Abstract
Objectives
Phase-contrast CMR (PC-CMR) might provide a fast and robust non-invasive determination of left ventricular function in patients after ST-segment elevation myocardial infarction (STEMI).
Methods
Cine sequences in the left-ventricular (LV) short-axis and free-breathing, retrospectively gated PC-CMR were performed in 90 patients with first acute STEMI and 15 healthy volunteers. Inter- and intra-observer agreement was determined. The correlations of clinical variables (age, gender, ejection fraction, NT pro-brain natriuretic peptide [NT-proBNP] with cardiac index (CI) were calculated.
Results
For CI, there was a strong agreement of cine CMR with PC-CMR in healthy volunteers (r: 0.82, mean difference: -0.14 l/min/m2, error ± 23 %). Agreement was lower in STEMI patients (r: 0.61, mean difference: -0.17 l/min/m2, error ± 32 %). In STEMI patients, CI measured with PC-CMR showed lower intra-observer (1 % vs. 9 %) and similar inter-observer variability (9 % vs. 12 %) compared to cine CMR. CI was significantly correlated with age, ejection fraction and NT-proBNP values in STEMI patients.
Discussion
The agreement of PC-CMR and cine CMR for the determination of CI is lower in STEMI patients than in healthy volunteers. After acute STEMI, CI measured with PC-CMR decreases with age, LV ejection fraction and higher NT-proBNP.
Key Points
• Cine CMR and PC-CMR correlate well in healthy volunteers.
• Agreement is lower in STEMI patients.
• Cardiac Output should be measured with one method longitudinally.
• Cardiac output decreases with age after myocardial infarction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Cardiac index (CI) is the product of stroke volume (SV) and heart rate (HR), normalized by the body surface area. It reflects the ability of the heart to meet the oxygen demands (VO2) of the organism [1].
Cardiovascular magnetic resonance (CMR) has become an excellent imaging technique for global cardiac assessment in patients with ischemic heart disease. In a single examination, a broad range of information, such as myocardial morphology, as well as central hemodynamic parameters (e.g., cardiac index), can be obtained [2, 3]. The latter have been traditionally measured by volumetric cine CMR.
An emerging alternative method for the assessment of central hemodynamic parameters is velocity-encoded, phase-contrast (PC-) CMR [4–9]. PC-CMR has been shown to be more reproducible than cine CMR [10] and inter-institutional variance is much lower in PC-CMR compared to cine CMR [11]. Flow measurements can be obtained during free-breathing [12] within a short scan time (~5 minute) [8]. With the increasing availability and improvement of CMR, the use of PC-CMR is being recommended in more and more indications in different clinical settings [13–16]. Its use, however, may be hampered by technical limitations or the lack of proper and standardised post processing and data analysis [17, 18]. Furthermore, patient related factors like valve regurgitation or stenosis and turbulent flow may reduce the reproducibility of PC-CMR [19]. Moreover, modern accelerated cine CMR techniques also promise fast and robust volumetric data during free breathing [20–22].
In patients after acute ST-segment elevation myocardial infarction (STEMI), PC-CMR for the assessment of CI has not been investigated so far. Especially in these patients, it might provide clinically useful information within a short scan time. Furthermore, factors influencing cardiac output, as assessed by PC-CMR, have not been evaluated in these patients.
Therefore, the aims of the present study were (1) to validate a free-breathing PC-CMR method for the assessment of CI in healthy volunteers, and (2) to evaluate its performance compared to cine CMR in STEMI patients. Furthermore, (3) the association of CI with patient characteristics after acute STEMI is investigated.
Methods
Study population
Cine CMR and PC-CMR examinations were performed in 15 healthy volunteers. Furthermore, 90 STEMI patients admitted to the coronary care unit of the Medical University Innsbruck Hospital between May 2010 and March 2012 were included in this prospective observational study. Inclusion criterion was the diagnosis of STEMI according to the redefined ESC/ACC committee criteria [23] and successful reperfusion by primary percutaneous coronary intervention (p-PCI). Exclusion criteria were renal dysfunction with an estimated glomerular filtration rate (eGFR) < 30 ml/min/1.73 m2, Killip class > 2 and contraindications for CMR. For evaluation of methods agreement, as well as inter- and intra-observer agreement, the first 16 STEMI patients were selected. Measurements were evaluated by two independent and experienced observers, each of which who was unaware of the results obtained by the other observer.
In STEMI patients, blood samples for investigation of all laboratory markers were collected and measured as described previously [24–26]. Data on mitral regurgitation were collected by a retrospective database analysis. In 70 of 90 STEMI patients, transthoracic echocardiography was performed within the first week after STEMI.
All study participants were aged above 18 years and gave written informed consent before inclusion in the study. The study was approved by the local ethics committee.
CMR protocol and image evaluation
All scans were performed on a 1.5 Tesla Magnetom AVANTO-scanner (Siemens, Erlangen, Germany). A detailed description of the CMR protocol was published previously [24, 27]. Briefly, cine CMR images in short-axis (11 slices) were acquired using breath-hold, retrospective ECG-triggered trueFISP bright-blood sequences. Evaluation of images was performed using standard software (ARGUS, Siemens Erlangen, Germany).
Late enhancement (LE) CMR images were acquired by using an ECG-triggered phase-sensitive inversion recovery (PSIR) single shot TrueFISP sequence with consecutive short-axis slices, as described in detail previously [27–30].
To quantify blood flow of the ascending aorta, a free-breathing, velocity-encoded phase-contrast (PC) protocol with a spatial resolution of 1.3 × 1.3 × 8 mm was applied directly after the cine CMR protocol. Velocity encoding was set to 150 cm/s. Retrospective ECG-triggering with 128 phases per cardiac cycle was applied. Repetition time (TR) was 13.56 ms. The mean heart rate during PC-CMR measurements was 67 ± 6 beats per minute in volunteers and 70 ± 12 beats per minute (bpm) in STEMI patients, resulting in a mean reconstructed temporal resolution of 7.0 ms and 6.7 ms, respectively. Slices were set perpendicular to the ascending aorta at the level of the pulmonary artery to measure through-plane flow [7, 31, 32].
Evaluation was performed using standard software (ARGUS, Siemens Erlangen, Germany). Contours of the ascending aorta were drawn manually on all 128 slices, and flow [ml/s] throughout one cardiac cycle was measured using the velocity values of the corresponding velocity-encoded images. Left ventricular SV [ml] was defined as the forward blood flow in the ascending aorta over one cardiac cycle. Cardiac output (CO) [l/min] was determined by multiplying SV by heart rate (HR) [beats/minute]. Heart rate was determined from the mean RR interval of cine stacks and PC-CMR, respectively. Cardiac index (CI) [l/min/m2] was obtained by dividing CO by body surface area (BSA) [m2]. To calculate BSA the Du Bois formula was used [33].
Statistical analysis
For statistical analysis, the statistical software package SPSS Statistics 19.0.0 (IBM, Armonk, NY, USA) was used. Kolmogorov-Smirnov test was used to test for normal distribution (ND). All results for continuous variables are expressed as mean ± standard deviation (SD) if ND, or as medians with corresponding interquartile range (IQR) if not. A p value < 0.05 was considered to indicate statistical significance. To evaluate the agreement between cine CMR and PC-CMR, Pearson correlation as well as Bland-Altman analysis was used [34]. Bias was defined as the mean value of the differences between CMR methods and limits of agreement ± 2 SDs. Error expressed in percent was calculated as the ratio of two times the SD of the differences to the mean of both measurements [35]. For healthy volunteers, a difference in CI of 0.2 ml/min/m2 could be detected with a statistical power of 80 %. For STEMI patients, a difference of 0.1 ml/min/m2 could be detected with a statistical power of 80 %. For the assessment of the coefficient of variability, the standard deviation of differences between the techniques was divided by mean value of the two methods.
Results
Study population
The mean age of the volunteers was 25.8 ± 2.4 years. 10 (67 %) were female. All volunteers were free of known cardiovascular diseases. The mean age of the STEMI population (n = 90) was 58.7 ± 10.8 years (range 29 to 79 years); 12 participants (13 %) were female. All patients were successfully treated with p-PCI (median pain-to-balloon time: 240 minutes, IQR: 146–577). Detailed patient characteristics on admission are shown in Table 1. Clinical characteristics of the first 16 STEMI patients included and selected for assessment of inter- and intra-observer coefficients of variability were comparable to total STEMI population [age = 61.4 ± 11.9 years; two female (13 %)].
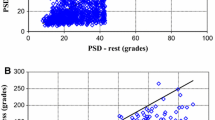
Healthy volunteers
There was a strong correlation of CI measured by cine CMR and PC-CMR in healthy volunteers (r: 0.83, p < 0.001). SVs determined by cine CMR and PC-CMR (r: 0.93, p < 0.001) and HR (r: 0.89, p < 0.001) during both examinations were also closely correlated. There was no statistical significant difference between CI or SV measured with cine CMR and PC-CMR (mean difference: -0.14 l/min/m2 and -1.1 ml, p = 0.07 and p = 0.48). Lower and upper limits of agreement were -0.68 l/min/m2 and 0.4 l/min/m2 for CI (error ± 23 %) and -12.8 ml and 10.6 ml for SV (error ± 18 %) (Fig. 1).
Agreement between cine CMR and PC-CMR
In STEMI patients, we observed a moderate correlation between the CI assessed by cine CMR and the CI assessed by PC-CMR (r = 0.61, p < 0.001). For the determination of SV, the two methods showed a strong association (r = 0.74, p < 0.001). The average CI determined by cine CMR was significantly higher compared to the average cardiac index measured by PC-CMR (2.9 ± 0.6 l/min/m2 vs. 2.7 ± 0.5 l/min/m2, p = 0.001, mean difference -0.17 l/min/m2). SV measured by cine CMR was 79.9 ± 18.4 ml and 78.2 ± 18.5 ml by PC-CMR (p = 0.22). The mean difference, or bias, was -0.17 l/min/m2 for CI and -1.7 ml for SV. Lower and upper limits of agreement were -1.1 l/min/m2 and 0.8 l/min/m2 for CI, as well as -28.3 ml and 24.8 ml for SV, respectively. The percentage error was 32 % for CI and 33 % for SV (Fig. 2).
Inter- and intra-observer variability
Inter-observer correlation coefficients for the assessment of cardiac index by PC-CMR were slightly higher compared to assessment by cine CMR (r = 0.91, p < 0.001 vs. r = 0.86, p < 0.001, respectively). Intra-observer correlation coefficients were significantly higher for PC-CMR ( r = 0.99, p < 0.001) than for cine CMR (r = 0.87, p < 0.001) (z-score: 3.349, p < 0.001). Moreover, for the measurement of cardiac index, PC-CMR showed lower intra-observer (1 % vs. 9 %) and similar inter-observer (9 % vs. 12 %) coefficients of variability compared to cine CMR.
Heart rate in STEMI patients
Heart rates at cine CMR and PC-CMR showed a strong linear correlation (r: 0.73, p < 0.001), but mean heart rate was higher during cine CMR than during PC-CMR (cine: 72 ± 12 bpm, PC-CMR: 70 ± 12, p = 0.02). In STEMI patients, the mean heart rate of both measurements correlated inversely with the mean SV (r: -0.55, p < 0.001) and positively with the mean CI (r: 0.25, p = 0.017). The differences in heart rate between both measurements were inversely correlated with the differences in SV (r: 0.42, p = 0.001) and positively correlated with the differences in CI (r: 0.37, p = 0.001). In the quartile of patients with a mean difference of more than -5 bpm between cine CMR and PC-CMR, the difference between both methods was significantly higher compared to the other patients (Fig. 3). The percentage error for CI and SV was similar in both groups (CI: 25 %, 32 % and 31 %; SV: 34 %, 32 % and 32 %).
Differences in cardiac index (A) and stroke volumes (B) between cine CMR and PC-CMR according to the change of heart rate between the protocols. If heart rate at the PC-CMR scan was more than 5 beats per minute lower than at the cine scan, the difference between both methods was significantly increased (* p < 0.05, ** p > 0.01)
Mitral regurgitation
In a subgroup of 70 STEMI patients (78 % of total study population), transthoracic echocardiography was performed within the first week after the index event. Mitral regurgitation was described in 42 (60 %) of the patients (Grade 1: n = 37, Grade 2: n = 4, Grade 3: n = 1 patients). The mean difference for CI (no mitral regurgitation: -0.11 ml/min/m2, with mitral regurgitation: -0.17 ml/min/m2, p = 0.62) or SVs (no mitral regurgitation: -0.56 ml, with mitral regurgitation: -0.94 ml, p = 0.91) did not differ significantly between patients with or without mitral regurgitation. The percentage error for CI and SV was similar in patients without (30 % and 37 %) or with mitral regurgitation (34 % and 30 %).
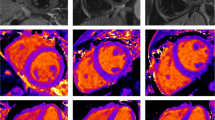
Factors associated with CI in STEMI patients
CMR data assessed by cine CMR and PC-CMR for all STEMI patients are summarized in Table 2. Study participants underwent CMR in median 2.9 days (IQR: 1.8–4.0) after the index event. PC-derived average CI was 2.7 ± 0.5 l/min/m2. Males (2.7 ± 0.5 l/min/m2) had a significantly higher CI compared to females (2.4 ± 0.3 l/min/m2). SV, but not HR, differed between males (SV: 80.4 ± 18.1 ml; HR: 70 ± 12 beats/min) and females (SV: 63.9 ± 14.1 ml, p = 0.003; HR: 67.1 ± 10.1 beats/min, p = 0.54). The lowest and highest CI measured in total population was 1.7 l/min/m2 and 4.2 l/min/m2, respectively.
CI decreased by 16 mL/min/m2 per year (r = -0.36, p = 0.001) (Fig. 4). Accordingly, age over 60 years was associated with lower CI in the two-way ANOVA analysis (p = 0.01). The decrease of CI with age was due to a decrease in SV (r = -0.23, p = 0.03) with age. HR was not associated with age (p > 0.05). In patients, mean left ventricular (LV) ejection fraction was 55 ± 11 %. CI was weakly associated with LV ejection fraction (r = 0.26, p < 0.02) and inversely correlated with NT-proBNP (r = -0.22, p < 0.05). CI was not associated with biomarkers of myocardial necrosis and infarct size (all p > 0.05).
Discussion
The main findings of the present study are that (1) free-breathing PC-CMR is a valid method for the assessment of CI in healthy volunteers, but (2) agreement with cine CMR is lower for the quantification of CI after acute STEMI. Furthermore we found, that (3) CI measured by PC-CMR is altered with age and gender, and is associated with LV ejection fraction and NT-proBNP in the acute phase after STEMI.
Agreement between cine CMR and PC-CMR
The measurement of hemodynamic parameters (e.g., CI) is an essential part of a comprehensive CMR examination. PC-CMR provides high accuracy and reproducibility for the assessment of aortic blood flow, and thus CI [4–8]. The choice of the method (cine vs. PC) and even the choice of the CMR protocol might influence results. Bolen et al. showed that agreement of aortic flow values between those obtained with breath-hold or non-breath-hold PC-CMR protocols is poor [12].
We found a strong linear correlation between the two methods in healthy volunteers, but a more moderate one in STEMI patients. In our study, the mean differences of CI and SV between cine CMR and PC-CMR were comparable to previous studies [12]. Average CI and SV were slightly higher with cine CMR compared to PC-CMR. One explanation might be that coronary flow, which is up to 5 % of the cardiac output [36], is included in SV as assessed by cine CMR, but not by PC-CMR.
In STEMI patients, Bland-Altman analysis revealed high limits of agreement between CIs as well as SVs determined by the two techniques. Two reasons might be responsible for this observation.
First, heart rate is significantly higher during cine CMR, most likely due to breath holds. This results in a decrease in SV [37] due to a decrease in diastolic filling time [38]. The increase in heart rate, however, increases CI. In our study, we observed a smaller bias in patients without an increase in heart rate < 5 bpm at cine CMR. However, the percentage error between the measurements did not improve.
It could be furthermore assumed that differences might be due to the presence of subclinical mitral regurgitation, which occurs in up to 50 % of STEMI patients [39]. This hypothesis, however, was not supported by a subgroup analysis of 70 STEMI patients. Mitral regurgitation was found in 60 % of patients, but the bias was not significantly related to the presence or absence of mitral regurgitation. The reason for this observation is most likely the low number of patients with grade 2 and 3 mitral regurgitation.
Critchley and Critchley propose a percentage error of < 30 % to indicate a good agreement between methods to determine CI [35]. In our study, the percentage error between cine CMR and PC-CMR is consistently above 30 %. These results indicate that cine CMR and PC-CMR findings are not interchangeable. Our findings suggest that for follow-up examinations for the measurement of hemodynamic parameters, the same CMR techniques should be used.
PC-CMR was proposed as the most accurate method for the in vivo measurement of cardiac output [40]. Interinstitutional variance was described as a potential source of variability in cine CMR, but not in PC-CMR [11]. We found that intra-observer variability was lower for PC-CMR compared to cine CMR, which is in line with previous studies comparing the two methods [10]. These results support the use of PC-CMR for the measurement of central hemodynamic parameters in patients after acute STEMI.
Factors influencing CI, assessed by PC-CMR, in patients after acute STEMI
CI may vary based on age, gender and ethnicity [1, 41–43]. Other studies, however, suggested that functional parameters might be independent of age [44, 45]. Hence, there is need for investigation of the possible impact of these parameters on CI for each population. In the present study, we describe for the first time the relation between CI and age as well as gender in patients post-STEMI.
CI index decreased gradually with age. The decrease of CI was driven by a slight decrease of stroke volume with age, whereas heart rate did not change significantly with age. This is in agreement with other studies reporting a significant, but slight, decline of left ventricular volumes with age [43, 46]. The magnitude of CI changes in patients after STEMI (16 mL/min/m2 per year) seems to be considerably higher than in healthy subjects (3.5 to 8 mL/min/m2 per year) [1, 41].
Myocardial dysfunction due to ischemic injury is likely to be responsible for this finding. However, CI was not related to the extent of myocardial damage in our study, which is in line with another study investigating hemodynamic patterns in the early phase after uncomplicated acute myocardial infarction by impedance cardiography [47].
There is conflicting evidence regarding the possible impact of gender on CI. Carlsson et al. did not find any gender differences in CI in healthy subjects and athletes. We observed a significantly higher CI in males compared to females. Most likely, the difference is attributed to the limited number of female patients and their older age. Therefore, the significance of this observation is limited. Further studies addressing possible gender differences in CI are necessary to finally clarify this issue.
In our STEMI cohort, mean CI was higher compared to those reported for patients with heart failure [1]. This observation might be explained by the inclusion of hemodynamically stable patients in our study. Even in STEMI patients without signs of heart failure, hemodynamic impairment is likely to occur [48]. Nevertheless, our results are limited to STEMI patients with a Killip Class ≤ 2.
Limitations
Eddy current correction was not applied in this study. Because of the integration of the measured flow velocities over the cardiac cycle, this might have significantly impacted our results [7]. After phantom correction, absolute flow values seem to increase in the ascending aorta [49]. The scanner system we used in this study is designed to compensate for induced fields. Furthermore, correction of phase offset errors with post processing is difficult near the heart because of the lack of stationary tissue in close vicinity of the vessel of interest [50]. As no eddy current correction was applied in healthy volunteers and STEMI patients, it is unlikely that the lack of correction has influenced our results. However, the effects of eddy current correction was beyond the scope of this study, so we cannot completely exclude an influence of phase offset errors. Further studies might be needed to answer this question.
Furthermore, no comparison between breath-hold and non–breath-hold PC-CMR has been performed in this study. Although prior studies have shown a poor agreement of breath-hold versus non–breath-hold PC-CMR [12] recent data suggest differences in RV but not in LV stroke volumes between different breath-hold techniques [51]. This might be different in STEMI patients and might therefore have altered our study results. Further studies on the effect of breath holding on LV stroke volumes and loading conditions in this specific cohort should be performed.
One reason for the differences in the agreement of cine-CMR and PC-CMR might be the larger STEMI cohort, compared to the validation group. This might result in a larger distribution of the differences in stroke volumes and cardiac index. Nevertheless, as, to the best of our knowledge, no studies on the use of PC-CMR derived stroke volumes are available yet, we were of the opinion that robust data should be based on a relatively large study cohort. Anyhow, the analysis of observer variability was performed in a small sub-study to ensure comparability with the data from the validation group.
Conclusion
In this study, we have shown that the agreement of PC-CMR and cine CMR for the determination of CI is lower in STEMI patients than in healthy volunteers. Reasons might be subclinical mitral regurgitation and changes in heart rates between both measurements. Therefore, follow-up examinations of STEMI patients should be performed with the same CMR technique.
After acute STEMI, CI measured with PC-CMR decreases gradually with age. The decrease is mainly explained by a decrease of SV with age. CI is further associated with LV ejection fraction and NT-proBNP in the acute phase after STEMI.
Abbreviations
- ACC:
-
American College of Cardiology
- BMI:
-
Body mass index
- Bpm:
-
Beat per minute
- BSA:
-
Body surface area
- CMR:
-
Cardiovascular magnetic resonance
- CI:
-
Cardiac index
- cTnT:
-
Cardiac Troponin T
- ECG:
-
Electrocardiogram
- eGFR:
-
Estimated glomerular filtration rate
- ESC:
-
European Society of Cardiology
- HR:
-
Heart rate
- IQR:
-
Interquartile range
- LE:
-
Late enhancement
- EF:
-
Ejection fraction
- NT-proBNP:
-
N-terminal pro-B-type natriuretic peptide
- NYHA:
-
New York Heart Association
- PC:
-
Phase-contrast
- PSIR:
-
Phase-sensitive inversion recovery
- p-PCI:
-
Primary percutaneous coronary intervention
- SD:
-
Standard deviation
- STEMI:
-
ST-segment elevation myocardial infarction
- SV:
-
Stroke volume
References
Carlsson M, Andersson R, Bloch KM et al (2012) Cardiac output and cardiac index measured with cardiovascular magnetic resonance in healthy subjects, elite athletes and patients with congestive heart failure. J Cardiovasc Magn Reson 14:51
Klug G, Metzler B (2013) Assessing myocardial recovery following ST-segment elevation myocardial infarction: short- and long-term perspectives using cardiovascular magnetic resonance. Expet Rev Cardiovasc Ther 11:203–219
Wong DT, Leong DP, Weightman MJ et al (2014) Magnetic resonance-derived circumferential strain provides a superior and incremental assessment of improvement in contractile function in patients early after ST-segment elevation myocardial infarction. Eur Radiol 24:1219–1228
Lee VS, Spritzer CE, Carroll BA et al (1997) Flow quantification using fast cine phase-contrast MR imaging, conventional cine phase-contrast MR imaging, and Doppler sonography: in vitro and in vivo validation. AJR Am J Roentgenol 169:1125–1131
Lew CD, Alley MT, Bammer R et al (2007) Peak velocity and flow quantification validation for sensitivity-encoded phase-contrast MR imaging. Acad Radiol 14:258–269
Beerbaum P, Korperich H, Gieseke J et al (2005) Blood flow quantification in adults by phase-contrast MRI combined with SENSE--a validation study. J Cardiovasc Magn Reson 7:361–369
Lotz J, Meier C, Leppert A et al (2002) Cardiovascular flow measurement with phase-contrast MR imaging: basic facts and implementation. Radiographics 22:651–671
Hundley WG, Li HF, Hillis LD et al (1995) Quantitation of cardiac output with velocity-encoded, phase-difference magnetic resonance imaging. Am J Cardiol 75:1250–1255
Traber J, Wurche L, Dieringer MA et al. (2015) Real-time phase contrast magnetic resonance imaging for assessment of haemodynamics: from phantom to patients. Eur Radiol. doi:10.1007/s00330-015-3897-7
Rominger MB, Dinkel HP, Bachmann GF (2002) Comparison between fast MR flow quantification in breathhold technique in ascending aorta and pulmonary trunc with right and left ventricular cine-MRI for the assessment of stroke volumes in healthy volunteers. RoFo 174:196–201
Beerbaum P, Barth P, Kropf S et al (2009) Cardiac function by MRI in congenital heart disease: impact of consensus training on interinstitutional variance. J Magn Reson Imaging 30:956–966
Bolen MA, Setser RM, Gabriel RS et al (2013) Effect of protocol choice on phase contrast cardiac magnetic resonance flow measurement in the ascending aorta: breath-hold and non-breath-hold. Int J Card Imaging 29:113–120
Prowle JR, Molan MP, Hornsey E et al (2012) Measurement of renal blood flow by phase-contrast magnetic resonance imaging during septic acute kidney injury: a pilot investigation. Crit Care Med 40:1768–1776
Nogami M, Ohno Y, Koyama H et al (2009) Utility of phase contrast MR imaging for assessment of pulmonary flow and pressure estimation in patients with pulmonary hypertension: comparison with right heart catheterization and echocardiography. J Magn Reson Imaging 30:973–980
Steeden JA, Atkinson D, Hansen MS et al (2011) Rapid flow assessment of congenital heart disease with high-spatiotemporal-resolution gated spiral phase-contrast MR imaging. Radiology 260:79–87
Kramer CM, Barkhausen J, Flamm SD et al (2008) Standardized cardiovascular magnetic resonance imaging (CMR) protocols, society for cardiovascular magnetic resonance: board of trustees task force on standardized protocols. J Cardiovasc Magn Reson 10:35
Gatehouse PD, Rolf MP, Graves MJ et al (2010) Flow measurement by cardiovascular magnetic resonance: a multi-centre multi-vendor study of background phase offset errors that can compromise the accuracy of derived regurgitant or shunt flow measurements. J Cardiovasc Magn Reson 12:5
Giese D, Haeberlin M, Barmet C et al (2012) Analysis and correction of background velocity offsets in phase-contrast flow measurements using magnetic field monitoring. Magn Reson Med 67:1294–1302
Kilner PJ, Gatehouse PD, Firmin DN (2007) Flow measurement by magnetic resonance: a unique asset worth optimising. J Cardiovasc Magn Reson 9:723–728
Setser RM, Fischer SE, Lorenz CH (2000) Quantification of left ventricular function with magnetic resonance images acquired in real time. J Magn Reson Imaging 12:430–438
Feng L, Srichai MB, Lim RP et al (2013) Highly accelerated real-time cardiac cine MRI using k-t SPARSE-SENSE. Magn Reson Med 70:64–74
Vincenti G, Monney P, Chaptinel J et al (2014) Compressed sensing single-breath-hold CMR for fast quantification of LV function, volumes, and mass. JACC Cardiovasc Imaging 7:882–892
Alpert JS, Thygesen K, Antman E et al (2000) Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36:959–969
Mayr A, Mair J, Schocke M et al (2011) Predictive value of NT-pro BNP after acute myocardial infarction: relation with acute and chronic infarct size and myocardial function. Int J Cardiol 147:118–123
Mayr A, Klug G, Schocke M et al (2012) Late microvascular obstruction after acute myocardial infarction: relation with cardiac and inflammatory markers. Int J Cardiol 157:391–396
Reinstadler SJ, Klug G, Feistritzer HJ et al (2013) Association of copeptin with myocardial infarct size and myocardial function after ST segment elevation myocardial infarction. Heart 99:1525–1529
Klug G, Trieb T, Schocke M et al (2009) Quantification of regional functional improvement of infarcted myocardium after primary PTCA by contrast-enhanced magnetic resonance imaging. J Magn Reson Imaging 29:298–304
Beek AM, Kuhl HP, Bondarenko O et al (2003) Delayed contrast-enhanced magnetic resonance imaging for the prediction of regional functional improvement after acute myocardial infarction. J Am Coll Cardiol 42:895–901
Bondarenko O, Beek AM, Hofman MB et al (2005) Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson 7:481–485
Nowosielski M, Schocke M, Mayr A et al (2009) Comparison of wall thickening and ejection fraction by cardiovascular magnetic resonance and echocardiography in acute myocardial infarction. J Cardiovasc Magn Reson 11:22
Herold V, Parczyk M, Morchel P et al (2009) In vivo measurement of local aortic pulse-wave velocity in mice with MR microscopy at 17.6 Tesla. Magn Reson Med 61:1293–1299
Klug G, Feistritzer HJ, Reinstadler SJ et al. (2014) Association of aortic stiffness with biomarkers of myocardial wall stress after myocardial infarction. Int J Card 173:253–8
Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 5:303–311, discussion 12-3
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15:85–91
Chernobelsky A, Shubayev O, Comeau CR et al (2007) Baseline correction of phase contrast images improves quantification of blood flow in the great vessels. J Cardiovasc Magn Reson 9:681–685
Reil JC, Tardif JC, Ford I et al (2013) Selective heart rate reduction with ivabradine unloads the left ventricle in heart failure patients. J Am Coll Cardiol 62:1977–1985
Opdahl A, Ambale Venkatesh B, Fernandes VR et al (2014) Resting heart rate as predictor for left ventricular dysfunction and heart failure: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 63:1182–1189
Bursi F, Enriquez-Sarano M, Nkomo VT et al (2005) Heart failure and death after myocardial infarction in the community: the emerging role of mitral regurgitation. Circulation 111:295–301
Gatehouse PD, Keegan J, Crowe LA et al (2005) Applications of phase-contrast flow and velocity imaging in cardiovascular MRI. Eur Radiol 15:2172–2184
Slotwiner DJ, Devereux RB, Schwartz JE et al (1998) Relation of age to left ventricular function in clinically normal adults. Am J Cardiol 82:621–626
Kuikka JT, Lansimies E (1982) Effect of age on cardiac index, stroke index and left ventricular ejection fraction at rest and during exercise as studied by radiocardiography. Acta Physiol Scand 114:339–343
Chang SA, Choe YH, Jang SY et al (2012) Assessment of left and right ventricular parameters in healthy Korean volunteers using cardiac magnetic resonance imaging: change in ventricular volume and function based on age, gender and body surface area. Int J Card Imaging 28(Suppl 2):141–147
Slotwiner DJ, Devereux RB, Schwartz JE et al (2001) Relation of age to left ventricular function and systemic hemodynamics in uncomplicated mild hypertension. Hypertension 37:1404–1409
Sandstede J, Lipke C, Beer M et al (2000) Age- and gender-specific differences in left and right ventricular cardiac function and mass determined by cine magnetic resonance imaging. Eur Radiol 10:438–442
Cain PA, Ahl R, Hedstrom E et al (2009) Age and gender specific normal values of left ventricular mass, volume and function for gradient echo magnetic resonance imaging: a cross sectional study. BMC Med Imaging 9:2
Zimlichman R, Mossinson D, Ovsyshcher IE (1989) Assessment of hemodynamic changes in the early phase of uncomplicated acute myocardial infarction. Int J Cardiol 25:303–311
Bergstra A, Svilaas T, van Veldhuisen DJ et al (2007) Haemodynamic patterns in ST-elevation myocardial infarction: incidence and correlates of elevated filling pressures. Neth Heart J 15:95–99
Holland BJ, Printz BF, Lai WW (2010) Baseline correction of phase-contrast images in congenital cardiovascular magnetic resonance. J Cardiovasc Magn Reson 12:11
Pelc NJ, Herfkens RJ, Shimakawa A et al (1991) Phase contrast cine magnetic resonance imaging. Magn Reson Q 7:229–254
Claessen G, Claus P, Delcroix M et al (2014) Interaction between respiration and right versus left ventricular volumes at rest and during exercise: a real-time cardiac magnetic resonance study. Am J Physiol Heart Circ Physiol 306:H816–H824
Acknowledgments
The scientific guarantor of this publication is Bernhard Metzler. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by the Austria Society for Cardiology, Innsbruck Medical University and the Hans und Blanca Moser Stiftung.
One of the authors has significant statistical expertise. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Written informed consent was waived by the Institutional Review Board. Some study subjects or cohorts have been previously reported in MRI, IJC. All patients have been studied within the MARINA-STEMI registry at the Medical University of Innsbruck. Phase contrast data has not been previously published. Methodology: prospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klug, G., Reinstadler, S.J., Feistritzer, HJ. et al. Cardiac index after acute ST-segment elevation myocardial infarction measured with phase-contrast cardiac magnetic resonance imaging. Eur Radiol 26, 1999–2008 (2016). https://doi.org/10.1007/s00330-015-4022-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4022-7