Abstract
Objectives
To compare the average glandular dose (AGD) and diagnostic performance of mediolateral oblique (MLO) digital breast tomosynthesis (DBT) plus cranio-caudal (CC) digital mammography (DM) with two-view DM, and to evaluate the correlation of AGD with breast thickness and density.
Methods
MLO and CC DM and DBT images of both breasts were obtained in 149 subjects. AGDs of DBT and DM per exposure were recorded, and their correlation with breast thickness and density were evaluated. Paired data of MLO DBT plus CC DM and two-view DM were reviewed for presence of malignancy in a jack-knife alternative free-response ROC (JAFROC) method.
Results
The AGDs of both DBT and DM, and differences in AGD between DBT and DM (ΔAGD), were correlated with breast thickness and density. The average JAFROC figure of merit (FOM) was significantly higher on the combined technique than two-view DM (P = 0.005). In dense breasts, the FOM and sensitivity of the combined technique was higher than that of two-view DM (P = 0.003) with small ΔAGD.
Conclusions
MLO DBT plus CC DM provided higher diagnostic performance than two-view DM in dense breasts with a small increase in AGD.
Key Points
• DBT has higher diagnostic performance and potential to overcome limitations of DM.
• Dose differences (DBT-DM, ΔAGD) were inversely correlated with breast thickness and density.
• Figure of merit of MLO-DBT/CC-DM was higher than that of two-view DM.
• In dense breasts, MLO-DBT/CC-DM provides better diagnostic performance with a small AGD increase.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mammography is, at present, the only screening test that has been shown to reduce breast cancer-related mortalities [1–4]. In addition, with the advent of digital mammography (DM), higher accuracy has been achieved in women under the age of 50 years, women with radiographically dense breasts, and premenopausal or perimenopausal women [5]. However, despite its clearly documented benefits, DM does not eliminate a fundamental limitation in detecting non-calcified breast cancers which are obscured by surrounding and overlying dense parenchyma [6–9]. Digital breast tomosynthesis (DBT), which allows partial three-dimensional (3D) reconstruction of breast tissue viewed in sequential sections through the breast, can potentially overcome this inherent limitation of DM caused by overlapping normal and pathological tissue during standard two-dimensional (2D) projections [10–12]. It offers potential advantages in the evaluation of masses, areas of architectural distortion and asymmetries compared with conventional 2D mammographic images. Therefore, unsurprisingly, the benefits of utilising DBT as an adjunct to DM have already been reported in a variety of observer performance studies [13] with two-view DBT outperforming two-view DM, especially for inexperienced readers [14–17].
Several studies [13, 18] have since examined whether single-view DBT could replace standard DM for screening purposes, and earlier studies which compared mediolateral oblique (MLO)-only DBT views with two-view DM reported that DBT alone in one view was confirmed to be equivalent to standard two-view DM [17, 19–21]. In addition, the combined technique of single-view DBT and single-view DM [22, 23] also showed its non- inferiority to two-view DM in the diagnostic setting. Using single view DBT or replacing single view DM with DBT may reduce the radiation dose burden while maintaining or improving diagnostic performances compared with standard two-view DM in clinical practice. Until now, however, although there have been studies comparing the diagnostic performances of single-view DBT or a combined technique with two-view DM [22, 23], there have been no studies comparing their radiation doses in addition to their diagnostic performances. Furthermore, as average glandular dose (AGD) for both DM and DBT increases along with thickness and with glandular fraction in most breasts [24], there may be a specific group of women who can benefit from DBT, and if so, DBT can be selectively performed for these patients to maximise its effect while minimising radiation dose according to the specific considerations of breast density and thickness.
Therefore, in this study, we evaluated the AGD of MLO DM and DBT according to breast density and thickness. In addition, as two-view mammographic examinations are more effective than one-view mammographic examinations [25], we compared the diagnostic performance of the combination of a cranio-caudal (CC) DM view with a single-view DBT (MLO) versus two-view DM.
Materials and methods
Study population
This retrospective study was approved by the institutional review board of Seoul National University Hospital, with waiver of informed consent. Between April and September 2012, we included 179 women (mean age, 51.1 ± 10.5; range, 22-78 years) who were referred to our institution with clinical signs and symptoms of breast cancer or referred for diagnostic work-up, and who showed an abnormality at screening mammography or ultrasound. Among these patients, 24 were excluded due to previous history of breast surgery, and one patient due to history of neoadjuvant chemotherapy. Five patients were additionally excluded as they had multifocal breast cancers in both breasts. Finally, 149 women (median age 50.0 years ± 10.4) were included in this study.
Of these 149 patients, 61 were asymptomatic, 72 presented with palpability, 8 presented with pain, 4 showed nipple discharge and 4 showed nipple retraction. Among them, 68.5 % (102 of 149) of patients had malignancies and others (31.5 %, 47 of 149) were considered to have negative or benign findings. All malignant lesions were confirmed through core-needle biopsy (14-gauge automated gun or 11-gauge vacuum-assisted) with ultrasound (US) or mammography guidance and underwent subsequent surgical excision, including breast conserving surgery (n = 66), modified radical mastectomy (n = 8) or total mastectomy (n = 28). Mean duration of imaging follow-up with mammography for lesions considered to have benign or negative findings was 649 days ± 43.3, and lesion stability was confirmed in all cases.
Image acquisition
DBT was performed in combination with DM by one dedicated technologist using a commercially available device (Selenia Dimensions System; Hologic, Bedford, MA, USA). The device used a custom-designed high-power (mA) tungsten (W) anode X-ray tube and X-ray filters of rhodium (Rh), silver (Ag) and aluminum (Al). Different filters in DBT and full-field DM imaging modes (a 0.7-mm-thick aluminium filter for DBT acquisition and 50-μm thick Rh or Ag filter for DM acquisitions). The X-ray spectra can vary between 20 and 49 kVp based on the thickness/composition of the breast using automatic exposure control (AEC) [26–28]. Both DBT and DM images were obtained in each breast with both CC and MLO projections, and the DBT images were acquired in the same compression sequence as the DM images. AGD per exposure as well as breast thickness measured for MLO DBT and DM were retrieved from the DICOM headers of the images using the automatic exposure settings.
Observer performance study
The database of the patients who underwent both DM and DBT was anonymised, and image sets of standard two-view DM and combined CC DM and MLO DBT were created in random order. Three radiologists (J.M.C., M.S.B. and S.H.L.) from a single academic institution, with 6-11 years of experience in breast imaging and in the interpretation of DBT images for 6 months in clinical practice, reviewed all images. The images were reviewed independently without any information of prior imaging or clinical history. Two separate reading sessions were performed with at least a 3-week interval to minimise any learning bias. Each reading session contained half of standard two-view DM and half of a combination of CC DM and MLO DBT images, randomised and presented in alternating order. All readers were requested to detect the tumours and record the location of each lesion. These identifiers were used to confirm that readers had correctly identified a cancer. After identifying the lesions, the reader then provided a forced Breast Imaging Reporting and Data System (BI-RADS) score of 1, 2, 3, 4, or 5 to indicate the most likely outcome based on the appearance of the finding and also a likelihood of malignancy score ranging from 0 % to 100 % for each case. One radiologist not involved in the readings (S.U.S.) determined whether each finding was a true positive or false positive by cross-checking the true location and identifier with the biopsy or surgery reports. This data set was analysed with jack-knife alternative free-response ROC (JAFROC) methods. Cases in which biopsy or surgery revealed malignant disease were considered positive. Cases with concordant benign biopsy results, as well as women that did not undergo biopsy and had no evidence of breast malignancy after 1 year of clinical follow-up, were considered negative.
Data collection and statistical analysis
The clinical, radiological and histopathological findings of all patients were reviewed. Mammographic breast density was determined according to BI-RADS breast density grading [29] by three radiologists in consensus, and breast thickness and AGD per exposure in MLO views retrieved from DICOM headers were recorded.
Statistical analyses consisted of two parts. First, we examined the correlation between patient variables and the AGD of DBT and DM in MLO views. The relationships of AGD with age, breast thickness and BI-RADS density were compared using Pearson’s correlation for parametric tests, and multiple linear regression analysis with the stepwise selection method was used to determine the relative influence of the different variables on the AGD of DBT and DM. In addition, to investigate the subgroups that most benefitted from DBT compared with DM in radiation dose, we calculated the difference between the AGD of DBT and DM (ΔAGD), and determined the patient factor which correlated with ΔAGD. Multiple linear regression analysis with the stepwise selection method was used to determine the relative influence of the different patient variables on the mean ΔAGD; a significance level of P in < 0.05, P out < 0.20 was established. The intercept term was not significant; thus, the coefficients of independent variables were estimated using multiple linear regression analysis. A P value of less than 0.05 was considered to indicate a significant difference.
Second, we compared the diagnostic performances of two-view DM and the combined technique of CC DM and MLO DBT. JAFROC curves for two-view DM and the combined technique were analysed to evaluate and compare their diagnostic performances using the likelihood of malignancy. Diagnostic sensitivity and specificity were compared, using BI-RADS scores of 4 or 5 considered as positive and BI-RADS scores of 1, 2, or 3 considered as negative [10, 13, 20]. To assess the diagnostic performance in different breast density subsets (fatty breast group versus dense breast group) in correlation with ΔAGD, JAFROC figure of merit (FOM), sensitivity and specificity were calculated separately in each group. Fatty breast represents mammographic breast density of grade 1 and 2. Dense breast represents mammographic breast density of grade 3 and 4. In addition, to assess the correlation of breast thickness with diagnostic performance, we assessed the odds ratios and 95 % confidence intervals for the proportion of positive diagnostic tests on malignant cases, and proportion of negative diagnostic tests on benign cases, according to the breast thickness using logistic regression analysis with generalised estimating equations. These analyses were performed using generalised estimating equation with independent working structure considering cluster effect caused by multiple readers. A P value of less than 0.05 was deemed to indicate a statistical significance. All statistical analyses were performed using SAS systems for windows, version 9.3 (SAS Institute, Cary, NC, USA) and JAFROC (http: //www. devchakraborty.com).
Results
Of 149 patients, histopathological proof was available for 115 lesions, including all breasts with carcinoma (n = 102), and 12 had no lesions. The mean tumour size was 3.11 ± 1.90 cm (range, 0.6-10.0 cm). Malignant histology included 6 ductal carcinomas in situ (DCIS) and 96 invasive ductal carcinomas (IDCs) with or without DCIS. There were 22 patients who had presumed benign lesions without pathology, 13 patients with pathology-proven benign lesions (1 papilloma, 8 fibroadenomas, 1 sclerosing adenosis, 1 columnar cell changes and 2 fibrocystic changes). On DM, 68 lesions presented as masses with or without microcalcifications, 10 as asymmetry, 10 as microcalcifications, 2 as architectural distortions and 12 showed no abnormality.
The distribution of breast tissue densities on DM were as follows: grade 1 in 11 patients, grade 2 in 23 patients, grade 3 in 84 patients and grade 4 in 31 patients. Among the 149 patients, 34 patients had fatty breasts (22.8 %, 34/149) and the other 115 patients had dense breasts (77.2 %, 115/149).
Mean breast thickness measured on MLO views was 4.8 cm ± 1.1. The distribution of breast thickness on both MLO views was as follows: breast thickness on right MLO views ≤2 cm (n = 2), 2-3 cm (n = 9), 3-4 cm (n = 23), 4-5 cm (n = 46), >5 cm (n = 69); breast thickness on left MLO views ≤2 cm (n = 1), 2-3 cm (n = 12), 3-4 cm (n = 20), 4-5 cm (n = 46), >5 cm (n = 70). A tendency toward an inverse correlation was observed between the grade of breast density and mean ages of the patients. As the grade of breast density increased, the mean age of the patients decreased (correlation coefficient = -0.564, P < 0.001). The thickness of the breast also showed an inverse correlation with the grade of breast density (correlation coefficient = -0.302 for MLO thickness, P < 0.001).
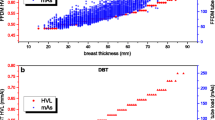
Average glandular dose
Mean AGD of DBT per exposure for both breasts was 1.74 mGy (range, 0.93-5.02 mGy), and that of DM was 1.63 mGy (range, 0.68-7.41 mGy). The mean AGD of DBT was significantly higher than that of DM (P < 0.001). In univarate analysis, breast thickness was significantly associated with AGDs, and both AGDs of DM and DBT increased with increased breast thickness (correlation coefficient = 0.792 and 0.926, respectively, all P < 0.001). Breast density showed inverse correlation with AGDs of DBT breast density (correlation coefficient = -0.175, P = 0.002); however, no correlation was noted with AGD of DM (correlation coefficient = 0.069, P = 0.235). There was a positive correlation in age with the AGD of DBT (correlation coefficient = 0.152, P = 0.009). However, there was no statistically significant correlation between age and AGD of DM (correlation coefficient = -0.018, P = 0.760). Even though there were multiple variables showing significant association with AGD values in univariate analysis, multiple linear regression analysis showed that breast thickness (regression coefficient = 0.041 and 0.052, respectively, all P < 0.001) and density (regression coefficient = 0.072 and 0.308, respectively, all P < 0.001) were independent factors associated with AGD of DBT and DM (Fig. 1).
With regards to ΔAGD, there was a negative correlation between breast thickness and ΔAGD (correlation coefficient = -0.281, P < 0.001), meaning the thicker the breast, the smaller the difference in AGD between DBT and DM. In addition, the ΔAGD in dense breasts was significantly smaller than in fatty breasts (0.037 mGy ± 0.340 vs 0.389 mGy ± 0.245, P < 0.001). Multiple linear regression analysis revealed that breast thickness (regression coefficient: -0.013; P < 0.001) and density (regression coefficient: -0.242; P < 0.001) were independent factors associated with ΔAGD. We found that the thicker and denser the breast tissue, the smaller the ΔAGD, implying that the AGD of DBT is similar to DM or possibly even smaller than DM.
Diagnostic performances
Using a cut-off point between BI-RADS final assessment category 3 and 4, the sensitivities for two-view DM and the combined technique were 79.4 % and 89.2 % for reader 1 (P = 0.003), 85.3 % and 92.2 % for reader 2 (P = 0.035), and 82.3 % and 87.3 % for reader 3 (P = 0.130), respectively (Table 1). The mean sensitivities for the three readers were significantly different between two-view DM and the combined technique (82.4 % vs 89.5 %, P < 0.001). The combined technique identified 21 more cancers than two-view DM by at least one reader, and 11 of the 21 cancers were invasive cancers (Fig. 2). Regarding breast density, the sensitivities for two-view DM and the combined technique in dense breasts were 80.0 % and 89.4 % for reader 1 (P = 0.010), 85.9 % and 92.9 % for reader 2 (P = 0.034) and 83.5 % and 87.1 % for reader 3 (P = 0.316), respectively. The mean sensitivity for the three readers was significantly higher in combined technique (89.8 %, 229/255) than two-view DM (83.1 %, 177/255) (P = 0.004). In fatty breasts, the mean sensitivity of three readers showed significant difference between two-view DM and the combined technique (78.4 % vs 88.2 %, P = 0.004), however, individual sensitivities did not show any statistical significances in any reader (76.5 % vs 88.2 %, P = 0.144; 82.4 % vs 88.2 %, P = 0.564; 76.5 % and 88.2 % P = 0.144).
A 44-year-old woman with a 15-mm grade II infiltrating ductal carcinoma. a, b Right breast: two-view DM (CC and MLO) shows subtle asymmetry in the right inner lower portion. c MLO DBT of the same breast (plane 31 of 55) shows a spiculated mass highly suggestive of malignancy, showing the better capability of DBT in depiction. Breast thickness measured at right MLO view was 51 mm. The AGD value of DM at right MLO view was 2.19 mGy, whereas that of DBT was 1.89 mGy
The specificities for two-view DM and the combined technique were 78.5 % and 58.2 % for reader 1 (P = 0.001), 94.9 % and 86.1 % for reader 2 (P = 0.008), and 62.0 % and 81.0 % for reader 3 (P = 0.001), respectively (Table 2). Results of two readers showed tendencies for decreasing specificity with combined technique, and the other reader showed the opposite tendency. This tendency was also noted in subgroup analysis (fatty versus dense breast). The mean specificities for the three readers were not significantly different between two-view DM and the combined technique (78.5 % vs 75.1 %, P = 0.260).
In JAFROC analysis (Table 3), FOMs using the probability of malignancy (%) for two-view DM and the combined technique were 0.853 and 0.874 (P = 0.29) for reader 1, 0.922 and 0.952 (P = 0.083) for reader 2, and 0.832 and 0.907 (P = 0.002) for reader 3, respectively. The overall FOM for the three readers were 0.869 for two-view DM and 0.911 for the combined technique. This difference was statistically significant (P = 0.005). In dense breasts, the overall FOM of the combined technique was significantly higher than that of two-view DM (0.910 vs 0.863, P = 0.010). However, in fatty breasts, the FOM for two-view DM and the combined technique were not significantly different (0.863 vs 0.908, P = 0.118).
Regarding breast thickness, sensitivity for detection of malignancy increased when breast thickness increased for both the combined technique and two-view DM (OR = 1.03, 95 % CI = 0.99-1.07); however, no statistical significance was noted (P = 0.126). This tendency of increasing sensitivity was higher in the combined technique (OR = 1.04, 95 % CI = 0.99-1.09) than two view DM (OR =1.03, 95 % CI = 0.99-1.07), which was statistically not significant (P = 0.506). The specificity also increased when breast thickness increased for both combined technique and two-view DM (OR = 1.01, 95 % CI = 0.98-1.04), however no statistical significance was noted (P = 0.538). A tendency of higher specificity increment in combined technique (OR = 1.011, 95 % CI = 0.98-1.04) than two view DM (OR = 1.005, 95 % CI = 0.98-1.03) was also noted according to breast thickness, but this was statistically not significant (P = 0.538).
Discussion
In this study, we found that breast thickness and density were independent factors associated with ΔAGD, and ΔAGD was significantly smaller in dense and thick breasts than in fatty and thin breasts. In addition, the combined technique of single-view MLO DBT plus single-view CC DM provided higher diagnostic performance including FOM values and sensitivities than two-view DM, especially in dense breasts. Our results show that the clinical benefit in using the combined technique of single-view DBT and single-view DM not only improves diagnostic performance but also minimises radiation dose increments in patients with dense breasts. In a study by Waldherr et al. [30], better diagnostic performances were reported with one-view DBT than with two-view DM. Another study using the combined technique of single-view DBT and single-view DM [22] also showed its non-inferiority to two-view DM. However, in their study, diagnostic performances were compared without consideration of radiation dose according to patient characteristics. It is well known that AGDs of both DBT and DM increases with thickness and with glandular fraction in most breasts [24]. In our study, we found that AGDs of DBT and DM were higher in dense or thick breasts, in general, ΔAGD were smaller in dense breasts, and in thick breasts. Thus, for dense- or thick-breast patients, we can expect higher diagnostic performance with a small dose difference using MLO DBT instead of MLO DM. It should be noted that these findings are system-specific, and therefore these results may be different for other DBT systems from other manufacturers. However, similar findings were noted in other studies, and for the breast with a thickness of 5 cm and 50 % glandular fraction, the authors found that DBT acquisition results in only an 8 % higher MGD than mammography [31]. In contrast, with another breast phantom of 6 cm thick, 14.3 % glandular fraction, the authors found a larger dose increase of 83 % from mammography to DBT [32].
In a previous study [30], similar to our results, the sensitivity of one-view DBT was observed to be higher than that of two-view DM for dense breasts, in which tissue overlap was a major problem. Furthermore, most additional cancer detections by DBT were invasive cancers [18]. However, in our study, overall specificities were not improved, and two readers even showed lower specificity using the combined technique rather than routine two-view DM. These results are different from those reported in other studies, as in many previous studies, the overall recall rate decreased with the use of DBT information [13, 33–35]. Ideally, the clinical performance of an imaging technique is reputed to be high if it has high sensitivity and, at the same time, high specificity [23]. The lack of improvement in specificity seen in our study can be explained by the fact that the number of benign or normal cases was small in our study, and that our data were enriched with malignant lesions. Further studies with more normal cases are warranted to validate our results.
In our study, AUCs, sensitivities and specificities by each reader were not significantly different in fatty breasts. In most studies [13, 18], the addition of DBT to routine DM improved diagnostic performances even in patients with fatty breasts. It has also been reported that the sensitivity and negative predictive values of single-view DBT were superior to those of DM in fatty breasts [13]. In a study by Gennaro et al. [23], the result showed equivalent performance using the combined technique to standard two-view mammography as in our study. However, in their study, subgroup analysis according to breast density was not performed. Further studies including a greater number of fatty breasts will be necessary to validate these results.
Our study has several limitations. First, this study was a retrospective study and, as in other retrospective studies, the clinical performance observed in retrospective reader studies may be different from the performance in a true clinical context, as readers are aware that they are participating in an “experiment” without the consequences of patient care [36]. Second, reader studies are enriched with malignant lesions, and these results may be different from those of a true screening population. As a result, the tendency among the readers to recall may likely be higher than normally would be observed. Further studies including more normal and benign cases as would be seen in the clinical environment will be critical to confirm the performance of this technique. Third, the number of patients with fatty breasts was relatively small in our study and might be not enough to make statistical differences. Further studies with larger populations are needed to confirm this result. Fourth, we just performed studies on this clinical-proven platform with established techniques, and dose values retrieved from the DICOM header were not verified. The issue of dose optimisation for lesion detection or characterisation in DBT remains, even though this is beyond our scope. Lastly, prior imaging studies were not available to the readers to assist them in making their assessments.
In conclusion, even though the mean AGD of DBT was higher than that of DM, the difference in AGD between single-view MLO DBT and DM showed an inverse correlation between breast thickness and density. In addition, the overall AUC of single-view MLO DBT plus single-view CC DM was higher than that of two-view DM. Particularly in dense breast patients, single-view MLO DBT plus single-view CC DM may provide better diagnostic performance with a minimal increase in AGD.
Abbreviations
- AGD:
-
Average glandular dose
- CC:
-
Cranio-caudal
- DBT:
-
Digital breast tomosynthesis
- DM:
-
Digital mammography
- FOM:
-
Figure of merit
- JAFROC:
-
Jack-knife alternative free-response receiver operating characteristic
- MLO:
-
Mediolateral oblique
References
Berry DA, Cronin KA, Plevritis SK et al (2005) Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353:1784–1792
Hellquist BN, Duffy SW, Abdsaleh S et al (2011) Effectiveness of population-based service screening with mammography for women ages 40 to 49 years: evaluation of the Swedish Mammography Screening in Young Women (SCRY) cohort. Cancer 117:714–722
Tabar L, Fagerberg CJ, Gad A et al (1985) Reduction in mortality from breast cancer after mass screening with mammography. Randomised trial from the Breast Cancer Screening Working Group of the Swedish National Board of Health and Welfare. Lancet 1:829–832
Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW (2003) Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet 361:1405–1410
Pisano ED, Gatsonis C, Hendrick E et al (2005) Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med 353:1773–1783
Carney PA, Miglioretti DL, Yankaskas BC et al (2003) Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med 138:168–175
Boyd NF, Guo H, Martin LJ et al (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356:227–236
Mandelson MT, Oestreicher N, Porter PL et al (2000) Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst 92:1081–1087
Kerlikowske K, Grady D, Barclay J, Sickles EA, Ernster V (1996) Effect of age, breast density, and family history on the sensitivity of first screening mammography. JAMA 276:33–38
Noroozian M, Hadjiiski L, Rahnama-Moghadam S et al (2012) Digital breast tomosynthesis is comparable to mammographic spot views for mass characterization. Radiology 262:61–68
Tagliafico A, Astengo D, Cavagnetto F et al (2012) One-to-one comparison between digital spot compression view and digital breast tomosynthesis. Eur Radiol 22:539–544
Tagliafico A, Tagliafico G, Astengo D et al (2012) Mammographic density estimation: one-to-one comparison of digital mammography and digital breast tomosynthesis using fully automated software. Eur Radiol 22:1265–1270
Rafferty EA, Park JM, Philpotts LE et al (2013) Assessing radiologist performance using combined digital mammography and breast tomosynthesis compared with digital mammography alone: results of a multicenter, multireader trial. Radiology 266:104–113
Gur D, Bandos AI, Rockette HE et al (2011) Localized detection and classification of abnormalities on FFDM and tomosynthesis examinations rated under an FROC paradigm. AJR Am J Roentgenol 196:737–741
Svahn T, Andersson I, Chakraborty D et al (2010) The diagnostic accuracy of dual-view digital mammography, single-view breast tomosynthesis and a dual-view combination of breast tomosynthesis and digital mammography in a free-response observer performance study. Radiat Prot Dosim 139:113–117
Michell MJ, Iqbal A, Wasan RK et al (2012) A comparison of the accuracy of film-screen mammography, full-field digital mammography, and digital breast tomosynthesis. Clin Radiol 67:976–981
Wallis MG, Moa E, Zanca F, Leifland K, Danielsson M (2012) Two-view and single-view tomosynthesis versus full-field digital mammography: high-resolution X-ray imaging observer study. Radiology 262:788–796
Skaane P, Bandos AI, Gullien R et al (2013) Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology 267:47–56
Teertstra HJ, Loo CE, van den Bosch MA et al (2010) Breast tomosynthesis in clinical practice: initial results. Eur Radiol 20:16–24
Gennaro G, Toledano A, di Maggio C et al (2010) Digital breast tomosynthesis versus digital mammography: a clinical performance study. Eur Radiol 20:1545–1553
Svahn TM, Chakraborty DP, Ikeda D et al (2012) Breast tomosynthesis and digital mammography: a comparison of diagnostic accuracy. Br J Radiol 85:e1074–e1082
Gennaro G, Hendrick RE, Toledano A et al (2013) Combination of one-view digital breast tomosynthesis with one-view digital mammography versus standard two-view digital mammography: per lesion analysis. Eur Radiol 23:2087–2094
Gennaro G, Hendrick RE, Ruppel P et al (2013) Performance comparison of single-view digital breast tomosynthesis plus single-view digital mammography with two-view digital mammography. Eur Radiol 23:664–672
Feng SS, Sechopoulos I (2012) Clinical digital breast tomosynthesis system: dosimetric characterization. Radiology 263:35–42
Hackshaw AK, Wald NJ, Michell MJ, Field S, Wilson AR (2000) An investigation into why two-view mammography is better than one-view in breast cancer screening. Clin Radiol 55:454–458
Ranger NT, Lo JY, Samei E (2010) A technique optimization protocol and the potential for dose reduction in digital mammography. Med Phys 37:962–969
Dance DR, Thilander AK, Sandborg M, Skinner CL, Castellano IA, Carlsson GA (2000) Influence of anode/filter material and tube potential on contrast, signal-to-noise ratio and average absorbed dose in mammography: a Monte Carlo study. Br J Radiol 73:1056–1067
Ren B, Ruth C, Wu T et al (2010) A new generation FFDM/tomosynthesis fusion system with selenium detector. Proc SPIE 7622:76220B–76211
D’Orsi CJ, Sickles EA, Mendelson EB et al (2013) ACR BI-RADS® Atlas, breast imaging reporting and data system. American College of Radiology, Reston
Waldherr C, Cerny P, Altermatt HJ et al (2013) Value of one-view breast tomosynthesis versus two-view mammography in diagnostic workup of women with clinical signs and symptoms and in women recalled from screening. AJR Am J Roentgenol 200:226–231
Hendrick RE, Pisano ED, Averbukh A et al (2010) Comparison of acquisition parameters and breast dose in digital mammography and screen-film mammography in the American College of Radiology Imaging Network digital mammographic imaging screening trial. AJR Am J Roentgenol 194:362–369
Yaffe MJ, Boone JM, Packard N et al (2009) The myth of the 50-50 breast. Med Phys 36:5437–5443
Haas BM, Kalra V, Geisel J, Raghu M, Durand M, Philpotts LE (2013) Comparison of tomosynthesis plus digital mammography and digital mammography alone for breast cancer screening. Radiology 269:694–700
Rose SL, Tidwell AL, Bujnoch LJ, Kushwaha AC, Nordmann AS, Sexton R Jr (2013) Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol 200:1401–1408
Bernardi D, Ciatto S, Pellegrini M et al (2012) Prospective study of breast tomosynthesis as a triage to assessment in screening. Breast Cancer Res Treat 133:267–271
Gur D, Bandos AI, Cohen CS et al (2008) The “laboratory” effect: comparing radiologists’ performance and variability during prospective clinical and laboratory mammography interpretations. Radiology 249:47–53
Acknowledgments
The scientific guarantor of this publication is Woo Kyung Moon. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This research was supported by the Seoul National University Hospital Research Fund (grant 06-2012-0780), and the Core Medical Device R & D Program (10043122) funded by the Ministry of Trade, Industry & Energy (MOTIE), Korea. The authors would also like to thank Chris Woo, B.A. for his kind assistance in editing this manuscript and appreciate the statistical advice given by the Medical Research Collaborating Centre at Seoul National University Hospital and the Seoul National University College of Medicine. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. This study is retrospective diagnostic study performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shin, S.U., Chang, J.M., Bae, M.S. et al. Comparative evaluation of average glandular dose and breast cancer detection between single-view digital breast tomosynthesis (DBT) plus single-view digital mammography (DM) and two-view DM: correlation with breast thickness and density. Eur Radiol 25, 1–8 (2015). https://doi.org/10.1007/s00330-014-3399-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3399-z