Abstract
Objectives
Renal denervation (RDN) is a promising therapy for resistant hypertension. RDN is assumed to decrease sympathetic activity. Consequently, RDN can potentially increase renal oxygenation. Blood oxygen level-dependent MRI (BOLD-MRI) provides a non-invasive tool to determine renal oxygenation in humans. The aim of the current study was to investigate the effect of RDN on renal oxygenation as determined by BOLD-MRI.
Methods
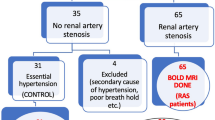
Patients with resistant hypertension or the inability to follow a stable drug regimen due to unacceptable side effects were included. BOLD-MRI was performed before and 12 months after RDN. Twenty-seven patients were imaged on 3 T and 19 on 1.5 T clinical MRI systems.
Results
Fifty-four patients were included, 46 patients (23 men, mean age 57 years) completed the study. Mean 24-h BP changed from 163(±20)/98(±14) mmHg to 154(±22)/92(±13) mmHg (p = 0.001 and p < 0.001). eGFR did not change after RDN [77(±18) vs. 79(±20) mL/min/1.73 m2 ; p = 0.13]. RDN did not affect renal oxygenation [1.5 T: cortical R2*: 12.5(±0.9) vs. 12.5(±0.9), p = 0.94; medullary R2*: 19.6(±1.7) vs. 19.3(1.4), p = 0.40; 3 T: cortical R2*: 18.1(±0.8) vs. 17.8(±1.2), p = 0.47; medullary R2*: 27.4(±1.9) vs. 26.7(±1.8), p = 0.19].
Conclusion
The current study shows that RDN does not lead to changes in renal oxygenation 1 year after RDN as determined by BOLD-MRI.
Key Points
• Renal denervation significantly decreased ambulatory blood pressure.
• Renal denervation did not change renal oxygenation as determined by BOLD-MRI.
• Absence of a change in renal oxygenation might be explained by autoregulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal hypoxia is thought to be both a result as well as a cause of hypertension, potentially inducing a vicious cycle. In several animal models of hypertension, cortical as well as medullary oxygenation is lower in hypertensive animals compared to controls [1]. This can be a result of increased sodium retention, a process requiring active sodium transport, which might lead to increased tubular oxygen consumption. Moreover, the renin angiotensin system (RAAS) and the sympathetic nervous system (SNS) are activated in hypertension, both influencing renal perfusion and oxygenation.
Animal studies show that renal ischemia triggers activation of the SNS. Even a small lesion by intrarenal injection of phenol chronically increases central sympathetic activation resulting in hypertension, without affecting kidney function, in rats [2]. The blood pressure (BP)-elevation after the intrarenal injection can be prevented by prior denervation of the phenol injected kidney [2], which demonstrates a crucial role of intact renal innervation for afferent signalling from the kidney to the vasomotor centre.
Renal denervation (RDN), a catheter-based approach developed to disrupt the renal sympathetic nerves using radio frequency energy, is a promising therapy for resistant hypertension. The first clinical studies, in a relatively small number of patients, showed that this technique appears safe and effective [3–5]. Office systolic blood pressure (SBP)/diastolic blood pressure (DBP) reduced by 32/12 mmHg 6 months after RDN [4]. RDN is assumed to decrease sympathetic activity, resulting in altered sodium handling by the kidneys and a decrease in peripheral vascular resistance. Consequently, RDN may potentially improve renal oxygenation, and thereby remove the trigger for hypertension.
Blood oxygen level-dependent (BOLD)-MRI provides a non-invasive tool to determine renal oxygenation in humans. BOLD-MRI uses the magnetic properties of deoxyhemoglobin. Deoxyhemoglobin is paramagnetic, causing a decrease in signal on T2*-weighted images. The apparent relaxation rate R2* (=1/T2*) is proportional to the concentration of deoxyhemoglobin. Increased R2* levels imply increased levels of deoxyhemoglobin which can be related to reduced partial pressures of oxygen in tissue [6]. Renal oxygenation reflects the balance between regional oxygen supply and consumption, principally for tubular transport [7]. There is a non-homogenous distribution of oxygen within the kidneys. pO2 sharply declines at the cortico-medullary junction. The renal medulla functions at levels of limited oxygen supply, with a pO2 as low as 25 mmHg under normal physiologic conditions [7].
The aim of current study was to investigate the effect of RDN on renal oxygenation determined by BOLD-MRI.
Methods
Study population
Patients both with resistant hypertension (defined as a SBP ≥160 mmHg, despite use of ≥3 antihypertensive drugs) as well as patients fulfilling the same BP criteria (n = 46), but without optimal pharmacological treatment due to intolerance for antihypertensive drugs, were included in the present study (n = 8). Major contraindications for inclusion were an estimated glomerular filtration rate (eGFR) <30 mL/min/1.73 m2, secondary causes of hypertension, and a history of renal artery stenting or severe co-morbidity. All patients were screened using a standardized screening protocol, described in detail in a recent paper [8]. The protocol had three aims: firstly, to confirm the presence of hypertension using ambulatory BP monitoring (ABPM); secondly, to exclude secondary forms of hypertension; and finally, to study the eligibility of the renal arteries to undergo RDN by contrast-enhanced magnetic resonance angiography (MRA).
The study protocol was carried out with the approval of the ethics committee of the University Medical Center Utrecht, and all patients gave written informed consent. The current study is registered as NCT01427049.
Temporal medication stop
At baseline and 12 months after RDN, we considered whether it would be safe to stop antihypertensive medication for 2 weeks prior to the tests [8]. This was done as part of our standardized clinical work-up for patients with complicated hypertension [8] to improve standardization of the test conditions since antihypertensive drugs influence BOLD-MRI. If considered unsafe to stop antihypertensive medication, patients were switched to doxazosin and/or diltiazem, which are neutral drugs [9, 10]. The decision to stop antihypertensive drugs was based on clinical judgement with emphasis on (cardiovascular) medical history. During the medication-free interval, patients were regularly contacted by telephone by trained nurses or a physician. Also, patients were informed to contact us if they developed symptoms. After the test period, patients restarted their medication.
Measurements
All measurements at baseline, as part of the standardized screening protocol, and 12 months after RDN were performed during the medication-free interval. An ABPM was taken non-invasively using WatchBP O3 (Microlife Inc., Widnau, Switzerland) with readings taken every 30 min during day and every 60 min at night. Twenty-four-hour urine was collected and sodium (mmol/24 h) was analysed. Three days before the investigations, patients were asked to maintain a constant diet in order to avoid large fluctuations in sodium balance. A blood sample was drawn and creatinine (μmol/L) was determined.
BOLD-MRI
MRIs were performed in the afternoon. Patients were scanned either on a 1.5 T (Ingenia, software release 4.1, Philips Healthcare, Eindhoven, the Netherlands) or 3 T (Achieva, release 3.2, Philips Healthcare, Eindhoven, the Netherlands) commercially available MR systems. In brief, the MR imaging protocol consisted of obtaining localizer images to locate the kidneys, after which coronal (three partitions) and transverse (six partitions) T2*-weighted imaging was performed with the following echo times: 4.6 ms, 9.2 ms, 13.8 ms, 18.4 ms, 23 ms, 27.6 ms, 32.2 ms, 36.8 ms, 41.4 ms, 46 ms, 50.6 ms, 55.2 ms, 59.8 ms, 64.4 ms, 69 ms, 73.6 ms, 78.2 ms, 82.8 ms, 87.4 ms, 92 ms. All data were acquired during breath-hold. We acquired one slice per breath-hold. Acquisition time per slice was 13.2 s. Total acquisition time was three or six times 13.2 s for the coronal and transverse scans, respectively, plus the time in between the breath-holds. We used SENSE for parallel imaging with a SENSE acceleration factor of 1.5. No signal averaging was applied. The receiver BW was 310/620 Hz at 1.5/3 T. Only linear shimming was used. The voxel sizes were 1.49 × 1.50 × 5.0 mm3 and the slice gap 7 mm. Coronal field of view (FOV) was 375 × 298 mm (1.5 T, fold-over direction (FD) right-left) or 298 × 375 mm (3 T, FD feet-head) and transversal FOV was 298 × 375 mm (FD right-left). Flip angle was 25° and TR was 94 ms (1.5 T) or 95 ms (3 T).
Regions of interest (ROIs) of the whole kidneys were drawn in the T2* map. Areas affected by artefacts were avoided in the selection of the ROIs. The R2* map was calculated from the T2* data by fitting an exponential curve to individual voxels over the echo times. MRIs were analyzed using the compartmental method proposed by Ebrahimi et al. [11] using an in-house developed Matlab tool (MathWorks Inc, Natick, MA, USA). The histogram of the R2* map was calculated and fitted to a Gaussian function (cortex) and a gamma function (medulla) (Fig. 1). To differentiate medulla, collecting system, and vessels objectively, a semi-automatic filter was applied to the R2* maps. High intensity voxels, representing collecting system, and low intensity voxels, representing blood vessels, were excluded, as well as the four adjacent voxels (Fig. 1). To obtain a measure for hypoxia, the cut-off R2*-value of the 10 % most hypoxic voxels (90th percentile of the histogram, P90) was used (Fig. 1). Muscle ROIs of the psoas muscle were obtained in the coronal slices in both the baseline and follow-up scan to assess scan reproducibility since muscle R2*-levels are not affected by RDN.
a: T2* image of the kidneys. ROIs are depicted in red. b: R2* image of the kidneys. ROIs are depicted in red. c: Exclusion of vessels and the collecting system. The collecting system is excluded by the filter (depicted in red). d: Histogram of the R2* map. According to the compartmental method, cortex is fitted to a Gaussian (blue) function and medulla to a gamma (pink) function. The sum (red) fits the histogram of the R2* map shown in the figure
Percutaneous renal denervation
Renal angiograms were performed to confirm anatomic eligibility. Fifty-one of 54 patients were treated using the Symplicity Flex device (Medtronic, Minneapolis, MN, USA). In these patients, using local anaesthetics, a 6Fr sheath was introduced via a femoral artery access site. Bilateral treatment of the arteries was performed using series of 2-min radio frequency (RF) energy deliveries along each artery [12]. These treatment points were made in a circumferential way with a minimum of 5 mm distance in between the treatment points. In two patients the EnligHTN system (St Jude, St. Paul, MN, USA) and in one patient the Oneshot system (Covidien, Mansfield, MA, USA) was used. The EnligHTN system is a non-occlusive, multi-electrode basket design, enabling four ablations in one session of 90 s [13]. The Oneshot system is an irrigated RF balloon equipped with a spiral monopolar electrode for 360° of ablation [14].
Data analysis
A patient was classified as a responder of treatment with RDN when average daytime SBP determined by ABPM decreased by ≥ 5 mmHg. Estimated glomerular filtration rate (eGFR) was calculated on the basis of the CKD-epi formula [15].
Prescribed dosages of antihypertensive drugs were converted to defined daily doses (DDD) using conversion factors as provided by the World Health Organization (WHO) Drug Classification (http://www.whocc.no/atcddd/). Using DDDs and the total prescribed dosages, daily use (DU) of all antihypertensive drugs was calculated.
The following subgroup analyses were performed: 1) patients who stopped medication twice regardless of the use of rescue medication (the latter does not influence BOLD-MRI), 2) patients who stopped medication twice and no rescue medication twice or used the same rescue medication. This approach was chosen since rescue medication does not influence BOLD-MRI and laboratory parameters; it does, however, influence BP.
Analysis of BOLD-MRI data was done by two investigators (EV and AB), blinded to patient information and other results from the standardized screening protocol. Five patients from the 1.5 T scanner and five from the 3 T scanner were randomly selected to determine intra-reader reproducibility. Eight patients from the 1.5 T scanner and eight patients from the 3 T scanner were randomly selected to determine inter-reader reproducibility.
For the statistical analysis, we combined the results of the coronal and transverse slices. Just averaging the R2* values obtained from the transverse and coronal slices would introduce a bias. Because of kidney anatomy and due to exclusion of collecting system and artefacts, the amount of kidney tissue represented by the transverse or coronal slices could differ significantly. Therefore, the total number of voxels of all six coronal slices together was calculated. The same was done for the three transverse slices. Based on the number of voxels, a weighted average was calculated: R2 = no_voxels_trans/no_voxels_total*R2trans + no_voxels_cor/no_voxels_total*R2cor. This calculation was performed both for the medullary and the cortical R2* value. Averaging transversal and coronal values implies that some of the kidney tissue was weighted twice, because the slices intersect. The number of voxels included in both the coronal and transverse slices was estimated to be around 8 %.
To combine data from the 1.5 T and the 3 T scanner, z-scores for the change in R2* levels for both field strengths were calculated and combined. A z-score is calculated for each individual as the obtained individual measurement minus the mean value of the group divided by the standard deviation around the group average [z-score = (participant value - μ)/σ].
Statistical analysis
All variables were reported as mean ± SD, median (range), or as proportion when appropriate. The Intra-class correlation coefficient (two-way mixed model, absolute agreement) and the Bland-Altman method (defining bias and variation by calculating the mean difference between the observers, the standard deviations of the differences, and the 95 % limits of agreement) were used to determine inter- and intrareader reproducibility.
The unpaired Students t-test and the chi-square test were used when applicable to compare baseline data between patients who stopped medication twice and the group who could not stop twice.
Paired sample analysis was done using the paired t-test or its nonparametric variant when applicable.
Linear regression analysis was used to analyze the association between the change in ABPM (independent variable) and change in R2* values of the cortex, medulla, and P90 (dependent variables). Multivariable models were applied adjusting for variables related to BOLD and BP (change in eGFR, change in 24-h urinary sodium excretion, and the change in hemoglobin). The number of variables in the multivariable models was restricted by the limited sample size.
A two-sided p value of <0.05 was considered to be statistically significant. All analyses were performed with the SPSS statistical package version 20 (IBM SPSS Data Collection, Chicago, IL, USA).
Results
Fifty-four patients were included in the present study; 46 patients completed follow-up. Baseline characteristics of the patients with a complete follow-up (n = 46), are shown in Table 1. Thirty-two patients stopped medication twice of which 27 patients stopped medication twice and used the same or no rescue medication twice. Twenty-seven patients (59 %) were scanned using a 1.5 T system, 19 patients (41 %) with a 3 T system. Inter- and intrareader reproducibility of R2* values of the cortex, medulla, and P90, were considered excellent based on the ICC (range: 0.957 – 0.999) as well as the Bland-Altman method (Appendix 2).
From two patients, both baseline and follow-up scans (coronal and transverse scans) were excluded from analysis, in one patient because of multiple cysts and in the other because of motion artefacts. From two patients, both the coronal as well as the transverse scans made at baseline were excluded because of motion artefacts. From 42 patients, pre- and post-imaging is available. In seven of these patients, only the coronal or transverse images were excluded. In five of these patients, these images were excluded because of motion artefacts, one because of erroneous shimming and one because of multiple eddy current artefacts visible in the R2* map.
Renal denervation
On average, 11.3 (±3.8) ablations were applied per patient. Periprocedurally, two patients had a minor bleeding at the puncture site, which was treated with compression.
Change in blood pressure and kidney function after RDN
Mean 24-h BP changed from 163(±20)/98(±14) mmHg to 154(±22)/92(±13) mmHg (p = 0.001 and p < 0.001, Table 2). Mean daytime BP changed from 168(±21)/102(±15) mmHg to 158(±23)/96(±13) mmHg (p = 0.001 and p < 0.001, Table 2). The decrease is less pronounced in the subgroup of patients who stopped medication twice (twice no rescue medication or twice the same rescue medication), but still significant (Table 2). Eleven patients (42 %) were classified as responder in this subgroup. Daytime heart rate (HR) did not change in the total group of patients and in the subgroup. The daily use of antihypertensive drugs did not change significantly [5.5 (±3.4) vs. 4.8 (±3.5), p = 0.18, Table 2]; eGFR remained stable 12 months after RDN compared to baseline [77 (±18) mL/min/1.73 m2 vs. 79 (±20) mL/min/1.73 m2 , p = 0.13, Table 2]. Average sodium excretion did not change: at baseline 149(±66) mmol/24-h and after 12 months 150(±83) mmol/24-h (p = 0.93).
Effect of RDN on renal oxygenation
As expected, the R2* values were a factor of 1.4 higher on the 3 T MR. Table 3 shows weighted mean baseline and 12-month follow-up R2* values of the cortex, medulla, and P90 for both field strengths. R2* levels did not change after RDN, including in the subgroup of patients who stopped medication twice (Table 4) or patients classified as responders (Table 5). The change in R2*values was not related to the change in daytime SBP in a univariate model, nor in multivariate models adjusting for the change in eGFR, the change in 24-h sodium excretion, and change in hemoglobin.
Muscle R2* levels did not change (Tables 3, 4 and 5), implying good reproducibility.
Discussion
In this study we demonstrate in hypertensive patients that renal BOLD did not change after treatment with RDN. Also, in the subgroup of patients classified as responder, BOLD not did alter after treatment.
BOLD-MRI gives information on renal oxygenation. The oxygen level within the kidney reflects the balance between regional oxygen supply and oxygen consumption. Oxygen supply is controlled by systemic and intrarenal factors that control intrarenal blood-flow and distribution, oxygen capacity of the blood, and the specific structure of the microcirculation of the kidney. The consumption is influenced by GFR, tubular and ion-pump mass, and various regulators that control transport activity [7]. Changes in either oxygen supply or demand alter the oxygen level. It is possible that RDN increases renal oxygenation as a consequence of decreased sympathetic activation resulting in a decreased renal vascular resistance and reduced activity of the RAAS. Decreased levels of aldosterone will result in reduced reabsorption of sodium in the collecting tubules, an active process. As a consequence of this, less oxygen will be used.
Our study shows that renal BOLD did not change after treatment with RDN although a reduction in BP was observed. This suggests that RDN did not affect renal oxygenation. Ott et al. showed that despite a decrease in BP, renal perfusion, determined by MRI with arterial spin labelling (ASL), did not change 3 months after RDN in 19 patients with resistant hypertension. Renal vascular resistance, calculated from BP and perfusion measured by ASL, was significantly reduced after RDN [16]. This is in line with another study showing that RDN reduced the renal resistive index, assessed by duplex ultrasound, 6 months after RDN in 88 patients with resistant hypertension [17]. So, it is very well possible that because renal perfusion did not change after RDN, also renal BOLD was unaffected. This can be the result of tight autoregulation in the kidneys.
Several issues need to be briefly discussed when considering the possible reason(s) for the absence of an effect, including both methodological, i.e. MRI-related issues, but also intervention, i.e. RDN-related issues.
It is important to realize that BOLD-MRI is sensitive to changes in medullary oxygenation since the medullary oxygen level lies on the linear part of the hemoglobin oxygenation curve, and is, therefore, sensitive to small changes in oxygen tension [18]. BOLD-MRI is, however, less sensitive to changes in cortical oxygenation, because cortical blood pO2 lies on the shoulder of the curve [18]. Thus, larger differences in oxygenation are necessary to observe similar changes in the R2* signal for the cortex compared with the medulla. A possible small effect of RDN on cortical oxygenation could, therefore, be missed using BOLD-MRI.
P90 (90th percentile of the histogram) gives information on the amount of hypoxia. This measure can be informative since in cases of renal injury, hyperfiltration and hypertrophy of uninjured nephrons can take place. These nephrons have a high metabolic demand, in contrast with injured nephrons. As a consequence, there can be a heterogeneous distribution of hypoxia in the kidney, which might not be detected using average R2* levels. Our study shows that P90 also did not change after RDN.
Another possible reason for the absence of an effect is that the RDN procedure was unsuccessful, at least in some patients. The high percentage of non-responders in our study may indicate that RDN was not complete in these patients, and that as a consequence RDN did not affect BP and renal oxygenation. However, in the subgroup of patients classified as responder, renal oxygenation also did not change.
We quantified the BP-lowering effect using ABPM. An ABPM offers a large number of BP measurements, during both day- and night-time. This results in a more precise assessment of BP compared to single measurements [19]. ABPM is also recommended in the follow-up of resistant hypertension in the guidelines from the European Society of Hypertension and the European Society of Cardiology [20]. Our study shows that RDN significantly reduces BP, determined by ABPM. Forty-two percent of the patients were classified as a responder. This percentage is lower compared to the study of Mahfoud et al investigating the effect of RDN on ABPM in 346 patients with uncontrolled hypertension (303 patients with resistant hypertension and 43 with pseudoresistant hypertension) 3, 6, and 12 months after RDN [21]. This studied identified 70 % of the 80 patients with resistant hypertension who completed 12 months follow-up as responder (defined as a decrease in SBP ≥5 mmHg of the 24-h ABPM) [21].
An important strength of our study is the standardization of antihypertensive drugs and the use of ABPM. This is important for quantifying the effects on both BP and BOLD-MRI. ABPM was assessed during a medication-free interval before and 12 months after RDN. This excludes the potential disturbance by antihypertensive medication. Pharmacologic treatment is likely to be changed during the 12 months after RDN and possibly drug adherence can be improved in some patients. Other studies may have overestimated the effect of RDN due to confounding by pharmacological treatment. Further, some medications have been shown to affect renal BOLD. Several studies have shown the effect of furosemide on BOLD [22–24]. This diuretic reduces the active sodium transport in the ascending loop of Henle, an oxygen-consuming process. BOLD-MRI detects this drop in medullary and, to a lesser degree, cortical oxygenation. Moreover, losartan, an angiotensin II receptor antagonist, is known to decrease cortical R2* levels [25]. Recently, we have shown that renin inhibitors affect the BOLD signal [26]. Unfortunately, the medication stop was not possible in all patients.
Several limitations need to be mentioned. Assessment of oxygenation of the kidneys, either by direct measurement or indirectly by BOLD-MRI, does not distinguish between (changes in) oxygen supply and consumption. It is, therefore, not possible to investigate the association between renal blood flow or oxygen consumption (mostly influenced by tubular transport) and the variables investigated in the present study. Further, a specific limitation of our study can be the use of two different field strengths. To combine the data, we used z-scores.
In conclusion, our study shows that RDN does not alter renal oxygenation in patients with hypertension as assessed by BOLD-MRI.
Abbreviations
- ABPM:
-
Ambulatory BP monitoring
- BOLD-MRI:
-
Blood oxygen level dependent
- BP:
-
Blood pressure
- CCT:
-
Captopril challenge test
- DBP:
-
diastolic blood pressure
- eGFR:
-
Estimated glomerular filtration rate
- ICC:
-
Intra-class correlation coefficient
- RAAS:
-
Renin angiotensin aldosterone system
- RDN:
-
Renal denervation
- R2*:
-
Apparent relaxation rate
- SBP:
-
Systolic blood pressure
References
Welch WJ (2006) Intrarenal oxygen and hypertension. Clin Exp Pharmacol Physiol 33:1002–1005
Ye S, Gamburd M, Mozayeni P, Koss M, Campese VM (1998) A limited renal injury may cause a permanent form of neurogenic hypertension. Am J Hypertens 11:723–728
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler M (2009) Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373:1275–1281
Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Bohm M (2010) Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 376:1903–1909
Symplicity HTN-1 Investigators (2011) Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension 57:911–917
Li LP, Halter S, Prasad PV (2008) Blood oxygen level-dependent MR imaging of the kidneys. Magn Reson Imaging Clin N Am 16:613–625
Heyman SN, Khamaisi M, Rosen S, Rosenberger C (2008) Renal parenchymal hypoxia, hypoxia response and the progression of chronic kidney disease. Am J Nephrol 28:998–1006
Verloop WL, Vink EE, Voskuil M, Vonken EJ, Rookmaaker MB, Bots ML, Doevendans PA, Blankestijn PJ, Spiering W (2013) Eligibility for percutaneous renal denervation: the importance of a systematic screening. J Hypertens 31:1662–1668
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, Young WF Jr, Montori VM (2008) Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 93:3266–3281
Shionoiri H, Yasuda G, Yoshimura H, Umemura S, Miyajima E, Miyakawa T, Takagi N, Kaneko Y (1987) Antihypertensive effects and pharmacokinetics of single and consecutive administration of doxazosin in patients with mild to moderate essential hypertension. J Cardiovasc Pharmacol 10:90–95
Ebrahimi B, Gloviczki M, Woollard JR, Crane JA, Textor SC, Lerman LO (2012) Compartmental analysis of renal BOLD MRI data: introduction and validation. Invest Radiol 47:175–182
Schlaich MP, Sobotka PA, Krum H, Lambert E, Esler MD (2009) Renal sympathetic-nerve ablation for uncontrolled hypertension. N Engl J Med 361:932–934
Worthley SG, Tsioufis CP, Worthley MI, Sinhal A, Chew DP, Meredith IT, Malaiapan Y, Papademetriou V (2013) Safety and efficacy of a multi-electrode renal sympathetic denervation system in resistant hypertension: the EnligHTN I trial. Eur Heart J 34:2132–2140
Ormiston JA, Watson T, Van PN, Stewart R, Haworth P, Stewart JT, Webster MW (2013) First-in-human use of the OneShot renal denervation system from Covidien. EuroIntervention 8:1090–1094
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, Kusek JW, Eggers P, Van LF, Greene T, Coresh J (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Ott C, Janka R, Schmid A, Titze S, Ditting T, Sobotka PA, Veelken R, Uder M, Schmieder RE (2013) Vascular and Renal Hemodynamic Changes after Renal Denervation. Clin J Am Soc Nephrol
Mahfoud F, Cremers B, Janker J, Link B, Vonend O, Ukena C, Linz D, Schmieder R, Rump LC, Kindermann I, Sobotka PA, Krum H, Scheller B, Schlaich M, Laufs U, Bohm M (2012) Renal Hemodynamics and Renal Function After Catheter-Based Renal Sympathetic Denervation in Patients With Resistant Hypertension. Hypertension
Prasad PV (2006) Evaluation of intra-renal oxygenation by BOLD MRI. Nephron Clin Pract 103:c58–c65
Waeber B, Brunner HR (1999) Clinical value of ambulatory blood pressure monitoring in the assessment of antihypertensive therapy. Blood Press Monit 4:263–266
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De BG, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F (2013) 2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31:1281–1357
Mahfoud F, Ukena C, Schmieder RE, Cremers B, Rump LC, Vonend O, Weil J, Schmidt M, Hoppe UC, Zeller T, Bauer A, Ott C, Blessing E, Sobotka PA, Krum H, Schlaich M, Esler M, Bohm M (2013) Ambulatory blood pressure changes after renal sympathetic denervation in patients with resistant hypertension. Circulation 128:132–140
Gloviczki ML, Glockner JF, Lerman LO, McKusick MA, Misra S, Grande JP, Textor SC (2010) Preserved oxygenation despite reduced blood flow in poststenotic kidneys in human atherosclerotic renal artery stenosis. Hypertension 55:961–966
Textor SC, Glockner JF, Lerman LO, Misra S, McKusick MA, Riederer SJ, Grande JP, Gomez SI, Romero JC (2008) The use of magnetic resonance to evaluate tissue oxygenation in renal artery stenosis. J Am Soc Nephrol 19:780–788
Epstein FH, Prasad P (2000) Effects of furosemide on medullary oxygenation in younger and older subjects. Kidney Int 57:2080–2083
Djamali A, Sadowski EA, Muehrer RJ, Reese S, Smavatkul C, Vidyasagar A, Fain SB, Lipscomb RC, Hullett DH, Samaniego-Picota M, Grist TM, Becker BN (2007) BOLD-MRI assessment of intrarenal oxygenation and oxidative stress in patients with chronic kidney allograft dysfunction. Am. J. Physiol Renal Physiol 292:F513–F522
Siddiqi L, Hoogduin H, Visser F, Leiner T, Mali WP, Blankestijn PJ (2014) Inhibition of the renin-angiotensin system affects kidney tissue oxygenation evaluated by magnetic resonance imaging in patients with chronic kidney disease. J Clin Hypertens 16:214–218
Acknowledgments
The scientific guarantor of this publication is Peter Blankestijn. The authors of this manuscript declare relationships with the following companies: MV has received consultancy fees of Medtronic Inc. PJB has received unrestricted research grants of Medtronic Inc., and speaker and consultancy fees of Medtronic Inc. and St. Jude Medical Inc. EEV was supported by a grant of the Dutch Kidney Foundation (IP10-15). No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Appendix 2
Bland Altman plot.

Bland Altman plot.

Bland Altman plot.

Rights and permissions
About this article
Cite this article
Vink, E.E., Boer, A., Verloop, W.L. et al. The effect of renal denervation on kidney oxygenation as determined by BOLD MRI in patients with hypertension. Eur Radiol 25, 1984–1992 (2015). https://doi.org/10.1007/s00330-014-3583-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3583-1