Abstract
Objective
Magnetic resonance spectroscopy (MRS) is a powerful tool for preoperative grading of gliomas. We performed a meta-analysis to evaluate the diagnostic performance of MRS in differentiating high-grade gliomas (HGGs) from low-grade gliomas (LGGs).
Methods
PubMed and Embase databases were systematically searched for relevant studies of glioma grading assessed by MRS through 27 March 2015. Based on the data from eligible studies, pooled sensitivity, specificity, diagnostic odds ratio and areas under summary receiver operating characteristic curve (SROC) of different metabolite ratios were obtained.
Results
Thirty articles comprising a total sample size of 1228 patients were included in our meta-analysis. Quantitative synthesis of studies showed that the pooled sensitivity/specificity of Cho/Cr, Cho/NAA and NAA/Cr ratios was 0.75/0.60, 0.80/0.76 and 0.71/0.70, respectively. The area under the curve (AUC) of the SROC was 0.83, 0.87 and 0.78, respectively.
Conclusions
MRS demonstrated moderate diagnostic performance in distinguishing HGGs from LGGs using tumoural metabolite ratios including Cho/Cr, Cho/NAA and NAA/Cr. Although there was no significant difference in AUC between Cho/Cr and Cho/NAA groups, Cho/NAA ratio showed higher sensitivity and specificity than Cho/Cr ratio and NAA/Cr ratio. We suggest that MRS should combine other advanced imaging techniques to improve diagnostic accuracy in differentiating HGGs from LGGs.
Key points
• MRS has moderate diagnostic performance in distinguishing HGGs from LGGs.
• There is no significant difference in AUC between Cho/Cr and Cho/NAA ratios.
• Cho/NAA ratio is superior to NAA/Cr ratio.
• Cho/NAA ratio shows higher sensitivity and specificity than Cho/Cr and NAA/Cr ratios.
• MRS should combine other advanced imaging techniques to improve diagnostic accuracy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gliomas are the most common primary neoplasm of the central nervous system, and the prognosis for this disease remains very poor [1]. In determining a treatment plan, tumour grade is a key consideration for minimizing the risk of unnecessary morbidity and mortality [2].
Given the limitations of conventional MRI in distinguishing low-grade gliomas (LGGs) from high-grade gliomas (HGGs) (accuracy between 55 % and 83 %), advanced multiparametric magnetic resonance (MR) techniques have been explored, including diffusion-weighted imaging (DWI), diffusion tensor imaging (DTI), proton MR spectroscopy (MRS) and perfusion imaging [3]. Because of its safety and non-invasive nature, MRS is of great advantage in patients with brain gliomas [4, 5]. MRS provides information about metabolic tissue composition, and advanced spectroscopic methods have been used to quantify markers of tumour metabolism (e.g. glucose), membrane turnover and proliferation (e.g. choline [Cho]), energy homoeostasis (e.g. creatine [Cr]), intact glioneuronal structures (e.g. N-acetyl-aspartate [NAA]) and necrosis (e.g. lactate [Lac] or lipids) [6]. Results are usually expressed as ratios between cerebral metabolites rather than absolute concentrations [7].
Numerous studies have evaluated the diagnostic accuracy of 1H-MR spectroscopy for distinguishing high- and low-grade gliomas. A systematic literature review [8] was performed approximately 10 years ago in order to provide evidence, but the interpretation was limited by the small number of studies and small sample sizes. In the current work, we performed a meta-analysis to measure the diagnostic performance of MRS in differentiating high- from low-grade gliomas.
Materials and methods
Search strategy
The PubMed and Embase databases were systematically searched to find relevant published articles (through 27 March 2015). We used the following keywords: (“magnetic resonance spectroscopy” or “MR spectroscopy” or “MRS”) AND (glioma). Additionally, the reference lists of all retrieved articles were checked for other eligible reports that were not identified in the initial search.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) MRS was used to differentiate HGGs from LGGs in patients with no clinical history of previous surgery, chemotherapy or radiotherapy; (2) the diagnostic criteria of glioma grading were clearly stated, and the number of LGGs and HGGs could be obtained; (3) at least one individual metabolite ratio was used to evaluate the grading of glioma; (4) values of true positive (TP), false positive (FP), false negative (FN), true negative (TN), sensitivity (SEN), specificity (SPE), positive likelihood ratio (LR+) and negative likelihood ratio (LR−) could be accurately calculated from the data reported; (5) at least seven patients were included; (6) pathology and/or clinical follow-up were used as the reference standard; (7) no data were overlapping; and (8) only English language full-text publications were included. The following were excluded: animal studies, abstracts, reviews, case report, letters, editorials, comments and conference proceedings.
Two authors (Q. Wang and H. Zhang) independently evaluated potentially relevant articles using the inclusion and exclusion criteria. If no agreement could be reached between these two authors, inconsistencies were discussed and resolved by a third author (B.N. Xu).
Data extraction and quality assessment
The screened articles were assessed independently by the same two authors (J.S. Zhang and X.L. Chen). For each included study, basal characteristics (authors, year of publication and country of origin), patient characteristics (number, mean age, sex, and grade of glioma) and technical aspects (imaging field strength, techniques of spectrum acquisition, device parameters, metabolite ratios, cut-off value, metabolite ratio mean value in different grades of glioma and reference standard) were noted. HGGs (grade III–IV gliomas) were considered positive; LGGs (grade I–II gliomas) were considered negative. The number of TP, FP, FN and TN results were calculated and recorded. The methodological quality of the studies was assessed using the Quality Assessment Tool for Diagnostic Accuracy Studies version 2 (QUADAS-2) [9]. Disagreements were resolved by consensus.
Statistical analysis
Standard methods recommended for meta-analysis diagnostic accuracy were used [10, 11]. First, heterogeneity was evaluated between studies in which this may have been caused by a threshold effect. A Spearman correlation coefficient was computed between the logit of SEN and the logit of (1 − SPE) to assess the threshold effect, and the extent of heterogeneity was then assessed using the chi-square value test and the inconsistency index (I2) of the diagnostic odds ratio (DOR). The existence of significant heterogeneity necessitated the use of a random-effects coefficient binary regression model when the test performance was summarized; otherwise, a fixed-effects coefficient binary regression model was used [12, 13].
The pooled SEN, SPE, LR+, LR− and DOR, with their 95 % confidence intervals (CIs), were calculated for each study. The summary receiver-operating characteristic curve (SROC), area under the curve (AUC) and Q* index were calculated. AUC values of 51–70 %, 71–90 %, and >90 % indicated low, moderate and high diagnostic accuracy, respectively.
Subgroup analysis was performed when some homogenous set of studies adopted similar design variables. Subgroups were constructed only when more than three studies could be included. Tests of interaction were performed to assess differences between subgroups [14]. The above-mentioned statistical analyses were performed using Meta-DiSc statistical software version 1.4 [11].
Publication bias was assessed by Deeks’ funnel plot. Formal testing for publication bias was conducted using a regression of the diagnostic log odds ratio against ESS1/2 (effective sample size) and weighting according to the effective sample size, with P < 0.10 indicating significant asymmetry [15]. This statistical analysis was performed using Stata 12.0 software (StataCorp LP, College Station, TX, USA).
Results
Study selection and characteristics
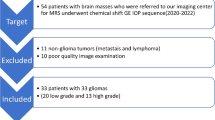
The study selection process is described in Fig. 1. The systematic literature search included 30 articles [16–45] comprising a total sample of 1335 patients (1228 patients with MRS of appropriate quality) with radiologically suspected untreated glioma. The detailed characteristics of the included studies are listed in Table 1.
Among these studies, 25 were retrospective cohort studies, and only five studies were prospective. In 1228 patients with MRS of appropriate quality, there were 426 LGGs and 802 HGGs. The detailed grading of HGGs was available in all but two studies [17, 25]. Histological results obtained from either surgical biopsy and/or resection were the main reference standard in all studies. Both pathology and clinical follow-up combined with radiological follow-up were used as reference standard in three studies [17, 19, 21].
Most studies used a single metabolite ratio, while five articles used only combined diagnostic thresholds, i.e. Cho/Cr >1.2 and the presence of a lipid/lactate peak [19], either Cho/Cr ratio or Cho/NAA ratio > 1.5 or the presence of lactate or lipids [24], Cho/Pcr-Cr and reduced NAA [41], Cho/Cr and/or LL/Cr [36], and Cho/Cr and NAA/Cho [43].
The risk of bias and concerns regarding the applicability of the studies are shown in Fig. 2. In most studies, the risk of bias was low or unclear. Three studies in which patients received a different reference standard were considered to have a high risk of bias.
Quantitative synthesis
Cho/Cr ratio
Overall, among 19 of the included studies, a total of 852 MRS examinations of good quality were performed for the detection of HGGs by calculating the Cho/Cr ratio [16–18, 20, 22, 23, 25, 27, 28, 30, 31, 33–35, 38–40, 42, 45]. The diagnostic threshold of Cho/Cr ranged between 0.49 and 2.07. The Spearman correlation coefficient was 0.085 (P = 0.73), which indicated that there was no obvious threshold effect in the estimates of accuracy. Significant heterogeneity was observed in the overall comparisons (I2 = 59 %), and therefore the test performance was summarized using a random-effects coefficient binary regression model.
The pooled weighted values were determined as follows: SEN, 0.75 (95 % CI: 0.71, 0.79); SPE, 0.60 (95 % CI: 0.55, 0.66); LR+, 2.78 (95 % CI: 1.62, 4.76); LR−, 0.35 (95 % CI: 0.25, 0.49); and DOR, 8.53 (95 % CI: 4.39, 16.59). The forest plots from 19 studies are shown in Fig. 3A. The AUC under the SROC was 0.83 (Fig. 4A). A total of 313 MRS examinations among six studies were performed on 1.5-T scanners [27, 34, 39, 40, 42, 45]. A 3.0-T unit was used for 539 scans among 13 studies [16–18, 20, 22, 23, 25, 27, 28, 30, 31, 33–35, 38–40, 42, 45] that were included. There was no significant difference in AUC between the 1.5-T and 3.0-T subgroups (Pinteraction = 0.77).
Next, we performed subgroup analyses by spectrum acquisition technique (multi-voxel spectroscopy [MVS] and single-voxel spectroscopy [SVS]) and echo time of the spectroscopic sequence (short echo time [STE] and long echo time [LTE]). There was no significant difference in the AUC between the MVS and SVS groups (Pinteraction = 0.96) or the STE and LTE groups (Pinteraction = 0.90). The results of the included studies and subgroup analyses of diagnostic accuracy variables are summarized in Table 2.
Cho/NAA ratio
A total of 603 MRS examinations were analyzed among 16 studies [26–33, 35, 37, 39–42, 44, 45] to detect HGGs from LGGs by calculating the Cho/NAA ratio. The diagnostic threshold of Cho/NAA ranged between 0.80 and 3.77. No threshold effect (P = 0.27) or heterogeneity (I2 = 34 %) was found among individual studies. The pooled SEN and SPE values were 0.80 (95 % CI: 0.76, 0.84) and 0.76 (95 % CI: 0.70, 0.82), respectively (Fig. 3B).The AUC under the SROC was 0.87 (Fig. 4B). The pooled SEN, SPE, LR+, LR−, DOR and AUC are summarized in Table 2. No significant difference in AUC was detected between the 1.5-T and 3.0-T subgroups (Pinteraction = 0.76) or the MVS and SVS subgroups (Pinteraction = 0.35).
NAA/Cr ratio
Ten studies [16, 28–30, 33, 34, 38, 40, 44, 45] including 333 MRS examinations were conducted in which HGGs were detected by calculating the NAA/Cr ratio. The diagnostic threshold of NAA/Cr ranged between 0.44 and 2.44. Here there was also no threshold effect (P = 0.35) or heterogeneity (I2 = 0.0 %) found among individual studies. The pooled SEN and SPE were 0.71 (95 % CI: 0.65, 0.77) and 0.70 (95 % CI: 0.61, 0.78), respectively (Fig. 3C).The AUC under the SROC was 0.78 (Fig. 4C). No significant difference in AUC was detected between the 1.5-T and 3.0-T subgroups (Pinteraction = 0.39) or the MVS and SVS subgroups (Pinteraction = 0.31).
LL/Cr
Only two studies [20, 36] had been performed in which HGGs were detected by calculating the ratio of lipids and lactate (LL)/Cr. Quantitative synthesis of studies measuring other metabolite ratios was impossible because of limited data. Finally, we compared the AUCs among the three groups, which revealed significant differences in AUC between the Cho/NAA and NAA/Cr groups (Pinteraction = 0.03).
Sensitivity analysis
Among the 19 included studies in which HGGs were detected by calculating the Cho/Cr ratio, the DOR values were greater than 1.0 in all but two studies [17, 34], which were then excluded from the sensitivity analysis. The corresponding pooled SEN, SPE, LR+, LR− and DOR were 0.74 (95 % CI: 0.70, 0.78), 0.72 (95 % CI: 0.65, 0.77), 2.8 (95 % CI: 2.02, 3.88), 0.31 (95 % CI: 0.22, 0.43) and 10.92 (95 % CI: 6.26, 19.06), respectively. The AUC under the SROC was 0.84, which was not materially different from the overall AUC (0.83), indicating that our results were statistically robust.
Heterogeneity analysis and publication bias
Significant heterogeneity was present in the pooled analysis in the Cho/Cr group that could not be explained by threshold effect. Meta-regression analysis showed that factors including year of publication, country, study design, compact surface, voxel, and echo time did not contribute to heterogeneity. There was no significant heterogeneity in the pooled analysis in the Cho/NAA and NAA/Cr groups.
The Deeks’ funnel plot asymmetry test for the overall analysis in the Cho/Cr, Cho/NAA and NAA/Cr groups showed that publication bias may have existed in Cho/Cr and Cho/NAA groups (P = 0.01 and 0.02, respectively) (Fig. 5A, B), while the NAA/Cr group showed no significant publication bias (P = 0.31) (Fig. 5C).
Discussion
Metabolic ratios of MRS have been frequently used to differentiate glioma grade among numerous studies. In an earlier article [8], the sensitivity and specificity of MRS was reviewed only in terms of differentiating high- from low-grade tumours. A recently published meta-analysis [46] concluded that MRS demonstrated moderate sensitivity and specificity for discriminating brain tumours (pooled estimates of 80.58 % and 78.46 %, respectively). The chief problem in this meta-analysis is that the authors combined all related articles without identifying gliomas from brain tumours or differentiating metabolite ratios used in each study, which would inevitably increase heterogeneity and render the conclusion unreliable [7]. We performed the present systematic review and meta-analyses based on accurate calculations of the relevant data.
Cho/Cr ratio
According to the quantitative synthesis, the AUC of the SROC curve was 0.83, suggesting a moderate level of overall accuracy. The DOR is a single indicator of test accuracy that combines the SEN and SPE data into a single number [47]. In this meta-analysis, the pooled DOR for diagnostic accuracy of glioma grading using the Cho/Cr ratio was 8.53, indicating that this ratio may be helpful in the diagnosis of glioma grade. As the likelihood ratios are considered clinically more meaningful than SROC curve and DOR, both LR+ and LR− were also calculated to assess diagnostic accuracy. An LR+ of 2.78 suggests that HGG patients have about threefold higher odds of a positive test (> cut-off value) than LGG patients. On the other hand, the LR− was 0.35, suggesting that with a low cut-off value for the Cho/Cr ratio, the probability of HGG for this patient would be 35 %, which is not low enough to rule out HGG.
The results of subgroup analysis showed no significant difference in diagnostic accuracy between 3.0-T and 1.5-T MRS. However, in light of the limited data, further verification of these results is needed. The diagnostic performance of both the MVS and SVS techniques in distinguishing HGGs from LGGs was mediocre, and showed no statistical difference in either LTE or STE subgroup.
Significant heterogeneity was observed in the overall comparisons that could not be explained by threshold effect. Despite performing meta-regression analysis, we were unable to find the source of the heterogeneity. There may be publication bias with regard to the Cho/Cr ratio (Fig. 5A), as the results of Deeks’ funnel plot asymmetry test (P = 0.01) indicated that only small studies with high accuracy had been reported, while small studies with lower accuracy likely had not.
Cho/NAA ratio
For the Cho/NAA ratio, the AUC (0.87) indicated a moderate level of overall accuracy. The pooled DOR of diagnostic accuracy for HGG detection by the Cho/NAA ratio was 11.95, indicating that the ratio may be helpful in the diagnosis of HGGs. No statistically significant difference in diagnostic accuracy was detected between the 1.5-T and 3.0-T or MVS and SVS subgroups. Because of the limited STE study data, we were unable to compare the diagnostic performance of the Cho/NAA ratio between LTE and STE. No heterogeneity was present in the overall comparisons, but publication bias may exist, due to the small study effects (the tendency for the small studies in a meta-analysis to show high accuracy).
NAA/Cr ratio
With regard to the NAA/Cr ratio, the AUC (0.78) indicated a moderate level of overall accuracy. The summary DOR of the diagnostic accuracy of the Cho/NAA ratio in detecting HGGs was 6.67, indicating that the ratio may be helpful in diagnosing HGGs. No statistically significant difference in diagnostic accuracy was detected between the 1.5-T and 3.0-T or MVS and SVS subgroups. Heterogeneity and publication bias was not present in the overall comparisons, indicating that the results for the NAA/Cr ratio in our meta-analysis were statistically robust.
Overall comparisons between different metabolite ratios
Several studies have strongly recommended the use of the Cho/NAA ratio rather than the Cho/Cr ratio for differentiating HGGs from LGGs [44, 48–50], and one study noted no significant differences in the tumoural Cho/Cr ratio between LGGs and HGGs [48]. Cho/Cr is the ratio most frequently used, as mentioned in an overview of MRS [51] and supported by other authors [52, 53]. This ratio has also demonstrated reasonably low overall error during image processing [54]. Another reason for its use is that creatine concentration is known to be relatively stable during the formation of the anaplastic foci, in contrast to Cho concentration, which increases progressively [4]. However, this is a controversial issue, and one study [55] showed that creatine can change during the course of glioma development, and that creatine concentration can even carry prognostic information.
It is noteworthy that our meta-analysis showed no significant difference in AUC between the Cho/Cr and Cho/NAA groups (Pinteraction > 0.05) or between the Cho/Cr and NAA/Cr groups, but that there was a significant difference in AUC between the Cho/NAA and NAA/Cr groups (Pinteraction < 0.05), thus demonstrating that the Cho/NAA ratio has higher diagnostic accuracy than the NAA/Cr ratio in distinguishing HGGs from LGGs.
Based on the overall study results, the sensitivity and specificity of glioma grade diagnosis was higher for the Cho/NAA ratio (SE = 0.80, SP = 0.76) than the Cho/Cr ratio (SE = 0.75, SP = 0.60) or NAA/Cr ratio (SE = 0.71, SP = 0.70). Taking this diagnostic performance into consideration, the Cho/NAA ratio may be a superior index for distinguishing HGGs from LGGs. However, given the limited data, further study is needed to confirm the efficacy of the Cho/NAA ratio.
Limitations
Although the present meta-analysis revealed moderate overall diagnostic accuracy for MRS in distinguishing HGGs from LGGs, some design limitations should be taken into consideration when interpreting our results.
First, most of the included articles focused on the diagnostic efficiency of a single metabolite ratio. The standards combined different metabolites with metabolite ratios in distinguishing HGGs from LGGs, but these were not well established. Thus it was difficult to perform an accurate statistical analysis, as it was not known whether combined standards could improve diagnostic accuracy. In addition, the focus of the analysis was the superior metabolite ratios of tumour tissue, and comparisons between tumour tissue and healthy tissue were lacking, which may have led to lower specificity.
Second, as mentioned above, several innovative and advanced multiparametric magnetic resonance techniques, including DWI, DTI, and MR perfusion and multimodal imaging including PET/SPECT, also help to distinguish HGGs from LGGs. Though it is controversial which imaging technique is superior, most authors concluded that combined techniques would improve diagnostic accuracy [17, 22, 29, 34, 54].
Third, heterogeneity was found among the Cho/Cr ratio groups, and factors such as sample size, patient age and glioma grade may have also contributed to heterogeneity. Although heterogeneity was not present in the other two groups, there was considerable variation in study design, such as different types of coils, MRI devices and diverse methods of determining cut-off values. Fourth, there may have been publication bias regarding the Cho/Cr and Cho/NAA groups. Our meta-analysis was based only on published studies, which tend to report high accuracy; studies with lower accuracy are often rejected or not even submitted. In addition, this review was restricted to full-text articles published in English, thus omitting eligible studies that were unpublished or reported in other languages, which also likely resulted in bias.
Fifth, different spectroscopic patterns of glial tumour grades were not reflected. High-grade tumours in these studies represented grade III and IV cases grouped together, whereas a major diagnostic challenge sometimes is differentiating grade II from grade III and grade III from grade IV. Dividing the subgroups would have changed the cut-off threshold. Finally, the studies with small sample sizes would be greatly affected by adding 0.5 to each cell of the study to correct for zero entries in order to avoid potential problems in odds calculations for studies with sensitivity or specificity of 100 %.
In conclusion, this meta-analysis provides evidence that MRS has moderate diagnostic performance in distinguishing HGGs from LGGs using tumoural metabolite ratios. The Cho/NAA ratio is superior to the NAA/Cr ratio in differentiating between HGGs and LGGs. We suggest that MRS should be combined with other advanced imaging techniques in order to improve diagnostic accuracy.
Abbreviations
- AUC:
-
Area under the curve
- Cho:
-
Choline
- CI:
-
Confidence intervals
- Cr:
-
Creatine
- DOR:
-
Diagnostic odds ratio
- DTI:
-
Diffusion tensor imaging
- DWI:
-
Diffusion-weighted imaging
- FN:
-
False negative
- FP:
-
False positive
- HGGs:
-
High-grade gliomas
- I2 :
-
Inconsistency index
- Lac:
-
Lactate
- LGGs:
-
Low-grade gliomas
- LL:
-
Lipids and lactate
- LR+:
-
Positive likelihood ratio
- LR−:
-
Negative likelihood ratio
- LTE:
-
Long echo time
- MI:
-
Myo-inositol
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- MVS:
-
Multi-voxel spectroscopy
- NAA:
-
N-acetyl-aspartate
- nCho:
-
Normalized choline
- nCr:
-
Normalized creatine
- Pcr:
-
Phosphocreatine
- PET:
-
Positron-emission tomography
- QUADAS-2:
-
Quality Assessment Tool for Diagnostic Accuracy Studies version 2
- SEN:
-
Sensitivity
- SPE:
-
Specificity
- SPECT:
-
Single photon mission computed tomography
- SROC:
-
Summary receiver-operating characteristic curve
- STE:
-
Short echo time
- SVS:
-
Single-voxel spectroscopy
- TN:
-
True negative
- TP:
-
True positive
References
Inoue T, Ogasawara K, Beppu T, Ogawa A, Kabasawa H (2005) Diffusion tensor imaging for preoperative evaluation of tumor grade in gliomas. Clin Neurol Neurosurg 107:174–180
Lu H, Pollack E, Young R et al (2008) Predicting grade of cerebral glioma using vascular-space occupancy MR imaging. AJNR Am J Neuroradiol 29:373–378
Chung C, Metser U, Menard C (2015) Advances in magnetic resonance imaging and positron emission tomography imaging for grading and molecular characterization of glioma. Semin Radiat Oncol 25:164–171
Bulik M, Jancalek R, Vanicek J, Skoch A, Mechl M (2013) Potential of MR spectroscopy for assessment of glioma grading. Clin Neurol Neurosurg 115:146–153
Herminghaus S, Dierks T, Pilatus U et al (2003) Determination of histopathological tumor grade in neuroepithelial brain tumors by using spectral pattern analysis of in vivo spectroscopic data. J Neurosurg 98:74–81
Dhermain FG, Hau P, Lanfermann H, Jacobs AH, van den Bent MJ (2010) Advanced MRI and PET imaging for assessment of treatment response in patients with gliomas. Lancet Neurol 9:906–920
Zhang H, Ma L, Wang Q, Zheng X, Wu C, Xu BN (2014) Role of magnetic resonance spectroscopy for the differentiation of recurrent glioma from radiation necrosis: a systematic review and meta-analysis. Eur J Radiol 83:2181–2189
Hollingworth W, Medina LS, Lenkinski RE et al (2006) A systematic literature review of magnetic resonance spectroscopy for the characterization of brain tumors. AJNR Am J Neuroradiol 27:1404–1411
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Deville WL, Buntinx F, Bouter LM et al (2002) Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol 2:9
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM (2008) Systematic reviews of diagnostic test accuracy. Ann Intern Med 149:889–897
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ 326:219
Deeks JJ, Macaskill P, Irwig L (2005) The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 58:882–893
Fudaba H, Shimomura T, Abe T et al (2014) Comparison of multiple parameters obtained on 3T pulsed arterial spin-labeling, diffusion tensor imaging, and MRS and the Ki-67 labeling index in evaluating glioma grading. AJNR Am J Neuroradiol 35:2091–2098
Dunet V, Maeder P, Nicod-Lalonde M et al (2014) Combination of MRI and dynamic FET PET for initial glioma grading. Nuklearmedizin 53:155–161
Caulo M, Panara V, Tortora D et al (2014) Data-driven grading of brain gliomas: a multiparametric MR imaging study. Radiology 272:494–503
Darweesh AMN, Badawy ME, Hamesa M, Saber N (2014) Magnetic resonance spectroscopy and diffusion imaging in the evaluation of neoplastic brain lesions. Egypt J Radiol Nucl Med 45:485–493
Yoon JH, Kim JH, Kang WJ et al (2014) Grading of cerebral glioma with multiparametric MR imaging and 18F-FDG-PET: concordance and accuracy. Eur Radiol 24:380–389
Metwally LIA, El-Din SE, Abdelaziz O, Hamdy IM, Elsamman AK, Abdelalim AM (2014) Predicting grade of cerebral gliomas using Myo-inositol/Creatine ratio. Egypt J Radiol Nucl Med 45:211–217
Sahin N, Melhem ER, Wang S et al (2013) Advanced MR imaging techniques in the evaluation of nonenhancing gliomas: perfusion-weighted imaging compared with proton magnetic resonance spectroscopy and tumor grade. Neuroradiol J 26:531–541
Roy B, Gupta RK, Maudsley AA et al (2013) Utility of multiparametric 3-T MRI for glioma characterization. Neuroradiology 55:603–613
Rao PJ, Jyoti R, Mews PJ, Desmond P, Khurana VG (2013) Preoperative magnetic resonance spectroscopy improves diagnostic accuracy in a series of neurosurgical dilemmas. Br J Neurosurg 27:646–653
Chawalparit O, Sangruchi T, Witthiwej T et al (2013) Diagnostic performance of advanced MRI in differentiating high-grade from low-grade gliomas in a setting of routine service. J Med Assoc Thai 96:1365–1373
Aprile I, Torni C, Fiaschini P, Muti M (2012) High-Grade Cerebral Glioma Characterization: Usefulness of MR Spectroscopy and Perfusion Imaging Associated Evaluation. Neuroradiol J 25:57–66
Shokry A (2012) MRS of brain tumors: diagrammatic representations and diagnostic approach. Egypt J Radiol Nucl Med 43:603–612
Liu ZL, Zhou Q, Zeng QS, Li CF, Zhang K (2012) Noninvasive evaluation of cerebral glioma grade by using diffusion-weighted imaging-guided single-voxel proton magnetic resonance spectroscopy. J Int Med Res 40:76–84
Zou QG, Xu HB, Liu F, Guo W, Kong XC, Wu Y (2011) In the assessment of supratentorial glioma grade: the combined role of multivoxel proton MR spectroscopy and diffusion tensor imaging. Clin Radiol 66:953–960
Zeng Q, Liu H, Zhang K, Li C, Zhou G (2011) Noninvasive evaluation of cerebral glioma grade by using multivoxel 3D proton MR spectroscopy. Magn Reson Imaging 29:25–31
Widhalm G, Krssak M, Minchev G et al (2011) Value of 1H-magnetic resonance spectroscopy chemical shift imaging for detection of anaplastic foci in diffusely infiltrating gliomas with non-significant contrast-enhancement. J Neurol Neurosurg Psychiatry 82:512–520
Chernov MF, Ono Y, Muragaki Y et al (2008) Differentiation of high-grade and low-grade gliomas using pattern analysis of long-echo single-voxel proton magnetic resonance spectroscopy ((1)H-MRS). Neuroradiol J 21:338–349
Di CA, Scarabino T, Trojsi F et al (2008) Proton MR spectroscopy of cerebral gliomas at 3 T: spatial heterogeneity, and tumour grade and extent. Eur Radiol 18:1727–1735
Zonari P, Baraldi P, Crisi G (2007) Multimodal MRI in the characterization of glial neoplasms: the combined role of single-voxel MR spectroscopy, diffusion imaging and echo-planar perfusion imaging. Neuroradiology 49:795–803
Zhang K, Li C, Liu Y et al (2007) Evaluation of invasiveness of astrocytoma using 1H-magnetic resonance spectroscopy: correlation with expression of matrix metalloproteinase-2. Neuroradiology 49:913–919
Kim JH, Chang KH, Na DG et al (2006) 3T 1H-MR spectroscopy in grading of cerebral gliomas: comparison of short and intermediate echo time sequences. AJNR Am J Neuroradiol 27:1412–1418
Stadlbauer A, Gruber S, Nimsky C et al (2006) Preoperative grading of gliomas by using metabolite quantification with high-spatial-resolution proton MR spectroscopic imaging. Radiology 238:958–969
Jeun SS, Kim MC, Kim BS et al (2005) Assessment of malignancy in gliomas by 3T 1H MR spectroscopy. Clin Imaging 29:10–15
Magalhaes A, Godfrey W, Shen Y, Hu J, Smith W (2005) Proton magnetic resonance spectroscopy of brain tumors correlated with pathology. Acad Radiol 12:51–57
Chen CY, Lirng JF, Chan WP, Fang CL (2004) Proton magnetic resonance spectroscopy-guided biopsy for cerebral glial tumors. J Formos Med Assoc 103:448–458
Fountas KN, Kapsalaki EZ, Vogel RL, Fezoulidis I, Robinson JS, Gotsis ED (2004) Noninvasive histologic grading of solid astrocytomas using proton magnetic resonance spectroscopy. Stereotact Funct Neurosurg 82:90–97
Law M, Yang S, Wang H et al (2003) Glioma grading: sensitivity, specificity, and predictive values of perfusion MR imaging and proton MR spectroscopic imaging compared with conventional MR imaging. AJNR Am J Neuroradiol 24:1989–1998
Kumar A, Kaushik S, Tripathi RP, Kaur P, Khushu S (2003) Role of in vivo proton MR spectroscopy in the evaluation of adult brain lesions: our preliminary experience. Neurol India 51:474–478
Yang D, Korogi Y, Sugahara T et al (2002) Cerebral gliomas: prospective comparison of multivoxel 2D chemical-shift imaging proton MR spectroscopy, echoplanar perfusion and diffusion-weighted MRI. Neuroradiology 44:656–666
Furuya S, Naruse S, Ide M et al (1997) Evaluation of metabolic heterogeneity in brain tumors using 1H-chemical shift imaging method. NMR Biomed 10:25–30
Wang W, Hu Y, Lu P et al (2014) Evaluation of the diagnostic performance of magnetic resonance spectroscopy in brain tumors: a systematic review and meta-analysis. PLoS One 9, e112577
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56:1129–1135
Server A, Kulle B, Gadmar OB, Josefsen R, Kumar T, Nakstad PH (2011) Measurements of diagnostic examination performance using quantitative apparent diffusion coefficient and proton MR spectroscopic imaging in the preoperative evaluation of tumor grade in cerebral gliomas. Eur J Radiol 80:462–470
Chen J, Huang SL, Li T, Chen XL (2006) In vivo research in astrocytoma cell proliferation with 1H-magnetic resonance spectroscopy: correlation with histopathology and immunohistochemistry. Neuroradiology 48:312–318
Moller-Hartmann W, Herminghaus S, Krings T et al (2002) Clinical application of proton magnetic resonance spectroscopy in the diagnosis of intracranial mass lesions. Neuroradiology 44:371–381
Bertholdo D, Watcharakorn A, Castillo M (2013) Brain proton magnetic resonance spectroscopy: introduction and overview. Neuroimaging Clin N Am 23:359–380
Howe FA, Barton SJ, Cudlip SA et al (2003) Metabolic profiles of human brain tumors using quantitative in vivo 1H magnetic resonance spectroscopy. Magn Reson Med 49:223–232
Pamir MN, Ozduman K, Yildiz E, Sav A, Dincer A (2013) Intraoperative magnetic resonance spectroscopy for identification of residual tumor during low-grade glioma surgery: clinical article. J Neurosurg 118:1191–1198
Bradac O, Vrana J, Jiru F et al (2014) Recognition of anaplastic foci within low-grade gliomas using MR spectroscopy. Br J Neurosurg 28:631–636
Hattingen E, Raab P, Franz K et al (2008) Prognostic value of choline and creatine in WHO grade II gliomas. Neuroradiology 50:759–767
Acknowledgments
The scientific guarantor of this publication is Hui Zhang, PHD. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors (Hui Zhang) has significant statistical expertise. Neither institutional review board approval nor written informed consent were required, because of the nature of our study, which was a systemic review and meta-analysis. Methodology: Meta-analysis, performed at one institution.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Qun Wang, Hui Zhang and JiaShu Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, Q., Zhang, H., Zhang, J. et al. The diagnostic performance of magnetic resonance spectroscopy in differentiating high-from low-grade gliomas: A systematic review and meta-analysis. Eur Radiol 26, 2670–2684 (2016). https://doi.org/10.1007/s00330-015-4046-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4046-z