Abstract
Objective
To evaluate the role of core-needle biopsy (CNB) by comparing the results of CNB and repeated fine-needle aspiration (FNA) for thyroid nodules with initially non-diagnostic FNA results.
Methods
From October 2008 to December 2011, 360 nodules – 180 consecutive repeated FNAs and 180 consecutive CNBs –– from 360 patients (83 men, 277 women; mean age, 54.4 years) with initially non-diagnostic FNA results were analyzed retrospectively. The incidence of non-diagnostic results, inconclusive results, diagnostic surgery, and diagnostic performance of repeated FNA and CNB were assessed, and factors affecting second non-diagnostic results were evaluated.
Results
CNB achieved a significantly lower non-diagnostic and inconclusive rate than repeated FNA (1.1 % versus 40.0 %, P < 0.001; 7.2 % versus 72.0 %, P < 0.001). All diagnostic performances with CNB were higher than repeated FNA. The diagnostic surgery rate was lower with CNB than with repeated FNA (3.6 % versus 16.7 %, P = 0.047). Multivariate logistic regression analysis showed that repeated FNA was the most important factor for second non-diagnostic results (OR = 56.06, P < 0.001), followed by nodules with rim calcification (OR = 7.46, P = 0.003).
Conclusions
CNB is more useful than repeated FNA for reducing the number of non-diagnostic and inconclusive results and for preventing unnecessary diagnostic surgery for thyroid nodules with initially non-diagnostic FNA results.
Key Points
• Core-needle biopsy achieved a lower number of non-diagnostic and inconclusive results.
• Core-needle biopsy achieved better diagnostic performance.
• Use of core-needle biopsy could prevent unnecessary diagnostic surgery.
• Repeated fine-needle aspiration was significantly associated with a second non-diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
US-guided FNA is a widely accepted diagnostic technique for the evaluation of thyroid nodules. However, several previous studies have reported that a major limitation of US-guided FNA is non-diagnostic results [1]. Nonetheless, despite the 17–47 % repeat non-diagnostic result rate [1–4], current guidelines recommended repeated FNA for any nodule with initially non-diagnostic results [5–8]. Current guidelines also recommend diagnostic surgery for nodules with repeated non-diagnostic results [5].
CNB has been suggested as an alternative diagnostic technique for the diagnosis of thyroid nodules [7, 9–13]. While CNB may not always be technically feasible and requires local anaesthesia and more clinical experience in thyroid intervention [14], it is known to be safe, well-tolerated, and associated with a low incidence of complications. Several recent studies have reported that CNB may be a successful alternative to repeated FNA for thyroid nodules with initially non-diagnostic FNA results. However, these study populations were relatively small [10] or there was a lack of control groups [15, 16].
Our study evaluated the role of CNB by comparing the results of CNB and repeated FNA for thyroid nodules with initially non-diagnostic FNA results in a large population.
Materials and methods
Patients
This retrospective study was approved by the institutional review board of our hospital. The requirement for informed consent was waived as we retrospectively used data that was available in our electronic medical records. However, informed consent for FNA or CNB was obtained from all patients prior to their biopsy.
From October 2008 to December 2011, 20,278 US-guided FNAs were performed at our institution, and the cytological results of 3,407 (16.8 %) procedures were non-diagnostic. Among the 3,407 procedures with initially non-diagnostic FNA results, we included 180 CNB procedures (from October 2008 to December 2011) and 180 consecutive repeated FNA procedures (from October 2008 to July 2011) after the initially non-diagnostic FNA results (Fig. 1). Because most patients with non-diagnostic FNA results did not undergo a second US-guided FNA or CNB, and had clinical follow-ups without repeated FNA or CNB, we excluded patients without a second US-guided FNA or CNB, and we ultimately included 360 nodules from 360 patients. The study included 83 men (mean age, 53.3 years; age range, 20–76 years) and 277 women (mean age, 54.7 years; age range, 22–79 years), with a mean age of 54.4 years (age range, 20–79 years).
A final diagnosis was made in 268 of the 360 thyroid nodules. A malignant final diagnosis was made when malignancy was confirmed on the surgical specimen (n = 72, 26.9 %). A final diagnosis of benign nodule was made in 196 nodules (73.1 %) when one of the following parameters was met: 1) surgical specimen (n = 14, 5.2 %); 2) benign cytology findings on repeated FNA and/or CNB procedures were confirmed at least twice (n = 21, 7.8 %); 3) benign cytology findings on the FNA or CNB procedure were confirmed, with a stable size seen at follow-up (n = 93, 34.7 %); and 4) a nodule was stable in size for at least one year (n = 68, 25.4 %) [10, 16] (Fig. 1).
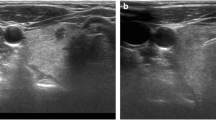
US-guided FNA and CNB procedures
US examinations were performed using one of three US systems: iU22 or HDI 5000 unit (Philips Healthcare, Bothell, WA, USA) or EUB-7500 unit (Hitachi Medical Systems, Tokyo, Japan). In all cases, a comprehensive US evaluation of the neck and thyroid gland was performed, and the size, location, composition, and vascularity of nodules were evaluated. FNA and CNB procedures were performed by two clinically experienced thyroid radiologists (J.H.B. and J.H.L.), with 16 and 11 years of thyroid US experience, or by residents and fellows under their supervision. Either US-guided FNA or CNB was utilized based upon the ultrasound operator’s decision, without definite indications for selection.
For FNA, a 23-gauge needle was routinely used. A 21-gauge needle was chosen for aspiration when a nodule had a large cystic portion and for second-needle passage when the first-needle passage failed due to severe nodule stiffness [14]. Either capillary or aspiration technique (but not both) was used according to the characteristics of each nodule [14]. Due to the retrospective study design, it was impossible to assess which gauge capillary or aspiration biopsies were used for each FNA procedure. Direct smears were made in all cases, and all smears were immediately fixed with alcohol after FNA and were stained with Papanicolaou. The number of needle passes was determined by the operator during the FNA procedure, and a maximum of four needle passes were permitted for each nodule. Additional FNAs were recommended in the case of incomplete results of visual assessment, according to our unpublished data.
For CNB, the biopsy procedures were performed using a 1.1-c, or 1.6-cm excursion, 18-gauge, double-action spring-activated needle (TSK Ace-cut; Create Medic, Yokohama, Japan) [10, 13, 16]. Before insertion of the core needle, we measured the longest diameter of the nodule and used power Doppler US to carefully evaluate the vessels along the approach route in order to avoid haemorrhage. After induction of local anaesthesia with 1 % lidocaine at the needle puncture site, the end of the biopsy needle was advanced into the solid part of the nodule using a free-hand technique (without an US transducer probe). After the tip of the biopsy needle had been advanced into the edge of the nodule, we re-evaluated the vessels around the nodule so as to minimize possible vessel injury. After measuring the distance of fire (1.1 or 1.6 cm), the stylet and cutting cannula of the needle were sequentially fired. Tissue cores were placed in 10 % buffered formalin immediately after the procedure and were then conventionally processed [16].
The adequacy of the procedure was assessed using real-time US imaging, and the adequacy of the specimens was assessed using visual inspection, classifying them into two groups: insufficient (fewer than six particles) or sufficient group (more than six visible particles). The insufficient group was re-aspirated. In order to be considered adequate, all negative smears had to contain at least six groups of epithelial cells, with 10 cells per group, in FNA and had to contain any identifiable thyroid tissue in CNB [10, 16]. Additional FNA or CNB procedures were performed when the lesion was considered inaccurately targeted in the case of small nodules or when an insufficient specimen was suspected by visual inspection [16]. The mean number of specimens obtained with CNB was 1.3 (one time, 136 nodules; two times, 43 nodules; three times, one nodule).
After the biopsy, each patient was observed using a firm local compression of the biopsy site for 10–20 minutes. When the patient complained of pain or swelling of the neck, a repeat US examination was performed to evaluate the complications [16].
Cytology and histology analysis
FNA cytology and CNB histology specimens were reviewed by an experienced pathologist. FNA cytology diagnoses were categorized into six categories according to the Bethesda System for Reporting Thyroid Cytopathology [10, 16, 17]: non-diagnostic, benign, AUS/FLUS, FN/SFN, suspicious for malignancy, and malignant. Because the diagnostic criteria for CNB have not been standardized for thyroid nodules, CNB histology diagnoses were categorized into the same six categories of the Bethesda System according to the histopathology results of CNB in this study [10, 13, 16]. A non-diagnostic CNB reading included the absence of any identifiable follicular thyroid tissue, the presence of only normal thyroid gland, or tissue containing only a few follicular cells insufficient for diagnosis. The benign CNB findings included colloid nodules, nodular hyperplasia, and lymphocytic thyroiditis. The AUS/FLUS reading for CNB included nodules in which some atypical cells were present but were not diagnostic of suspicious malignancy or malignant tumor, and included cellular follicular nodules in which a distinction between follicular neoplasm and hypercellular hyperplastic nodule was not possible. The FN/SFN reading for CNB included nodules with histology features favouring follicular neoplasm. The suspicious-for-malignancy CNB finding was considered when the specimen showed atypia but there was insufficient evidence for a definite diagnosis of malignancy. The malignant CNB finding was considered when the specimen showed unequivocal features of cancer.
Analysis of the US findings
US images were independently reviewed retrospectively by two radiologists (J.H.B. and S.H.C.). Neither reviewer had any information regarding a patient’s clinical history, previous imaging results, or histological results. Any diagnostic discrepancies between the two reviewers were resolved by consensus.
The US findings for nodules were evaluated for the following features [8, 18–20]: size (maximal diameter); internal composition (solid, predominantly solid, predominantly cystic, or cystic); shape (oval to round, taller than wide, or irregular); margins (smooth, spiculated, or ill-defined); echogenicity (isoechoic, hypoechoic, markedly hypoechoic, or hyperechoic); and the presence of calcification (microcalcification, incomplete macrocalcification, complete macrocalcification, or rim calcification). The relationship between the final diagnosis and the malignant US findings was then assessed. The US criteria for malignant nodules were a taller-than-wide shape, spiculated margin, marked hypoechogenicity, and the presence of micro- or macrocalcification [8, 18, 19, 21].
Statistical analysis
The rates of the non-diagnostic and inconclusive results of FNA and CNB were calculated and compared. An inconclusive diagnosis was defined as FNA or CNB results showing non-diagnostic or AUS/FLUS findings.
The sensitivity, specificity, positive predictive value, and negative predictive value of repeated FNA and CNB for the diagnosis of thyroid malignancy and the overall diagnostic accuracy, respectively, were calculated.
To determine the independent risk factors associated with second non-diagnostic results (defined as non-diagnostic results of repeated FNA and CNB), the results of 180 CNB procedures and 180 consecutive repeated FNA procedures after initial non-diagnostic FNA results were divided into two groups, the diagnostic group and the non-diagnostic group. The parameters of the two groups were compared by univariate analysis with the Student’s t tests used for numerical values and Fisher’s exact tests for categorical values. Subsequently, the parameters that were found to be significantly different were evaluated using multivariate logistic regression analysis to determine any independent risk factors. A P value of <0.05 was considered statistically significant. Statistical analysis was performed using statistical software (SPSS, version 11.0; SPSS; Chicago, IL, USA).
Results
In all patients, FNA and CNB procedures were well-tolerated and were completely performed. The mean size of the 360 nodules was 13.3 mm (range, 2–83 mm). The mean size of the 180 nodules in repeated FNA and CNB was 12.8 mm (range, 2–52 mm) and 13.9 mm (range, 3–83 mm), respectively, and therefore without significant difference (P = 0.355).
Diagnostic performance of repeated FNA and CNB
The diagnostic results of repeated FNA (n = 180) and CNB (n = 180) along with the final diagnoses (n = 268) are summarized in Table 1. Final diagnoses were obtained in 140 of 180 nodules (77.8 %) with repeated FNA and in 128 of 180 nodules (71.1 %) with CNB. The incidence of non-diagnostic results for repeated FNA was higher than that for CNB (40.0 % versus 1.1 %, P < 0.001). Inconclusive results were significantly lower in CNB than in repeated FNA (7.2 % versus 72.0 %, P< 0.001).
The diagnostic outcomes of repeated FNA and CNB are summarized in Table 2. All statistical measures for the diagnosis of malignancy, including sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy, were higher with CNB than those in repeated FNA.
Risk factors associated with second non-diagnostic results
Among the 360 initially non-diagnostic thyroid nodules, a second non-diagnostic result was obtained in 74 nodules. The results of the univariate analyses for risk factors associated with second non-diagnostic results are shown in Table 3. The percentage of the nodule size <1.0 cm in the diagnostic group (44.8 %) was lower than that in the non-diagnostic group (48.6 %), although this result was not significantly significant (P = 0.549). However, there were four significant risk factors associated with second non-diagnostic results: age ≥55 years (P = 0.017), final benign diagnosis (P = 0.001), repeated FNA (P < 0.001), and nodules with a taller-than-wide shape (P = 0.031). No significant differences between the two groups were noted for sex, nodular composition, margin, echogenicity, or calcification.
According to the multivariate logistic regression analysis, repeated FNA (OR = 56.06, P < 0.001), nodules with rim calcification (OR = 7.46, P = 0.003), a final benign diagnosis (odds ratio [OR] = 5.52, P = 0.004), and nodules with a taller-than-wide shape (OR = 6.41, P = 0.004) were independent risk factors associated with second non-diagnostic results (Table 4).
Comparison of diagnostic surgery after FNA and CNB
Figure 2 shows the final diagnosis of FNA and CNB and the reasons for surgery, including diagnostic surgery. In the 268 nodules with a final diagnosis, 196 (73.1 %) were benign and 72 (26.9 %) were malignant. Among them, surgery was performed in 86 nodules (14 benign and 72 malignant).
Surgery was performed in 30 nodules after repeated FNA and in 56 nodules after CNB. The reasons for surgery according to the repeated FNA and CNB results are shown in Fig. 2.
Diagnostic surgery was performed in five of 30 nodules (16.7 %) after repeated FNA and in two of 56 nodules after CNB (3.6 %). The reason for diagnostic surgery in the repeated FNA group (n = 30) was image-pathology discordance in all cases (n = 5), and in the CNB group (n = 56) the reason was image-pathology discordance in all cases (n = 2) as well. Although diagnostic surgery was necessary following FNA or CNB in only a small number of patients (1.9 %, 7 of 360), the rate of diagnostic surgery was significantly higher for repeated FNA than for CNB (16.7 % versus 3.6 %, P = 0.047). The surgical diagnoses of seven patients who underwent diagnostic surgery based on their FNA/CNB results are summarized in Table 5. Two nodules with benign CNB results showed concordant final benign pathologies.
Complications
There were no major complications in either the repeated FNA or the CNB group, and no patients required hospital admission or intervention. Symptoms were relieved by manual compression for one hour.
Discussion
Our study demonstrated that CNB achieved significantly lower non-diagnostic and inconclusive rates than repeated FNA for the thyroid nodules with initially non-diagnostic FNA results (1.1 % versus 40.0 %, P < 0.001; 7.2 % versus 72.0 %, P < 0.001). The rate of diagnostic surgery was also lower in CNB than repeated FNA (3.6 % versus 16.7 %, P = 0.047). Factors associated with non-diagnostic results were repeated FNA (OR = 56.06), a final benign diagnosis (OR = 5.52), taller-than-wide shape (OR = 6.41), and rim calcification (OR = 7.46). Repeated FNA was the most significant factor for second non-diagnostic biopsy results. These results suggest that CNB can be utilized rather than repeated FNA as the subsequent diagnostic approach for thyroid nodules with initially non-diagnostic FNA results.
Previous studies have investigated the feasibility of CNB as an alternative to repeated FNA, with non-diagnostic rates of CNB ranging from 1.3 % to 23.3 % [12, 15, 16]. Similarly, in our study, CNB demonstrated a 1.1 % rate of non-diagnostic results. CNB in our study effectively reduced non-diagnostic (1.1 % versus 40.0 %) and inconclusive (7.2 % versus 72.0 %) results compared with those of repeated FNA, similarly to those of a previous study (1.6 % versus 28.1 %; 12.5 % versus 45.3 %) [10]. CNB has been known to reduce non-diagnostic [10, 12, 15, 16] and inconclusive results [13, 22, 23] in other studies as well.
Our large-population study (n = 360) demonstrated higher diagnostic performance with CNB for thyroid malignancy compared with repeated FNA. The diagnostic accuracy of CNB was better than that of repeated FNA (98.4 % versus 60.0 %), and the diagnostic performance of CNB was comparable to that seen in previous studies [10, 16]. This is illustrated primarily in the lower non-diagnostic and inconclusive results in CNB than those in FNA.
In several previous studies, thyroid nodules with a predominantly cystic portion, small size, hypoechogenicity, and macrocalcification have been identified as independent factors affecting non-diagnostic FNA results [24–26]. However, there have been few studies with regard to the risk factors associated with second non-diagnostic results as compared to the initially non-diagnostic FNA results. In our study, repeated FNA was the most significant risk factor affecting the second non-diagnostic results. CNB can be effective in minimizing non-diagnostic results as it provides a larger tissue sample and can assess the histological architecture [10, 14]. Nodules with rim calcification also were associated with a significantly higher risk for non-diagnostic results than nodules with no calcification. Severe calcification could impede the ability to obtain sufficient tissue. Other factors such as final benign diagnosis and nodules with a taller-than-wide shape were also of significant importance.
The current guidelines recommend diagnostic surgery as a method for the management of solid nodules with repeated non-diagnostic results [5, 6]. Reported diagnostic surgery rates range from 22.2 % to 94.7 % [4, 27–29]. Several studies have suggested that CNB reduces the need for diagnostic surgery [12, 16, 30], with rates of diagnostic surgery rate for CNB ranging from 4.4 % to 8.4 % [12, 16]. In our study, although diagnostic surgery was necessary following FNA or CNB in only a small number of patients (1.9 %), the rate was higher in repeated FNA than in CNB (16.7 % versus 3.6 %), which is similar to that of previous CNB studies, and suggesting that CNB could minimize the need for diagnostic surgery.
In conclusion, we found that the use of CNB was effective in reducing non-diagnostic and inconclusive results while preventing unnecessary diagnostic surgery in patients with initially non-diagnostic FNA results. Furthermore, repeated FNA was shown to be the most significant risk factor with regard to second non-diagnostic results. Therefore, CNB rather than repeated FNA may be a useful diagnostic tool for patients with initially non-diagnostic FNA results.
Abbreviations
- US:
-
ultrasound
- FNA:
-
fine-needle aspiration
- CNB:
-
core-needle biopsy
- AUS:
-
atypia of undetermined significance
- FLUS:
-
follicular lesion of undetermined significance
- FN:
-
follicular neoplasm
- SFN:
-
suspected follicular neoplasm
References
Yassa L, Cibas ES, Benson CB, Frates MC, Doubilet PM, Gawande AA, Moore FD, Kim BW, Nose V, Marqusee E, Larsen PR, Alexander EK (2007) Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 111:508–516
Alexander EK, Heering JP, Benson CB, Frates MC, Doubilet PM, Cibas ES, Marqusee E (2002) Assessment of nondiagnostic ultrasound-guided fine needle aspirations of thyroid nodules. J Clin Endocrinol Metab 87:4924–4927
Yang J, Schnadig V, Logrono R, Wasserman PG (2007) Fine-needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer 111:306–315
Orija IB, Pineyro M, Biscotti C, Reddy SS, Hamrahian AH (2008) Value of repeating a nondiagnostic thyroid fine-needle aspiration biopsy. Endocr Pract 13:735–742
Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedus L, Vitti P (2010) American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules. Endocr Pract 16:1–43
Cooper DS, Doherty GM, Haugen BR, Hauger BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Baloch ZW, Cibas ES, Clark DP, Layfield LJ, Ljung BM, Pitman MB, Abati A (2008) The National Cancer Institute Thyroid fine needle aspiration state of the science conference: a summation. Cytojournal 5:6
Moon WJ, Baek JH, Jung SL, Kim DW, Kim EK, Kim JY, Kwak JY, Lee JH, Lee JH, Lee YH, Na DG, Park JS, Park SW (2011) Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J Radiol 12:1–14
Ha EJ, Baek JH, Lee JH, Song DE, Kim JK, Shong YK, Hong SJ (2013) Sonographically suspicious thyroid nodules with initially benign cytologic results: the role of a core needle biopsy. Thyroid 23:703–708
Na DG, Kim JH, Sung JY, Baek JH, Jung KC, Lee H, Yoo H (2012) Core–needle biopsy is more useful than repeat fine-needle aspiration in thyroid nodules read as nondiagnostic or atypia of undetermined significance by the bethesda system for reporting thyroid cytopathology. Thyroid 22:468–475
Renshaw AA, Pinnar N (2007) Comparison of thyroid fine-needle aspiration and core needle biopsy. Am J Clin Pathol 128:370–374
Screaton NJ, Berman LH, Grant JW (2003) US-guided core-needle biopsy of the thyroid gland. Radiology 226:827–832
Choi YJ, Baek JH, Ha EJ, Lim HK, Lee JH, Kim JK, Song DE, Shong Y, Hong SJ (2013) Different risk of malignancy and management recommendations in subcategories of thyroid nodules with atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS): the role of US-guided core-needle biopsy (CNB). Thyroid
Sung JY, Na DG, Kim KS, Yoo H, Lee H, Kim JH, Baek JH (2012) Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur Radiol 22:1564–1572
Samir AE, Vij A, Seale MK, Desai G, Halpern E, Faquin WC, Parangi S, Hahn PF, Daniels GH (2012) Ultrasound-guided percutaneous thyroid nodule core biopsy: clinical utility in patients with prior nondiagnostic fine-needle aspirate. Thyroid 22:461–467
Yeon JS, Baek JH, Lim HK, Ha EJ, Kim JK, Song DE, Kim TY, Lee JH (2013) Thyroid nodules with initially nondiagnostic cytologic results: the role of core-needle biopsy. Radiology 268:274–280
Cibas ES, Ali SZ (2009) The Bethesda System for Reporting Thyroid Cytopathology. Thyroid 19:1159–1165
Kwak JY, Jung I, Baek JH, Baek SM, Choi N, Choi YJ, Jung SL, Kim EK, Kim JA, Kim JH, Kim KS, Lee JH, Moon HJ, Moon WJ, Park JS, Ryu JH, Shin JH, Son EJ, Sung JY, Na DG (2013) Image reporting and characterization system for ultrasound features of thyroid nodules: multicentric korean retrospective study. Korean J Radiol 14:110–117
Moon WJ, Jung SL, Lee JH, Na DG, Baek J-H, Lee YH, Kim J, Kim HS, Byun JS, Lee DH (2008) Benign and malignant thyroid nodules: US differentiation–multicenter retrospective study. Radiology 247:762–770
Renshaw AA, Gould EW (2013) Should “indeterminate” diagnoses be used for thyroid fine-needle aspirates of nodules smaller than 1 cm? Arch Pathol Lab Med 137:1627–1629
Lee YH, Kim DW, In HS, Park JS, Kim SH, Eom JW, Kim B, Lee EJ, Rho MH (2011) Differentiation between benign and malignant solid thyroid nodules using an US classification system. Korean J Radiol 12:559–567
Choi WJ, Baek JH (2013) Role of core needle biopsy for patients with indeterminate, fine-needle aspiration cytology. Endocrine
Nasrollah N, Trimboli P, Guidobaldi L, Cicciarella Modica DD, Ventura C, Ramacciato G, Taccogna S, Romanelli F, Valabrega S, Crescenzi A (2013) Thin core biopsy should help to discriminate thyroid nodules cytologically classified as indeterminate. A new sampling technique. Endocrine 43:659–665
Choi YS, Hong SW, Kwak JY, Moon HJ, Kim EK (2012) Clinical and ultrasonographic findings affecting nondiagnostic results upon the second fine needle aspiration for thyroid nodules. Ann Surg Oncol 19:2304–2309
Choi SH, Han KH, Yoon JH, Moon HJ, Son EJ, Youk JH, Kim EK, Kwak JY (2011) Factors affecting inadequate sampling of ultrasound-guided fine-needle aspiration biopsy of thyroid nodules. Clin Endocrinol (Oxf) 74:776–782
Moon HJ, Kwak JY, Kim EK, Kim MJ (2011) Ultrasonographic characteristics predictive of nondiagnostic results for fine-needle aspiration biopsies of thyroid nodules. Ultrasound Med Biol 37:549–555
Hryhorczuk AL, Stephens T, Bude RO, Rubin JM, Bailey JE, Higgins EJ, Fox GA, Klein KA (2012) Prevalence of malignancy in thyroid nodules with an initial nondiagnostic result after ultrasound guided fine needle aspiration. Ultrasound Med Biol 38:561–567
Lubitz CC, Nagarkatti SS, Faquin WC, Samir AE, Hassan MC, Barbesino G, Ross DS, Randolph GW, Gaz RD, Stephen AE, Hodin RA, Daniels GH, Parangi S (2012) Diagnostic yield of nondiagnostic thyroid nodules is not altered by timing of repeat biopsy. Thyroid 22:590–594
Jo VY, Vanderlaan PA, Marqusee E, Krane JF (2011) Repeatedly nondiagnostic thyroid fine-needle aspirations do not modify malignancy risk. Acta Cytol 55:539–543
Park KT, Ahn SH, Mo JH, Park YJ, do Park J, Choi SI, Park SY (2011) Role of core needle biopsy and ultrasonographic finding in management of indeterminate thyroid nodules. Head Neck 33:160–165
Acknowledgement
The scientific guarantor of this publication is Jung Hwan Baek. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. This retrospective study was approved by the Institutional Review Board, and required neither patient approval nor informed consent for review of the images and medical records. However, informed consent for FNA or CNB was obtained from all patients prior to biopsy. Some nodules with CNB (n = 123) in this study have been used in a previously published article (Yeon et al. Radiology 2013; 268(1):274–80), which evaluated the role of CNB in thyroid nodules with initially non-diagnostic cytological results. In our study, we enrolled a relatively large number of study subjects (n = 180) for CNB and repeated FNA (n = 180) as a control group. Therefore, we believe that our study results provide more valuable information and options for both clinicians and patients to avoid unnecessary diagnostic surgery. Methodology: retrospective case-control study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, S.H., Baek, J.H., Lee, J.H. et al. Thyroid nodules with initially non-diagnostic, fine-needle aspiration results: comparison of core-needle biopsy and repeated fine-needle aspiration. Eur Radiol 24, 2819–2826 (2014). https://doi.org/10.1007/s00330-014-3325-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3325-4