Abstract
The long-term variations of fractional flow reserve derived from coronary computed tomography (FFRCT) after surgical (SAVR) or transcatheter (TAVR) aortic valve replacement in patients with severe aortic valve stenosis (AS) have not been investigated. A total of 25 patients with isolated, severe AS underwent coronary computed tomography with 3-vessel FFRCT analysis (Heartflow Inc.—Redwood City, California, USA) and measurement of total coronary volume (V), left ventricular mass (M) and their ratio (V/M) before and 6 months after SAVR or TAVR. A significant increase in V/M due to a decrease in left ventricular mass 6 months after intervention was observed, whereas total coronary volume did not change (coronary volume pre: 2924.5 ± 867.9 mm3, coronary volume post: 2844.2 ± 792.8 mm3, P = 0.158; LV mass pre: 151.7 ± 40.7 g, LV mass post: 127.3 ± 34.7 g, P < 0.001; V/M pre: 19.5 ± 4.1 mm3/g, V/M post: 22.7 ± 4.28 mm3/g, P = 0.002). FFRCT (expressed as area under the virtual pullback curve) remained constant. This proof-of-concept study showed that FFRCT was not subject to the confounding effect of left ventricular mass regression after SAVR or TAVR. Despite significant left ventricular remodeling at 6 months after AS treatment, FFRCT values remained constant. Further studies are needed comparing the performance of the different invasive and non-invasive coronary physiological indices in this patient cohort.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary physiology in the presence of severe aortic stenosis (AS) remains a clinically relevant subject of research. Severe AS causes substantial physiological distortion on the coronary and microcirculatory level: the stenosed valve behaves as a proximal tandem stenosis, increased left ventricular afterload leads to left ventricular hypertrophy, coronary flow reserve and coronary perfusion pressure are reduced and there is an altered response to hyperemic agents [1]. Many of these confounding factors are reversible after aortic valve replacement (AVR). Fractional flow reserve derived from coronary computed tomography (FFRCT) has emerged as a valuable non-invasive coronary physiological test [2]. Recently it was demonstrated that FFRCT is feasible and safe with a moderate to good diagnostic accuracy compared to invasive fractional flow reserve (FFR) in patients with severe AS [3]. So far, the long-term variations of FFRCT after AVR have not been investigated. In this study FFRCT was measured before and 6 months after surgical (SAVR) or transcatheter (TAVR) aortic valve replacement to investigate whether cardiac structural remodeling after relief of AS had an influence on FFRCT.
Methods
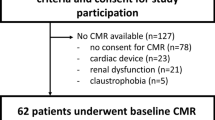
This is a single center, prospective observational study including 25 patients with AS eligible for SAVR or TAVR after heart team discussion. Adult patients with isolated, severe, normal flow, high gradient AS with preserved left ventricular ejection fraction as defined on echocardiography (peak velocity > 4 m/s, mean gradient > 40 mmHg, aortic valve area < 1.0 cm2, indexed aortic valve area < 0.6 cm2/m2, velocity ratio < 0.25) were included. Exclusion criteria were history of cardiac surgery or percutaneous cardiac intervention, history of acute coronary syndrome, other significant valvular heart disease, coronary artery stenosis necessitating revascularization, refusal or inability to give informed consent and contra-indication for any of the procedures or medications inherent to the study. All patients underwent thorough transthoracic echocardiography before and 6 months after the index procedure. The study protocol was approved by the hospital’s ethical committee, complied with the declaration of Helsinki and all patients signed informed consent. Patient inclusion took place between May 2019 and November 2020.
Invasive coronary angiography
Coronary angiography was performed by radial access according to standard practice in all patients. Only patients with epicardial stenosis < 30% (visual analysis by experienced operator) were included.
Coronary computed tomography angiography (CCTA)
CCTA was performed on 2 occasions: less than one month before and 6 months after AVR.
We maintained a time interval of 6 months because long-term follow-up studies have shown that up to 75% of left ventricular mass (LVM) regression occurred within the first 6 months following AVR [4]. All images were acquired with a 320 slice GE Revolution™ scanner. Bèta-blockers were administered to achieve a heart rate of less than 65 beats/minute when needed (metoprolol intravenously with a titration dose up to 15 mg) and all patients received nitroglycerin 0.4 mg sublingually before image acquisition to ensure maximal vasodilation. Importantly all patients received nitrates for the second scan as well, this was essential to make a reliable comparison between the 2 scans both for coronary volume as for FFRCT. FFRCT was analyzed by Heartflow Inc. (Redwood City, California, USA) in a blinded manner.
Patient-specific coronary geometries were derived from conventional CCTA images. Computational fluid dynamics and blood flow simulations were performed to calculate FFRCT values which were available at all points of the coronary tree. FFRCT values are presented as area under the virtual pullback curve (FFRCTAUC) by plotting the FFRCT value at every 0.1 mm versus length of the vessel (FFRCTAUC = Σ[FFRCT1 + FFRCT2/2 × (d2−d1)] with d for distance between points 1 and 2). For comparison, values were matched in length between the 2 scans. Based on the same CCTA images the ratio of total coronary volume to left ventricular myocardial mass was calculated. This involved the following steps: a three-dimensional patient-specific anatomic model of the epicardial coronary arteries was segmented, arteries were truncated, branches off the main epicardial coronary arteries greater than 1 mm in diameter were included and total arterial lumen volume (V) of the segmented epicardial coronary arteries was calculated. The volume of the myocardium traced from CCTA imaging data was multiplied by an average value of myocardial tissue density (1.05 g/ml) to calculate left ventricular myocardial mass (M). Finally, the ratio of total coronary lumen volume to left ventricular myocardial mass (V/M) was computed.
SAVR/TAVR procedure
Procedures were done according to standard hospital practice. TAVR was performed under conscious sedation through transfemoral access. SAVR was done by means of median sternotomy under cardiopulmonary bypass. Medtronic Corevalve™ Evolut™-R (Medtronic Inc., Minneapolis, MN), Carpentier-Edwards (Edwards Lifesciences, Irvine, CA) and Trifecta™ GT (Abbott, Illinois) bioprosthesis were used.
Statistical analysis
Primary endpoint of the study was the variation of left ventricular mass (M), total coronary volume (V), the ratio of these 2 variables (V/M) and FFRCTAUC at 6 months after intervention compared with baseline values. Comparison was done using Wilcoxon signed-rank test. A P-value < 0.05 was considered statistically significant.
Results
Twenty-five patients with isolated, severe AS without obstructive coronary artery disease signed informed consent. Three patients had insufficient image quality for FFRCT analysis so 22 patients were finally included (aortic valve area 0.77 ± 0.22 cm2, mean gradient 56 ± 17 mmHg, coronary Agatston score 208.6 ± 211.8, aortic valve Agatston score 2960.6 ± 1696.9, mean age 72.5 ± 8.5 years, 36% men, 86% underwent SAVR). See Table 1.
Pre-scan medication (nitrates in all patients and bètablockers to achieve heart rate < 65 beats per minute in 8 patients) was well tolerated, none had symptomatic hypotension or excessive bradycardia. SAVR and TAVR were successfully performed in all patients without any major adverse event. One patient received a permanent dual chamber pacemaker after TAVR because of high-degree atrioventricular block without influence on the image quality of the second CCTA. Any valvular or paravalvular regurgitation on transthoracic echocardiography after the procedure was graded < 1/4. At 6 months follow-up there was a significant improvement in all hemodynamic parameters. See Table 2.
A significant increase in V/M due to a decrease in left ventricular mass was observed, whereas total coronary volume did not change (coronary volume pre: 2924.5 ± 867.9 mm3, coronary volume post: 2844.2 ± 792.8 mm3, P = 0.158; LV mass pre: 151.7 ± 40.7 g, LV mass post: 127.3 ± 34.7 g, P < 0.001; V/M pre: 19.5 ± 4.1 mm3/g, V/M post: 22.7 ± 4.28 mm3/g, P = 0.002). FFRCTAUC (per vessel) and total FFRCTAUC (per patient = sum of 3 vessels) remained constant. See Table 2 and Figs. 1 and 2.
Discussion
This proof-of-concept study showed that despite a significant decrease in left ventricular mass and hence increase in V/M at 6 months after SAVR or TAVR, FFRCT remained constant.
Because AS has such a profound influence on coronary physiology, the 2 most widely used invasive coronary indices FFR and instantaneous wave-free ratio (iFR) have to be interpreted with caution in this subset of patients. So far, 2 studies have explored the long-term variations of coronary physiology after AVR. Scarsini et al. showed that FFR can decrease after TAVR at a median follow-up of 14 months in lesions with abnormal baseline value, whereas values remained stable when baseline FFR > 0.80 [5]. In contrast, Vendrik et al. showed a significant and consistent reduction of FFR values immediately post-TAVR, further lowering after 6 months follow-up; iFR did not change significantly [6]. Since its value can lower after TAVR, FFR could possibly ‘underestimate’ the severity of a coronary artery stenosis in AS. This is caused by a blunted hyperemic response that is restored after relief of AS through recovery of microcirculatory function and coronary flow reserve resulting in more hyperemic systolic flow [7]. Therefore, a practical solution would be to measure FFR after AVR. The question here remains when to do this: directly after TAVR which is most straightforward since the patient is still on the table (for obvious reasons this is cumbersome after SAVR) or after a longer period of time i.e., after full restoration of coronary and microcirculatory physiology? iFR is less subject to change after AVR since this is a resting index measured in the diastolic wave-free period only. However, the ischemic threshold of iFR seems to be lower probably because of the higher coronary resting flow associated with severe AS altering the pressure-flow relationship during the diastolic wave-free period [8, 9]. Therefore it is important to investigate if and how physiological measurements change after relief of AS. This informs us about the proper applicability of the test in question.
FFRCT uses computational fluid dynamics to calculate 3-vessel virtual FFR based on CCTA, presuming an intact microcirculatory function with a preserved vasodilatory capacity mimicking hemodynamics as they would be after AS treatment [10]. In a recent study it was demonstrated that FFRCT is feasible and safe with a moderate to good diagnostic accuracy compared to invasive FFR in patients with severe AS. There was a tendency of higher mean FFR values compared to mean FFRCT values probably explained by the mechanisms described above [3]. Until now, it has not been investigated if FFRCT changes after AVR. Theoretically, this could be because the estimation of coronary blood flow used for FFRCT calculation is based on LVM that often regresses after treatment of AS [10]. Lower LVM causes lower absolute coronary flow (ml/min) with the same perfusion (ml/min/g) thus theoretically leading to a lower pressure loss and hence a higher FFRCT value [11]. This means FFRCT could ‘overestimate’ the severity of a coronary artery stenosis in AS compared to FFR. Regression of LVM after AVR is translated into a higher V/M ratio. V/M has already been studied in other patient populations with somewhat conflicting data concerning its effect on FFRCT values. A low V/M on CCTA in patients with stable coronary artery disease was an independent predictor of invasive FFR < 0.80 irrespective of the presence of obstructive coronary stenosis [12]. V/M was lower in hypertrophic cardiomyopathy compared to controls, especially when there was important septal hypertrophy. This resulted in lower cumulative 3-vessel FFRCT values but somewhat surprising, no difference in FFRCT was seen in the mid portion of the left anterior descending coronary artery [13]. Patients with primary microvascular angina had lower V/M (intrinsically smaller caliber coronary arteries versus impaired vasodilatory response to nitroglycerin) compared to controls. This did not lead to lower FFRCT values [14]. Recently, it was shown that females compared to males have higher V/M for the same degree of coronary stenosis which was associated with a higher FFRCT value [15]. Concerning our study, V/M could be regarded as a quantitative metric of imbalance between coronary blood supply and myocardial demand in AS that improves to a certain extent after AVR. It could therefore serve as a future marker of ‘maladaptive’ (low V/M) versus ‘adaptive’ (high V/M) left ventricular hypertrophy in AS. A low V/M ratio could also provide one of several explanations why a high LV mass independently conveys a worse prognosis in AS [16, 17].
Despite a significant increase in V/M at 6 months after AVR, FFRCTAUC remained constant. FFRCTAUC quantifies total epicardial conductance and pressure loss along the vessel [18]. Previous work has shown an excellent correlation between this virtual FFRCT pullback curve and the invasive FFR pullback curve with nearly identical curves in non-obstructive segments [19]. We used this parameter rather than a single point FFRCT value for comparison because these were all patients without significant focal stenosis. Also, we did not use the distal or nadir FFRCT value (defined as the lowest FFRCT value in a given system) since these are sometimes prone to false positivity [20]. We did see however a gradual decline of FFRCTAUC from the proximal to the distal part of the vessel (without ever reaching absolute FFRCT value < 0.75) reflecting the diffuse coronary disease that was present in our patients which is in concordance with previous data using invasive FFR pullbacks [21]. See Fig. 3.
An older study showed a decrease in coronary size after AVR with an even more important regression of LVM resulting in normalization of V/M compared to controls without AS. We did not see any change in coronary size after AVR, keeping in mind that we used total coronary volume instead of proximal coronary artery diameter [22]. Furthermore, our patients did not have strictly normal coronary arteries but diffuse disease with often high calcium burden and extensive atherosclerosis possibly hampering coronary vasoreactivity.
The main reason we excluded patients with angiographically moderate or severe stenosis is the duration of follow-up during which revascularization would not have been possible due to the concept and the protocol of the study. After percutaneous coronary intervention or coronary artery bypass grafting the repeat CCTA would not be interpretable. Nevertheless, because of the propensity for myocardial ischemia in severe AS, it is worthwhile and interesting to examine coronary physiology even in the absence of angiographically significant coronary artery disease. Impairment of coronary flow reserve with microvascular dysfunction, low aortic valve area, high rate pressure product, low coronary perfusion pressure and short diastolic perfusion time are all hemodynamic factors causing myocardial ischemia even without coronary artery stenosis. Many of these are at least partially reversible after AS relief. [1, 23]. See Table 2.
A possible explanation for the stable FFRCT values is that our patient population did not have the severe left ventricular hypertrophy sometimes seen in severe AS since mean LVM at baseline was 151.7 ± 40.7 g [24]. This could mean that the absolute change in mass and thus V/M was not large enough (although a very substantial mass reduction of 16% was seen) to induce a significant change in FFRCTAUC. Also, since LVM regression after AVR is an ongoing process that can continue for years, we do not know what the evolution of coronary physiology will be after a longer period of time [24, 25]. Another possibility is the absence of focal stenosis with all baseline FFRCT values > 0.75 making our findings concordant with those of Scarsini et al. mentioned before [5].
Importantly, FFRCT showed low time-to-time biological variability and proved to be a robust and reproducible test in the same patient on 2 totally different occasions with a 6 months’ time interval. Despite massive changes in the heart first induced by the presence of severe AS and afterwards by AVR, FFRCT was not vulnerable to these confounding factors. The most important confounders in comparing AS and post-AVR patients are most likely CCTA image quality and change in LVM. None of them caused distortion in the performance of FFRCT.
Further research is needed in patients with AS and concomitant focal coronary artery stenosis.
Theoretically it is very likely that FFRCT will remain stable even in a 50–70% stenosis since the major driver for the invasive FFR lowering is restoration of microcirculatory function and FFRCT is blinded to this change. This is inherent to the technique which uses fixed inlet (aortic) and outlet (microcirculatory) boundary conditions making FFRCT blinded to the presence of AS or an aortic bioprosthesis, with epicardial coronary anatomy being the main determinant of FFRCT [26, 27].
Validation of FFRCT against the other physiological indices (invasive versus non-invasive and hyperemic versus resting) is certainly needed. A particularly appealing question is whether FFRCT before AVR could predict invasive FFR after intervention i.e., after full recovery of microcirculatory function and coronary flow reserve. As such, CCTA could become a one-stop test in patients with AS to evaluate severity of valve disease (aortic valve calcium score), severity of coronary artery disease (Agatston score, percentage stenosis, FFRCT), feasibility of TAVR (sizing, vascular access), left ventricular mass and V/M ratio. When FFRCT is clearly negative or positive far away from its ischemic cut-off point of 0.80, one could safely defer from revascularization or proceed to revascularization respectively without further testing. In case of borderline values, invasive physiological testing would be indicated by measuring iFR or FFR after AVR but further studies with clinical endpoints are needed to validate this hypothesis. Since FFRCT did not change 6 months after AVR, the value obtained before AVR could be used in deciding whether revascularization is indicated. Should the FFRCT values have gone up due to regression of LV mass, caution would have been needed in interpreting the value before AVR especially when ending up in the grey-zone (0.75–0.80). These values could thus have become negative (> 0.80) after AVR, obviating the need for revascularization.
Study limitations
Our study has several limitations. This is a proof-of-concept study with a small number of patients having isolated AS without focal coronary artery stenosis, limiting the conclusions that can be drawn. Specific subanalyses were not possible due to the small sample size. Invasive FFR and iFR were not measured and thus could not be used as a reference. However, both FFR and iFR their selves are not free from confounding factors as outlined above, cautioning to consider them as gold standard tests in severe AS. Vessel specific V/M data of the different coronary territories were not available which would have added an extra layer of data. Finally, patients were treated predominantly with SAVR in the current TAVR era but this was subordinate to the purpose of the study.
Conclusion
This proof-of-concept study showed that FFRCT can be performed in patients with isolated, severe AS and with a surgical or transcatheter aortic bioprosthesis in place. Despite significant left ventricular remodeling 6 months after AVR, FFRCT values remained constant and were not vulnerable to the confounding effect of LVM regression. Further validation studies with clinical endpoints are needed before FFRCT could be used as a reliable stand-alone coronary test in patients with severe AS scheduled for AVR. The findings of this study add another piece of the puzzle needed to make appropriate decisions in the vexing combination of AS and coronary artery disease.
Data availability
N/A
Code availability
N/A
References
Michail M, Davies JE, Cameron JD et al (2018) Pathophysiological coronary and microcirculatory flow alterations in aortic stenosis. Nat Rev Cardiol 15:420–431
Min JK, Taylor CA, Achenbach S et al (2015) Noninvasive fractional flow reserve derived from coronary CT angiography. Clinical data and scientific principles. JACC 8:1209–22
Michail M, Ihdayhid AR, Comella A et al (2021) Feasibility and validity of computed tomography derived fractional flow reserve in patients with severe aortic stenosis. Circ Cardiovasc Interv 14:e009586
Biederman RWW, Magovern JA, Gtrant SB et al (2011) LV reverse remodeling imparted by aortic valve replacement for severe aortic stenosis; is it durable? A cardiovascular MRI study sponsored by the American heart association. J Cardiothorac Surg 6:53–61
Scarsini R, Lunardi M, Venturi G et al (2020) Long-term variations of FFR and iFR after transcatheter aortic valve implantation. Int J Cardiol 317:37–41
Vendrik J, Ahmad Y, Eftekhari A et al (2020) Long term effects of transcatheter aortic valve implantation on coronary hemodynamics in patients with concomitant coronary artery disease and severe aortic stenosis. J Am Heart Assoc 9:e015133
Zelis JM, Tonino PA, Johnson NP (2020) Why can fractional flow reserve decrease after transcatheter aortic valve implantation? J Am Heart Assoc 9:e015806
Scarsini R, Pesarini G, Zivelonghi C et al (2017) Coronary physiology in patients with severe aortic stenosis: comparison between fractional flow reserve and instantaneous wave-free ratio. Int J Cardiol 243:40–46
Scarsini R, Cantone R, Venturi G et al (2019) Correlation between intracoronary physiology and myocardial perfusion imaging in patients with severe aortic stenosis. Int J Cardiol 292:162–165
Taylor CA, Fonte TA, Min JK (2013) Computational fluid dynamics applied to cardiac computed tomography for noninvasive quantification of fractional flow reserve: scientific basis. J Am Coll Cardiol 61:2233–2241
Johnson NP, Kirkeeide RL, Gould KL (2019) Same lesion, different artery, different FFR!? JACC 12:718–719
Taylor CA, Gaur S, Leipsic J et al (2017) Effect of the ratio of coronary arterial lumen volume to left ventricle myocardial mass derived from coronary CT angiography on fractional flow reserve. J Cardiovasc Comput Tomogr 11:429–436
Sellers SL, Fonte TA, Grover R et al (2018) Hypertrophic cardiomyopathy: new insights into coronary artery remodeling and ischemia from FFRCT. J Cardiovasc Comput Tomogr 12:467–471
Grover R, Leipsic JA, Mooney J et al (2017) Coronary lumen volume to myocardial mass ratio in primary microvascular angina. J Cardiovasc Comput Tomogr 11:423–428
Fairbairn T, Dobson R, Hurwitz-Koweek L et al (2020) Sex differences in coronary computed tomography angiography-derived fractional flow reserve. Lessons from advance. JACC 13:2576–2587
Minamino-Muta E, Kato T, Morimoto T et al (2017) Impact of the left ventricular mass index on the outcomes of severe aortic stenosis. Heart 103:1992–1999
Gerdts E, Rossebo AB, Pedersen TR et al (2015) Relation of left ventricular mass to prognosis in initially asymptomatic mild to moderate aortic valve stenosis. Circ Cardiovasc Imaging 8:e003644
Collet C, Katagiri Y, Miyazaki Y et al (2018) Impact of coronary remodeling on fractional flow reserve. Circulation 137:747–749
Mizukami T, Tanaka K, Sonck J et al (2020) Evaluation of epicardial coronary resistance using computed tomography angiography: a proof of concept. J Cardiovasc Comput Tomogr 14:177–184
Cami E, Tagami T, Raff G et al (2019) Fractional flow reserve by coronary computed tomography (FFRCT): impact of measurement site on assessment of lesion-specific ischemia and statistical performance. J Am Coll Cardiol 73:1449
De Bruyne B, Hersbach F, Pijls NH, Bartunek J, Bech JW, Heyndrickx GR et al (2001) Abnormal epicardial coronary resistance in patients with diffuse atherosclerosis but “normal” coronary angiography. Circulation 104:2401–2406
Villari B, Hess OM, Meier C et al (1992) Regression of coronary artery dimensions after successful aortic valve replacement. Circulation 85:972–978
Zelis JM, Tonino PAL, Pijls NHJ et al (2020) Coronary microcirculation in aortic stenosis: pathophysiology, invasive assessment and future directions. J Interv Cardiol. https://doi.org/10.1155/2020/4603169
Chau KH, Douglas PS, Pibarot P et al (2020) Regression of left ventricular mass after transcatheter aortic valve replacement: the PARTNER trials and registries. J Am Coll Cardiol 75:2446–2458
Lund O, Emmertsen K, Dorup I et al (2003) Regression of left ventricular hypertrophy during 10 years after valve replacement for aortic stenosis is related to the preoperative risk profile. Eur Heart J 24:1437–1446
Sankaran S, Kim HJ, Choi G et al (2016) Uncertainty quantification in coronary blood flow simulations: impact of geometry, boundary conditions and blood viscosity. J Biomech 49:2540–2547
Johnson NP, Kirkeeide RL (2013) Gould KL Coronary anatomy to predict physiology. Fundamental limits. Circ Cardiovasc Imaging 6:817–832
Funding
This work was supported by an unrestricted grant from Medtronic, Inc. and LivaNova, PLC.
Author information
Authors and Affiliations
Contributions
All authors read and approved the manuscript and contributed equally to the writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
Approved by the local ethical committee.
Consent to participate
Informed consent was signed by all participants.
Consent for publication
N/A
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Michiels, V., Andreini, D., Conte, E. et al. Long term effects of surgical and transcatheter aortic valve replacement on FFRCT in patients with severe aortic valve stenosis. Int J Cardiovasc Imaging 38, 427–434 (2022). https://doi.org/10.1007/s10554-021-02401-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02401-1