Abstract
Objectives
To investigate follow-up after percutaneous pulmonary valve implantation (PPVI).
Methods
Forty patients with pulmonary conduit dysfunction (males/females 24/16; 21 ± 08 years; 12 tetralogy of Fallot, 11 aortic valve disease, 17 other congenital heart disease) were planned for CMR before PPVI and repeated 7 times up to 48 months. CMR prospective results regarded: pressure gradient (PG) and regurgitation fraction (RF); end-diastolic volume, end-systolic volume, and stroke volume indexed to body surface area (EDVI, ESVI, and SVI); ejection fraction (EF) of right and left ventricles (RV, LV). A Friedman test was used for comparisons.
Results
Overall, PG (31 ± 06 to 16 ± 4 mmHg), RF (16 ± 17 to 0.3 ± 1 %), RVEDVI (82 ± 38 to 58 ± 12 ml/m2), and RVESVI (44 ± 12 to 30 ± 13 ml/m2) declined (p < 0.001), RVEF (49 ± 13 to 58 ± 12 %) and RVSVI (from 38 ± 14 to 40 ± 8 ml/m2) increased (p < 0.001), LVEDVI (67 ± 17 to 73 ± 18 ml/m2) and LVSVI (37 ± 11 to 43 ± 10 ml/m2) increased (p = 0.034 and p < 0.001). Two patients had valve fracture at 24 and 36 months and underwent surgery. One patient had stent restenosis at 24 months and underwent percutaneous retreatment. Baseline/follow-up CMR did not predict PPVI failure.
Conclusions
CMR demonstrated restored pulmonary conduit function, reduced RV volumes and increased RV and LV function but did not predict valve fracture/restenosis.
Key points
• A CMR 4-year follow-up after PPVI showed restored pulmonary conduit function
• RV volumes were significantly reduced
• RV function was significantly better in terms of increased EF and SVI
• LV function was significantly better in terms of increased EDVI and SVI
• Baseline/follow-up CMR did not predict three cases of PPVI failure
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous pulmonary valve implantation (PPVI) is a nonsurgical option for treating right ventricular (RV) outflow tract and/or pulmonary trunk dysfunction, representing one of the most exciting approaches of interventional cardiology as the first in-human application of this technique [1]. In particular, Bonhoeffer et. al. [2] developed a new approach to treat RV conduit dysfunction using a bovine valve sutured on a platinum-iridium alloy stent, with welded joints of gold (Melody, Medtronic, Inc., Minneapolis, MN, US) [2].
Being less invasive than surgical pulmonary valve replacement, PPVI avoids the risks of ventriculotomy and cardiopulmonary bypass as well as the risks of bleeding and infections associated with reoperation, avoiding postoperative intensive care reduces costs. The procedure would have to provide feasibility and safety comparable to those of surgical procedures, which are burdened by conduit failures and require multiple re-interventions [3]. The most common indications for surgical pulmonary valve replacement are pulmonary regurgitation with or without stenosis, RV dilation and hemodynamically significant residual lesions [1].
The majority of patients referred for surgical pulmonary valve replacement or PPVI have a diagnosis of tetralogy of Fallot with pulmonary stenosis or pulmonary atresia or a previous surgical treatment for critical pulmonary valve stenosis [4–6]. In these patients, after repairing, the chronic RV volume overload leads to ventricular dilation and impairment of systolic and diastolic function. In the long term, this causes atrial and ventricular arrhythmia as well as heart failure and increases the risk of sudden death [7]. Restoration of pulmonary valve competence at an appropriate time has resulted in improvement in RV function and effort tolerance and reduces the incidence of arrhythmias [8, 9]. Thus, patient selection and correct timing for PPVI plays a key role in the success of this technique.
Follow-up after PPVI may be performed using echocardiography as a first-line technique [10]. This modality is relatively inexpensive, widely available, and is not associated with ionizing radiation exposure. However, its limitations include poor acoustic windows in assessing RV morphology, function and valve regurgitation [11]. In recent years, studies have been reporting the use of cardiac magnetic resonance (CMR) to evaluate patients before and after PPVI [12–14]. CMR has been demonstrated to outperform echocardiography in the evaluation of cardiac chambers, especially the RV, and it is considered as a first-choice technique in this setting [15–17].
Our aim was to report the 4-year CMR follow-up of patients treated with PPVI.
Materials and methods
Study design and population
After institutional review board approval waived specific patient consent for data analysis, we retrospectively retrieved prospective reports of CMR examinations performed before and after PPVI from January 2008 to June 2014 in 40 consecutive patients treated with a Melody valve stent (Medtronic, Inc., Minneapolis, MN, US). Demographics, age, and disease spectrum are shown in Table 1. CMR had been planned at least 1 month before PPVI, and 1, 3, 6, 12, 24, 36, and 48 months after PPVI. Paediatric cardiologists obtained informed consent for the intervention and use of this type of valve for PPVI. Informed consent was obtained by each patient for the injection of gadolinium (Gd)-based contrast material, when administered.
CMR protocol
We used a 1.5-T unit with 40-mT/m gradient power (Magnetom Sonata Maestro Class, Siemens, Erlangen, Germany) and a four-channel cardio-thoracic phased-array coil. The same imaging protocol was used before and after PPVI. The mean CMR duration was 45 ± 10 min.
Electrocardiographically-triggered short-axis, four-chamber and long-axis images were obtained with a breath-hold steady-state free precession (SSFP) sequence (true fast imaging with SSFP, true-FISP) acquired with the following technical parameters: TR/TE, 4.0/1.5 ms; FA, 80°; slice thickness, 8 mm; temporal resolution, 45 ms; mean acquisition time, 14 ± 4 s. A breath-hold turbo spoiled gradient echo sequence (fast low-angle shot, FLASH) was performed for phase-velocity mapping of pulmonary flow with the following technical parameters: TR/TE, 4.0/3.2 ms; slice thickness, 5 mm; velocity encoding (VENC) from 150 to 350 ms; temporal resolution, 41 ms; mean acquisition time, 15 ± 4 s. Firstly we acquired the phase-contrast sequence with a VENC of 150 ms; in the presence of aliasing, we modified the VENC adding 50 ms for each new sequence, step-by-step up to the complete disappearance of the aliasing artefact.
Before PPVI, the slice of the phase-contrast sequence was located on the pulmonary conduit, perpendicular to the vessel long axis, immediately distal to the valve; after PPVI, the slice was located at least 4 mm distal to the stent artefact to avoid contamination of images from the metallic artefact. Mr angiography with a three-dimensional gradient-echo fast low-angle shot sequence (FLASH, TR = 3.32 ms, TE = 1.21 ms, flip angle 25°, slice thickness = 1.5 mm, 72 partitions, acquisition time 21 s) after injection of 0.1 mmol/kg of gadobenate dimeglumine (MultiHance, Bracco Imaging SpA, Milan, Italy) was performed only at the baseline CMR before PPVI [18]. MR angiography was not performed after PPVI due to the presence of the metal artefact in the pulmonary conduit.
Image analysis
Cine true-FISP images in the short-axis plane, from heart base to apex, were segmented semiautomatically (Syngo-Argus, version VE32B, Siemens Medical Solutions, Erlangen, Germany) by a reader with 7 years of experience in CMR imaging, to obtain end-diastolic volume (EDV), normalized to body surface area (EDV index, EDVI), end-systolic volume index (ESVI), stroke volume (SVI), and ejection fraction (EF) of the RV and left ventricle (LV) [19]. In Fig. 1 is shown an example of RV segmentation. Papillary muscles were excluded from the volume. The basis was chosen with the references of a four-chamber view [20].
Reverse flow, forward flow and peak velocity data of the pulmonary valve were obtained by segmenting phase contrast images with the same software. We estimated pulmonary regurgitation fraction (RF) by flow data [21]. The pressure gradient (PG) was estimated from peak flow velocities using Bernoulli’s equation as described [22].
Statistical analysis
A Friedman test was used to compare EDVI, ESVI, SVI, EF, RF and PG before and after 1, 3, 6, 12, 24, 36, and 48 months from PPVI. All testing was performed using SPSS statistical software for Windows, release 14.0 (SPSS Inc., Chicago, IL, US). P values lower than 0.05 were considered statistically significant.
Results
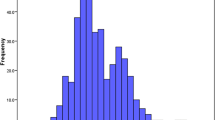
Overall results of CMR before and during the follow-up after PPVI are shown in Table 2. Overall, PG (31 ± 06 to 16 ± 4 mmHg) and RF (16 ± 17 to 0.3 ± 1 %) declined significantly (p < 0.001). A significant reduction of RV volumes (EDVI from 82 ± 38 to 58 ± 12 ml/m2, p < 0.001; ESVI from 44 ± 12 to 30 ± 13 ml/m2, p < 0.001), as well as a significant increase of RVEF (from 49 ± 13 to 58 ± 12 %, p < 0.001) and SVI (from 38 ± 14 to 40 ± 8 ml/m2, p < 0.001) were observed; RF and PG were significantly reduced at the last follow-up (p < 0.001). LV analysis showed a significant increase in EDVI (from 67 ± 17 to 73 ± 18 ml/m2, p = 0.034) and SVI (from 37 ± 11 to 43 ± 10 ml/m2, p < 0.001) while no significant changes were observed for ESVI and EF. In Fig. 2, RV and LV volumes, EF, RF and PG are represented during the follow-up as plotted versus time. In Figs. 3 and 4, CMR images before PPVI and during the follow-up are shown.
Graphs showing ventricle volumes, ejection fraction, regurgitation fraction and pressure gradient as plotted versus time. PPVI: percutaneous pulmonary valve replacement. RV: right ventricle. LV: left ventricle. EDVI: end-diastolic volume index. ESVI: end-systolic volume index. SVI: stroke volume index. EF: ejection fraction. RF: regurgitation fraction. PG: pressure gradient
CMR images of a 14-year-old patient with congenital pulmonary atresia treated with a homograft. Due to homograft stenosis, a percutaneous pulmonary valve (PPVI) was implanted. In the figure are shown images of cine true-FISP sequences at the end-diastolic phase. Right ventricle outflow tract (a, b) and three short axis planes (c, d, e, f, g and h) from the basal portion of the heart to the apex before (upper line) and after 48 months from PPVI (lower line) are shown. Note the artefact of pulmonary valve stent after PPVI in b and the reduction of the right ventricle end-diastolic volume (from 80 ml/m2 to 55 ml/m2) and septal flattening. Septal flattening is visible on c and e. Reduction of the volume abd of septal flattenig is evident when comparing images e and f
CMR of a 24-year-old patient with tetralogy of Fallot treated with a homograft. Due to homograft stenosis, a percutaneous pulmonary valve was implanted (PPVI). Cine true-FISP images at the end-diastolic phase of the right ventricle outflow tract before (a) and after PPVI (b) are shown. Reference lines (white lines) of phase-contrast sequences before (a) and after PPVI (b) are also shown
One patient performed CMR with an intracardiac defibrillator with the housing implanted on the right anterior side of the chest (Fig. 5). Before CMR examinations, a dedicated cardiologist deactivated the device to avoid a wrong response during the examination.
CMR of a 31-year-old patient with tetralogy of Fallot with an implantable cardiac defibrillator (ICD), previously treated with a homograft. Cine FLASH sequences at the end-diastolic phase of the right ventricle outflow tract before (a) and after PPVI (b) are shown. Note the artefact created by the catheter in the right ventricle and that created by the pulmonary valve stent after PPVI. The ICD in the right position of the chest allowed for a diagnostic CMR without artefacts impairing heart evaluation
Two patients needed a surgical conduit replacement 24 and 36 months after the PPVI due to a fracture of the pulmonary stents. One patient needed a second implantation of a stent in the pulmonary conduit after 24 months of PPVI due to a restenosis of the valve. Patient characteristics as well as baseline and follow-up CMR results of these three patients up to the adverse event are shown in Table 3. We did not find any signs or parameters of CMR that could predict the adverse events.
Discussion
In the last decade, PPVI has emerged as the preferred treatment in pulmonary conduit dysfunction in CHD patients, being less invasive than surgical repair. We investigate with CMR a consecutive series of patients before and after PPVI to evaluate the immediate and mid-term changes in cardiac function values.
We observed a significant and progressive reduction of RV volumes as well as a significant increase of RVEF and RVSVI during the investigated follow-up. The most important remodelling occurred 3 months after the PPVI. However, it was important to show what happened during the following four years, when a further progressive remodelling was observed with a continuous increase of RVEF. Regarding flow analysis, both RF and PG were strongly and immediately reduced (at 1 month follow-up) and were thereafter stable at lowered values. These results were in agreement with the literature [12–14, 16], showing a good effect of PPVI on the RV function. However, to our knowledge, there are no studies showing the follow-up of these patients up to 4 years after PPVI.
Interestingly, follow-up of LV volumes showed a significant increase in EDVI and SVI. The former result can be explained considering that the reduction of RVEDVI allows a better diastolic compliance of LV, in turn determining an increased LVSVI. The improvement of LVEDVI likely reflects a decrease in RV volume and pressure overload, and hence a reduction in interventricular dependence from paradoxical septal motion. Conversely, the LVEF remained unchanged due to the insignificant increase in LVESVI.
Of note, one patient with an implantable cardiac defibrillator was fully studied with CMR with a comprehensive evaluation of RV and RV outflow tract function. The reason for this good result is that the housing of the device was implanted on the right side of the chest, causing artefacts to not influence heart imaging. This CMR was performed because the patient had been enrolled in an IRB-approved prospective study aimed at evaluating the MR safety in patients having pacemakers or implantable cardiac defibrillators.
PPVI implies some possible complications as stent fracture [23] or stent restenosis [23, 24]. In our population, two patients had stent fracture and one had stent restenosis. In the two cases of stent fracture, a surgical implantation of a conduit was performed; in the case of restenosis, a new stent was implanted. We did not find any CMR sign or parameter that could predict the adverse events, the baseline and follow-up results (see Table 3) not being different from those patients who did not have any adverse events. Thus, while endocarditis is the most probable cause of restenosis, the only possible explanation for the fracture is a suboptimal correspondence between the stent geometry and the individual outflow tract anatomy.
This study had some limitations. First, we retrospectively evaluated a heterogeneous sample of patients with congenital heart diseases originally treated with different surgical procedures. However, the series of patients was consecutive and all patients presented the same condition of pulmonary stenosis/insufficiency treated with PPVI. Second, we did not estimate the inter- and intra-observer reproducibility of CMR data. However, CMR is widely considered more reproducible than echocardiography in the evaluation of the right chambers and pulmonary artery in a multiplanar and comprehensive evaluation [15, 21]. Finally, only one type of pulmonary valve stent was involved, as described in the Methods section, so that our conclusion cannot be applied to other pulmonary valve stents.
In conclusion, a CMR four-year follow-up after PPVI demonstrated restored pulmonary conduit function, reduced RV volumes and increased RV and LV function. However, it did not predict valve fracture/restenosis.
References
Khambadkone S, Bonhoeffer P (2004) Nonsurgical pulmonary valve replacement: why, when, and how? Catheter Cardiovasc Interv 62:401–408
Bonhoeffer P, Boudjemline Y, Saliba Z et al (2000) Percutaneous replacement of pulmonary valve in a right-ventricle to pulmonary-artery prosthetic conduit with valve dysfunction. Lancet 356:1403–1405
Stark J (1998) The use of valved conduits in pediatric cardiac surgery. Pediatr Cardiol 19:282–288
Lurz P, Bonhoeffer P, Taylor AM (2009) Percutaneous pulmonary valve implantation: an update. Expert Rev Cardiovasc Ther 7:823–833
Eyskens B, Reybrouck T, Bogaert J et al (2000) Homograft insertion for pulmonary regurgitation after repair of tetralogy of fallot improves cardiorespiratory exercise performance. Am J Cardiol 85:221–225
Kanter KR, Budde JM, Parks WJ et al (2002) One hundred pulmonary valve replacements in children after relief of right ventricular outflow tract obstruction. Ann Thorac Surg 73:1801–1806
Gatzoulis MA, Elliott JT, Guru V et al (2000) Right and left ventricular systolic function late after repair of tetralogy of Fallot. Am J Cardiol 86:1352–1357
Conte S, Jashari R, Eyskens B et al (1999) Homograft valve insertion for pulmonary regurgitation late after valveless repair of right ventricular outflow tract obstruction. Eur J Cardiothorac Surg 15:143–149
Therrien J, Siu SC, Harris L et al (2001) Impact of pulmonary valve replacement on arrhythmia propensity late after repair of tetralogy of Fallot. Circulation 103:2489–2494
Li W, Davlouros PA, Kilner PJ et al (2004) Doppler-echocardiographic assessment of pulmonary regurgitation in adults with repaired tetralogy of Fallot: comparison with cardiovascular magnetic resonance imaging. Am Heart J 147:165–172
Valente AM, Cook S, Festa P et al (2014) Multimodality imaging guidelines for patients with repaired tetralogy of fallot: a report from the american society of echocardiography: developed in collaboration with the society for cardiovascular magnetic resonance and the society for pediatric radiology. J Am Soc Echocardiogr 27:111–141
McElhinney DB, Hellenbrand WE, Zahn EM et al (2010) Short- and medium-term outcomes after transcatheter pulmonary valve placement in the expanded multicenter US melody valve trial. Circulation 122:507–516
Eicken A, Ewert P, Hager A et al (2011) Percutaneous pulmonary valve implantation: two-centre experience with more than 100 patients. Eur Heart J 32:1260–1265
Lurz P, Nordmeyer J, Giardini A et al (2011) Early versus late functional outcome after successful percutaneous pulmonary valve implantation: are the acute effects of altered right ventricular loading all we can expect? J Am Coll Cardiol 57:724–731
Hendel RC, Patel MR, Kramer CM et al (2006) ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol 48:1475–1497
Secchi F, Resta EC, Piazza L et al (2014) Cardiac magnetic resonance before and after percutaneous pulmonary valve implantation. Radiol Med 119:400–407
Secchi F, Di Leo G, Papini GD et al (2011) Cardiac magnetic resonance: impact on diagnosis and management of patients with congenital cardiovascular disease. Clin Radiol 66:720–725
Vogt FM, Theysohn JM, Michna D et al (2013) Contrast-enhanced time-resolved 4D MRA of congenital heart and vessel anomalies: image quality and diagnostic value compared with 3D MRA. Eur Radiol 23:2392–2404
Van Dijck I, Budts W, Cools B et al (2014) Infective endocarditis of a transcatheter pulmonary valve in comparison with surgical implants. Heart 0:1–6
Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E (2013) Society for Cardiovascular Magnetic Resonance Board of Trustees Task Force on Standardized Protocols. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson 15:91
Caudron J, Fares J, Lefebvre V, Vivier PH, Petitjean C, Dacher JN (2012) Cardiac MRI, assessment of right ventricular function in acquired heart disease: factors of variability. Acad Radiol 19(8):991–1002
Kilner PJ, Gatehouse PD, Firmin DN (2007) Flow measurement by magnetic resonance: a unique asset worth optimising. J Cardiovasc Magn Reson 9:723–728
Secchi F, Iozzelli A, Papini GD et al (2009) MR imaging of aortic coarctation. Radiol Med 114:524–537
Butera G, Milanesi O, Spadoni I et al (2013) Melody transcatheter pulmonary valve implantation. Results from the registry of the Italian Society of Pediatric Cardiology. Catheter Cardiovasc Interv 81:310–316
Acknowledgments
The scientific guarantor of this publication is Professor Francesco Sardanelli. M Carminati is consultant/proctor for Medtronic and Edwards; F. Sardanelli has received research grants from and is a member of the speakers’ bureau for Bracco Imaging. The remaining authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Secchi, F., Resta, E.C., Cannaò, P.M. et al. Four-year cardiac magnetic resonance (CMR) follow-up of patients treated with percutaneous pulmonary valve stent implantation. Eur Radiol 25, 3606–3613 (2015). https://doi.org/10.1007/s00330-015-3781-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3781-5