung
Hintergrund
Akute Gefäßverschlüsse der großen hirnversorgenden Arterien haben niedrige Rekanalisierungsraten unter alleiniger systemischer Thrombolyse mit rTPA. Die Effizienz einer stent-retriever basierten, mechanischen Thrombektomie in Patienten mit einem zusätzlichen extrakraniellen Verschluss der A. carotis interna, die zunächst extrakraniell gestentet werden müssen, um einen intrakraniellen Zugang zu ermöglichen, ist wenig untersucht. In der vorliegenden Arbeit wurde das klinische Outcome nach endovaskulärer Rekanalisation im akuten Schlaganfall bei Tandem-Okklusionen der vorderen Zirkulation untersucht.
Methoden
Basierend auf spezifischen Ein- und Ausschluss-Kriterien wurden geeignete Patienten mit Verschlüssen großer hirnversorgender Arterien mittels mechanischer Thrombektomie mit dem Solitaire stent-retriever behandelt. Im Falle einer Tandem-Okklusion wurde eine akute Stentimplantation (Wallstent) vorgeschaltet. Zwischen Oktober 2009 und März 2011 wurden 50 Patienten endovaskulär behandelt. Erfasst wurde neben den klinischen und angiographischen Parametern auch das klinische Outcome nach 90 Tagen.
Ergebnisse
41 Patienten hatten einen Verschluss eines großen hirnversorgenden Gefässes in der vorderen, 9 in der hinteren Zirkulation. Die Rekanalisationsrate betrug in der vorderen Zirkulation 85 % (35/41). 6/41 Patienten (15 %) verstarben in der akuten Phase. In 17/41 Patienten (42 %) war eine vorgeschaltete, akute, Stent-basierte Rekanalisation der extrakraniellen A. carotis interna erforderlich. Die respektiven NIHSS (National Institutes of Stroke Health Scale) und mRS (modifizierte Rankin Skala) Scores verbesserten sich sowohl in der Gruppe der akut gestenteten Patienten, als auch in der Gruppe der nicht gestenteten Patienten; es wurden keine signifikanten Unterschiede zwischen beiden Gruppen beobachtet. Nach 90 Tagen wiesen 54 % der akut gestenteten Patienten ein gutes klinisches Ergebniss auf.
Schlussfolgerungen
Die Kombination eines akuten extrakraniellen Stentings der A. carotis interna verbunden mit einer anschließenden intrakraniellen mechanischen Rekanalisation mittels Solitaire ist technisch sicher und kann zu einer Verbesserung des neurologischen Ergebnisses bei Patienten führen, die unter alleiniger systemischer Thrombolyse eine eingeschränkte Prognose aufweisen
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascular recanalization has a decisive influence on functional clinical outcome after stroke [1]. However, in acute stroke, proximal cerebral artery occlusion is associated with poor recanalization rates under i.v. thrombolytic therapy. Only 5.9 % of distal internal carotid artery (ICA) occlusions are successfully recanalized with recombinant tissue plasminogen activator (rTPA) alone [2].
In recent times, there is growing evidence for a potential benefit of mechanical thrombectomy in acute stroke caused by proximal large vessel occlusions. The second generation thrombectomy devices, termed “stent retrievers,” play a key role in this interventional therapy. Most of the published data refers to the Solitaire AB or Solitaire FR stent retriever (ev3 Inc., Plymouth, MN), whose superiority to the first generation device MERCI (Concentric Medical, Mountain View, CA) has recently been shown [3]. However, there is little information available on the effect of stent retriever–based mechanical thrombectomy in patients with additional extracranial occlusion of the ICA, who require acute a priori extracranial stenting in order to reach the intracranial obstruction site.
The present study aims at evaluating the clinical outcome of stroke patients after acute mechanical recanalization of carotid-T or M1 occlusions with preceding acute extracranial ICA stenting. This study is a subgroup analysis of prospectively collected intention-to-treat data of all patients eligible for mechanical thrombectomy between October 2009 and March 2011 at our institution.
Materials and Methods
Prerequisites
The study was approved by the institutional review committee. All subjects gave informed consent.
Patient Selection Criteria
Between October 2009 and November 2011, all consecutive acute stroke patients aged 80 years or younger with an National Institutes of Health Stroke Scale (NIHSS) score of ³ 10 presenting within a 4.5-h time frame from symptom onset were triaged on admission for potential mechanical thrombectomy with the Solitaire stent retriever (initially AB, then FR). Also, patients presenting with an NIHSS score of < 10 were considered in case of clinically fluctuating symptoms or secondary worsening of 4 or more NIHSS points after admission, as well as patients with a last well-time beyond 4.5 h and obvious mismatch between severe neurological deficits and cranial computed tomography (CT) findings.
All patients had to fulfill the following preinterventional CT-based imaging criteria to be mechanically thrombectomized: (1) absence of cerebral hemorrhage, (2) no acute infarction in more than one-third of middle cerebral artery (MCA) territory in native cranial CT scan, and (3) CT angiography (CTA) showing arterial occlusion in the ICA and/or the MCA (M1 and M2 segments, respectively) of the anterior circulation or in the posterior circulation (vertebral artery [VA], basilar artery [BA], and posterior cerebral artery [PCA]) corresponding to the clinical syndrome.
While digital image processing of the CTA was underway, the patients eligible for i.v. rTPA were treated according to the guidelines of the German Neurological Society independently from the decision for mechanical thrombectomy. For the present study, we retrospectively analyzed the subgroup of patients with carotid-T or M1 occlusions who required acute a priori stenting of the ICA (tandem occlusions).
Endovascular Treatment
General Approach
The treatment of the anterior circulation vessel obstructions was performed under general anesthesia. Through a transfemoral approach, a 6-Fr guiding catheter Neuropath (Micrus, San Jose, CA) or Neuron (Penumbra, Alameda, CA) was placed in the proximal ICA. A heparinized saline solution was continuously applied through the catheter for the duration of the intervention. A 0.014-inch guide wire was advanced over a Rapidtransit microcatheter (Cordis, Bridgewater, NJ) and navigated distal to the clot. The microcatheter was then subsequently advanced over the wire through the clot. The correct position of the microcatheter tip distally of the clot and the selected vessel’s diameter were depicted by a gentle contrast injection before advancing the Solitaire stent (4/20) through the microcatheter. The stent was deployed with its distal portion being placed a few millimeters distal to the clot. At this point, a routine control injection was performed via the guide catheter to check for a potential restoration of flow distal to the thrombus. The Solitaire was kept deployed for 1–2 min. Then, one-third of the stent was retrieved and the microcatheter and the stent were gently withdrawn through the guide catheter under continuous proximal aspiration with a syringe. A control angiography was performed to assess the degree of recanalization and reperfusion. If there was no or incomplete recanalization, the procedure was repeated up to a maximum of four maneuvers. Any relevant vascular stenosis proximal to the occlusion was treated by stent implantation before using the thrombectomy device.
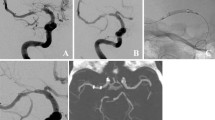
Tandem Occlusions
In case of a tandem occlusion, we used the so-called antegrade approach or technique in all cases (stenting followed by thrombectomy). An 8-Fr Vista Brite Tip guiding catheter (Cordis, Bridgewater, NJ) was placed into the ipsilateral distal common carotid artery. A 0.014-inch wire was then passed through the proximal ICA occlusion, and a microcatheter was advanced over this wire into the petrous portion. Then, a contrast injection was performed in order to verify passage into the true lumen and to depict the extent of the occlusive lesion. Extracranial carotid stenting was carried out without the use of any protective devices, as there was an intracranial obstruction in all cases. Prestenting balloon angioplasty was performed when necessary with a 3.0- or 3.5-mm balloon. All patients received a Wallstent (Boston Scientific, Natick, MA). For poststenting angioplasty, 4.5- or 5.0-mm balloons were used. The subsequent thrombectomy in the carotid-T or M1 segment was carried out as described until the point of retrieval of the Solitaire. This step has to be carried out carefully, as there is a potential for an entrapment of the Solitaire in the Wallstent. It is crucial to pass the Wallstent with the guiding catheter first, verifying its correct position once again before removing the partially sheathed Solitaire.
Periprocedural Antiplatelet Regimen in Tandem Occlusions
If the patients had no prior medication with dual antiplatelet therapy for other medical indications at the time of treatment, eptifibatide was continuously infused for 24 h to prevent secondary stent occlusion. We decided to use eptifibatide instead of acetylsalicylic acid (ASA) as early antiplatelet therapy because of it has a short half-life allowing for decompressive craniectomy in case of edematous brain swelling. The combination of rTPA and eptifibatide has been considered safe [4].
Patients were monitored in the intensive care unit postinterventionally. A control CT scan was obtained after 24 h or earlier in case of any neurological worsening (NIHSS score deterioration of > 4).
After intracranial hemorrhage and decompressive craniectomy were ruled out, the regimen was switched to a secondary prophylaxis of stent occlusion based on a dual antiplatelet therapy: Under continuous i.v. eptifibatide, patients received a loading dose of 300 mg clopidogrel and 500 mg ASA. Patients with daily ASA medication prior to treatment did not receive an ASA loading dose. The administration of eptifibatide was stopped 4 h after loading with clopidogrel (and ASA). Patients continued with lifelong ASA (100 mg/day) and additional clopidogrel (75 mg/day) for 8 weeks. If a Multiplate® testing 72 h after loading resulted in an insufficient efficacy of clopidogrel (nonresponder), we decided to use prasugrel (10 mg/day) for the duration of 8 weeks.
Clinical Evaluation of Outcome
The NIHSS and modified Rankin Scale (mRS) scores were assessed on admission and discharge. Good functional outcome was defined as mRS score of 0–2 on discharge. Primary endpoints were change in NIHSS and mRS scores between admission and discharge. In case of fatal stroke, no NIHSS score could be assessed at discharge. These patients were completely excluded from NIHSS-related statistics and classified as mRS score 6.
Thrombolysis in myocardial infarction (TIMI) scores of 2 or 3 were defined as successful recanalization. In case of a tandem occlusion, the final grade of recanalization was defined on the basis of the entire result and not separately for the extracranial and intracranial portion. Thus, a successful ICA recanalization in combination with a completely failed recanalization of the carotid-T in a patient resulted in a TIMI grade of 0. We followed up all patients by structured telephone interview in order to assess their mRS scores and any potential history of recurrent stroke.
Results
From October 10, 2009, to March 22, 2011, a total of 50 patients with cerebral artery occlusions were eligible on the basis of the protocol criteria for mechanical thrombectomy with the Solitaire device at the study hospital. Male to female ratio was 34:16. Mean age was 62 years. Forty-one patients had a large artery occlusion in the anterior circulation and nine in the posterior circulation. Mean hospitalization time for the treated patients was 17 days (min. 2 days, max. 89 days).
Anterior Circulation Strokes
The 35 anterior circulation stroke survivors were included in the NIHSS statistics. They had an average NIHSS score of 15.9 on arrival in the emergency department and of 8.5 at hospital discharge, a significant reduction (p = 0.003, Wilcoxon signed-rank test). The corresponding median mRS scores were 5 on admission and 3 on discharge; the improvement was statistically significant (p < 0.01, Wilcoxon signed-rank test). Good immediate (discharge) functional outcome was achieved in 13/41 patients (32 %), including 5 patients (12 %) without any residual symptoms (mRS score, 0).
Technical Success in Anterior Circulation Stroke
Overall, the mechanical recanalization was successful in 35/41 cases (85 %). In detail, the endovascular treatment resulted in TIMI 3 in 23/41 cases (56 %) and TIMI 2 in 12/41 cases (29 %). In the remaining six cases (15 %), the obstructed arteries could not be recanalized (TIMI 1); of these patients only one (Table 1, patient no. 4) had an acute stenting. Interestingly, the restoration of flow in his ICA led to an mRS score of 3 at 90 days, although we were not able to recanalize the subsequent thromboembolic occlusion of his M1 segment. He was also the only patient with a technical complication: the initially placed Wallstent dislocated, resulting in a dissection of the ICA up to the petrous segment. The immediate placement of a self-expandable Protege Stent (ev3 Inc., Plymouth, MN) resulted in a flow restoration. Postinterventionally, he developed a critical edematous swelling based on a partial MCA infarction, requiring decompressive craniectomy. The remaining five patients without flow restoration suffered from a bad clinical outcome: two patients died in the postinterventional course and three patients had an mRS score of 5 at 90 days. Thus, failure to recanalize led to a very bad outcome compared with the successful recanalizations except for the above-mentioned patient with a partial success (recanalization of his ICA).
Mortality in Anterior Circulation Stroke
Six of 41 patients (15 %) died in the acute phase. No death was directly attributable to the endovascular procedure. Mortality in the bridging group was 18 % (6/34) and 0 % (0/7) in the nonbridging group. In 3/6 cases, the etiology was an intracranial hypertension on the basis of malignant territorial infarctions. In the remaining three cases symptomatic intracranial hemorrhage (SICH) was the cause, whereby two hemorrhages occurred within 24 h postinterventionally and one 3 days after recanalization. Thus, two fatal early bleedings in 34 bridging patients may be attributed to the systemic thrombolysis with rTPA, meaning 6 % mortality.
Patients with Acute ICA Stenting
Overall, 17/41 patients (42 %) had to be stented in the extracranial portion of the ICA. In the present cohort, all patients presented with extra- or intracranial tandem occlusions comprising an intracranial thromboembolic occlusion either in the carotid-T or in the M1 segment of the MCA. The additional endovascular procedure led to a prolongation of the mean needle-to-recanalization time of approximately 10 min on average; the delay did not result in a statistically significant difference in mRS or NIHSS outcomes compared with the patients without a priori stenting. All tandem occlusions were treated with a Wallstent in the extracranial ICA portion.
Patients Without Acute ICA Stenting
Twenty-four of 41 patients (58 %) underwent mechanical thrombectomy in the anterior cerebral circulation without extracranial ICA stenting. Baseline variables and results of the two groups are presented in Tables 1 and 2.
Comparison of Subgroups (With vs. Without Acute Stenting) in Anterior Circulation Stroke
Age
The mean age of the patients in the group requiring acute extracranial stenting was 59 years compared with 65 years in the nonstenting group, resulting in a significant intergroup age difference (p = 0.04, Mann–Whitney U test).
Etiology (TOAST Criteria)
The stroke etiology was markedly different between the two groups. While the acute stenting group comprised exclusively thromboembolic causes for stroke, the nonstenting group had almost exclusively cardioembolic stroke etiology (20 cardioembolic, 3 thromboembolic, 1 unclear).
NIHSS Score of Survivors (Admission and Discharge)
There was no statistical difference in baseline NIHSS or mRS scores at admission between the two groups (p = 0.28 and 0.99, respectively, Mann–Whitney U test). The changes in NIHSS scores from hospital admission to discharge were recorded for all patients. The NIHSS scores showed significant improvement in the stenting group (median NIHSS score from 17 to 6, p = 0.003, Wilcoxon signed-rank test) as well as in the nonstenting group (median NIHSS score from 15.5 to 4, p = 0.0004, Wilcoxon signed-rank test). Comparison of the changes between the stenting vs. the nonstenting group showed no statistical difference (p = 0.67, Mann–Whitney U test).
Immediate Outcome (mRS Admission and Discharge)
On discharge, 5/17 patients (29 %) in the acute stenting group had a good outcome. This was true for 8/24 patients (33 %) in the group without acute stenting. Each group showed a significant amelioration of mRS scores (stent group: median mRS score from 5 to 3, p = 0.03; nonstent group: median mRS score from 5 to 3, p = 0.008; Wilcoxon signed-rank test each). The comparison of the mRS changes between the groups was indifferent (p = 0.87, Mann–Whitney U test).
Recanalization
The recanalization rate was 16/17 (94 %) and 19/24 (79 %) in the group with and without acute stenting, respectively. Successful recanalization was significantly associated with the degree of mRS improvement (p = 0.01, Mann–Whitney U test). For the surviving patients with successful recanalization (n = 39), the mean NIHSS score improvement was 8.8; however, for nonrecanalized survivors (n = 4), the mean NIHSS score worsened by 0.3 points.
Bridging
In the acute stenting group, 14/17 patients (82 %) were bridged with i.v. rTPA. This was true for 20/24 patients (83 %) in the nonstenting group. There was no difference in the rate of i.v. thrombolysis between groups.
Antiplatelet Regimen
The described antiplatelet regimen, comprising the acute phase and a secondary prophylaxis of in-stent thrombosis, did not lead to an increased rate of SICH postinterventionally. During the acute phase and the follow-up, we found no clinical evidence for acute in-stent thrombosis. The restroke rate during follow-up was not increased in either group.
Follow-up
In the follow-up, 90-day data could be obtained for all 35 patients who survived the acute phase. The median follow-up mRS score of these initial stroke survivors was 3 at the time of hospital discharge as well as on follow-up. However, there was, significant amelioration in mRS scores during follow-up time, when statistically tested (p = 0.02, Wilcoxon signed-rank test).
Three of 35 patients (9 %) died during follow-up: one of a previously undiagnosed metastatic cancer of the prostate, one of a heart attack, and 1 of unclear cause of death. Of the remaining 32 patients, 7/13 (54 %) treated with acute stenting had a good functional outcome and 11/13 (85 %) were able to walk without assistance at 90 days. In the subgroup without acute stenting, 8/19 (42 %) had a good functional outcome and 12/19 (63 %) were able to walk independently at 90 days.
Four of 35 patients suffered a new stroke or transient ischemic attack (TIA) during follow-up. Two of the recurrent strokes affected vessel territories different from the ones originally treated. The two recurrent vessel occlusions lead to a new stroke in the previously recanalized territories of the respective MCA. The etiology in both cases was cardioembolic. One event occurred after the patient had discontinued oral anticoagulation despite a proven ventricular thrombus after myocardial infarction; the other patient also had a proven cardioembolic cause for the primary stroke, but received ASA (300 mg/day) instead of phenprocoumone because of repeated drop attacks. Consequently, these events were not attributable to the prior mechanical recanalization.
Discussion
The study contains an analysis of 50 consecutive patients fulfilling the inclusion criteria, focusing on the initial and midterm results of 17 patients, which had to be stented in the extracranial portion of the ICA before intracranial clot removal either in the carotid-T or M1 segments. In recent times multiple stent retriever designs have been introduced after initial encouraging results with the Solitaire, e.g., Trevo (Concentric Medical, Mountain View, CA), Revive (Codman & Shurtleff Inc., Raynham, MA), and Capture (Mindframe, Irvine, CA). However, to date, there is no clinical trial that has demonstrated that any intra-arterial revascularization device improves clinical outcome in acute stroke patients compared with i.v. rTPA within 4.5 h. Most experiences have been published about the performance of the Solitaire; the available data consist of small initial case series [5–10], including a systematic review [11], larger prospective single-center case series [12, 13], and single-center retrospective analysis in more than 100 patients [14], as well as a retrospective multicenter study [15]. The reported recanalization rates (technical success) vary between 60 and 90 %. There is though no consistency in the reported grading systems, including references in TIMI or thrombolysis in cerebral infarction (TICI) or modified TICI scales. The reported rate of good neurological outcome varies between 40 and 60 % at 90 days, depending on the inclusion criteria and time frames [11–13, 15]. Recently, the superiority of the Solitaire has been shown in a randomized trial against the MERCI device [3].
The present cohort features an unusually high percentage (42 %) of consecutive patients treated for tandem occlusions. The data on endovascular therapy for tandem occlusion in acute stroke is scarce. Initial case reports and small series on the results of an immediate endovascular recanalization of an obstructed extracranial ICA in acute stroke [16–20] reported technical success rates between 84 and 100 % and a good clinical outcome in 50–60 % after 90 days. Pertaining to the more severe tandem occlusions, there are two recent retrospective reports about endovascular treatment results before the advent of stent retrievers. In these studies the concomitant intracranial occlusion was either treated by intra-arterial thrombolysis or first-generation devices (e.g., MERCI) or a combination of both. Malik et al. [21] reported a mean NIHSS score of 15 on admission. Proximal revascularization was successful in 100 % of cases, which is consistent with previous reports. However, the intracranial recanalization rate was only 58 % in case of a concomitant carotid-T obstruction; in case of a M1 obstruction, it increased to 79 %. The rate of good outcome is not given for each subgroup, only the overall rate of 42 % is reported. Mortality was 25 % at 90 days [21]. Hauck et al. [22] had a mean NIHSS score of 14 at admission, a recanalization rate of 68 % (15/22 patients) in case of a tandem occlusion, and a good outcome in 50 % (11/22) at 9 months. Mortality rate was 32 % [22].
To our knowledge, the present series is the largest to date featuring 17 consecutive tandem occlusions treated with emergency extracranial ICA stenting followed by intracranial thrombectomy exclusively with the Solitaire stent retriever. There is only one study by Cohen et al. [23] with comparable inclusion criteria, featuring seven tandem occlusions where the Solitaire was used exclusively for intracranial clot retrieval in conjunction with an extracranial Wallstent. The main difference is that Cohen et al. used a second endovascular approach (thrombectomy followed by extracranial stenting) in some patients alternatively. They conclude, though, that proximal angioplasty and distal stent retriever–based thrombectomy was the fastest and most effective approach in terms of recanalization in tandem occlusions. The experience derived from the present series supports this technical conclusion.
Clinically, tandem occlusions usually result in major acute stroke, leading to a severe disability or death [24, 25]. In the present study, we observed a high recanalization rate of 94 % in tandem occlusions, leading to a good outcome in 54 % at 90 days. The door-to-recanalization time was not significantly prolonged compared with the nonstenting group. The mortality rate was low compared with the literature, which was 15 % overall in the acute phase. No death was attributable to a procedural complication. Of three intracranial hemorrhages, two are most probably attributable to concomitant i.v. thrombolysis; no increased hemorrhage rate was observed in the course of the described periprocedural antiplatelet regimen in acute stenting for tandem occlusions, which is consistent with previous reports [26, 21, 27]. Thus, the main finding in the present series is that stent-assisted endovascular recanalization of the extracranial ICA followed by a stent retriever (Solitaire)-based thrombectomy either in the carotid-T or M1 segments in the setting of acute stroke is technically feasible; the recanalization rate is high and the procedure is not associated with a significantly increased risk when compared with i.v. rTPA alone.
The follow-up showed two strokes in the territory of the originally treated vessels both of which have to be considered cardioembolic. We observed no increased risk for a recurrent stroke in the treated arterial territories at 90 days in either group compared with conservative treatment alone [28].
The present study is limited by its design as a subgroup analysis from an original prospective study to evaluate the technical and clinical success of emergency mechanical thrombectomy in acute stroke with the solitaire stent retriever. Furthermore, patients’ age, sex, and stroke etiology are distributed unequally between the extracranial stenting and nonstenting groups. These differences in baseline variables, however, result in the need for combined extracranial stenting and intracranial thrombectomy in the first place. Carotid stenosis due to atherosclerosis is the major underlying pathophysiology of tandem occlusions, hence the different distributions of stroke etiology. As male sex is a risk factor for atherosclerosis and age a risk factor for atrial fibrillation and thus cardioembolic stroke, the group differences in these items seem inevitable in any kind of noncontrolled trial as well. The strong points of this study are the high rate of tandem occlusions treated, the consecutive inclusion of all patients according to the inclusion criteria on an intention-to-treat basis, the prospective assessment of outcome variables, the evaluation of clinical as well as technical outcome, and the high follow-up rate.
Conclusion
In our study on stent retriever (Solitaire)-based mechanical revascularization, we observed an unusually high rate of tandem occlusions in acute stroke. Our data suggest that acute extracranial stenting in this setting combined with intracranial Solitaire-based thrombectomy is safe and may lead to an improvement in neurological outcome in patients with an otherwise poor prognosis under i.v. thrombolysis alone. The endovascular manipulation did not increase the risk for recurrent stroke during follow-up.
Conflict of Interest
MB and HB have no conflicts of interest. AM and WW received travel grants from ev3 Inc. (Plymouth, MN). The present study was not financially supported.
Abbreviations
- VA:
-
Vertebral artery
- PCA:
-
Posterior cerebral artery
- BA:
-
Basilar artery
- TIMI:
-
Thrombolysis in myocardial infarction
- OTR:
-
Time interval from onset to recanalization
- SICH:
-
Symptomatic intracranial hemorrhage
References
Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38(3):967–73.
Saqqur M, Uchino K, Demchuk AM, Molina CA, Garami Z, Calleja S, et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007;38(3):948–54.
Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012;380(9849):1240–9.
Pancioli AM, Broderick J, Brott T, Tomsick T, Khoury J, Bean J, et al. The combined approach to lysis utilizing eptifibatide and rt-PA in acute ischemic stroke: the CLEAR stroke trial. Stroke. 2008;39(12):3268–76.
Castano C, Dorado L, Guerrero C, Millan M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010;41(8):1836–40.
Miteff F, Faulder KC, Goh AC, Steinfort BS, Sue C, Harrington TJ. Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB): experience in 26 patients with acute cerebral artery occlusion. Am J Neuroradiol. 2011;32(6):1078–81.
Mpotsaris A, Bussmeyer M, Loehr C, Oelerich M, Buchner H, Weber W. Mechanical thrombectomy in severe acute stroke: preliminary results of the Solitaire stent. J Neurol Neurosurg Psychiatry. 2012;83(1):117–8.
Nayak S, Ladurner G, Killer M. Treatment of acute middle cerebral artery occlusion with a Solitaire AB stent: preliminary experience. Br J Radiol. 2010;83(996):1017–22.
Park H, Hwang GJ, Jin SC, Jung CK, Bang JS, Han MK, et al. A retrieval thrombectomy technique with the Solitaire stent in a large cerebral artery occlusion. Acta Neurochir (Wien). 2011;153(8):1625–31.
Stampfl S, Hartmann M, Ringleb PA, Haehnel S, Bendszus M, Rohde S. Stent placement for flow restoration in acute ischemic stroke: a single-center experience with the Solitaire stent system. Am J Neuroradiol. 2011;32(7):1245–8.
Koh JS, Lee SJ, Ryu CW, Kim HS. Safety and efficacy of mechanical thrombectomy with solitaire stent retrieval for acute ischemic stroke: a systematic review. Neurointervention. 2012;7(1):1–9.
Costalat V, Machi P, Lobotesis K, Maldonado I, Vendrell JF, Riquelme C, et al. Rescue, combined, and stand-alone thrombectomy in the management of large vessel occlusion stroke using the solitaire device: a prospective 50-patient single-center study: timing, safety, and efficacy. Stroke. 2011;42(7):1929–35.
Machi P, Costalat V, Lobotesis K, Maldonado IL, Vendrell JF, Riquelme C, et al. Solitaire FR thrombectomy system: immediate results in 56 consecutive acute ischemic stroke patients. J Neurointerv Surg. 2012;4(1):62–6.
Dorn F, Stehle S, Lockau H, Zimmer C, Liebig T. Endovascular treatment of acute intracerebral artery occlusions with the solitaire stent: single-centre experience with 108 recanalization procedures. Cerebrovasc Dis. 2012;34(1):70–7.
Davalos A, Pereira VM, Chapot R, Bonafe A, Andersson T, Gralla J. Retrospective multicenter study of Solitaire FR for revascularization in the treatment of acute ischemic stroke. Stroke. 2012;43(10)2699–705.
Dabitz R, Triebe S, Leppmeier U, Ochs G, Vorwerk D. Percutaneous recanalization of acute internal carotid artery occlusions in patients with severe stroke. Cardiovasc Intervent Radiol. 2007;30(1):34–41.
Du Mesnil De Rochemont R, Sitzer M, Neumann-Haefelin T, Harmjanz A, Berkefeld J. Endovascular recanalization of acute atherothrombotic carotid artery occlusion holds up progressive stroke. Neuroradiology. 2004;46(7):583–6.
Imai K, Mori T, Izumoto H, Watanabe M, Majima K. Emergency carotid artery stent placement in patients with acute ischemic stroke. Am J Neuroradiol. 2005;26(5):1249–58.
Jovin TG, Gupta R, Uchino K, Jungreis CA, Wechsler LR, Hammer MD, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke. 2005;36(11):2426–30.
Nedeltchev K, Brekenfeld C, Remonda L, Ozdoba C, Do DD, Arnold M, et al. Internal carotid artery stent implantation in 25 patients with acute stroke: preliminary results. Radiology. 2005;237(3):1029–37.
Malik AM, Vora NA, Lin R, Zaidi SF, Aleu A, Jankowitz BT, et al. Endovascular treatment of tandem extracranial/intracranial anterior circulation occlusions: preliminary single-center experience. Stroke. 2011;42(6):1653–7.
Hauck EF, Natarajan SK, Ohta H, Ogilvy CS, Hopkins LN, Siddiqui AH, et al. Emergent endovascular recanalization for cervical internal carotid artery occlusion in patients presenting with acute stroke. Neurosurgery. 2011;69(4):899–907; discussion 907.
Cohen JE, Gomori M, Rajz G, Moscovici S, Leker RR, Rosenberg S, et al. Emergent stent-assisted angioplasty of extracranial internal carotid artery and intracranial stent-based thrombectomy in acute tandem occlusive disease: technical considerations. J Neurointerv Surg. 2012 (in press).
Adams HP Jr, Bendixen BH, Leira E, Chang KC, Davis PH, Woolson RF, et al. Antithrombotic treatment of ischemic stroke among patients with occlusion or severe stenosis of the internal carotid artery: A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology. 1999;53(1):122–5.
Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, et al. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006;37(9):2301–5.
Akbari SH, Reynolds MR, Kadkhodayan Y, Cross DT 3rd, Moran CJ. Hemorrhagic complications after prasugrel (Effient) therapy for vascular neurointerventional procedures. J Neurointerv Surg. 2012 (in press).
Stetler WR, Chaudhary N, Thompson BG, Gemmete JJ, Maher CO, Pandey AS. Prasugrel is effective and safe for neurointerventional procedures. J Neurointerv Surg. 2012 (in press).
Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363(9411):768–74.
Acknowledgments
AM and MB contributed equally to the manuscript. No other persons apart from the authors have made substantial contributions to this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mpotsaris, A., Bussmeyer, M., Buchner, H. et al. Clinical Outcome of Neurointerventional Emergency Treatment of Extra- or Intracranial Tandem Occlusions in Acute Major Stroke: Antegrade Approach With Wallstent and Solitaire Stent Retriever. Clin Neuroradiol 23, 207–215 (2013). https://doi.org/10.1007/s00062-013-0197-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-013-0197-y