Abstract
Indeterminate neoplasms (IN) represent the gray zone of thyroid cytology in which malignant and benign tumors cannot be discriminated. Recently, the approach by thin core needle biopsy has been proposed. Here we report a new thin core needle biopsy approach in 40 consecutive patients with thyroid IN at cytology. In this study, a 21-G needle was inserted into the nodule, advanced within the lesion, and moved ahead reaching extranodular tissue. The resulting sample allowed to evaluate the cytomorphology of nodular tissue, its relationship with extranodular parenchyma, and the nodule’s capsule when present. All biopsies were adequate for diagnosis but one. Of the 39 adequate samples, 5 cases were papillary cancer as confirmed at histology, while 14 nodules avoided surgery because of Hürthle cell hyperplasia in thyroiditis (n = 6) and microfollicular adenomatous hyperplasia (n = 8). The remaining 20 cases were assessed as follicular neoplasms because of encapsulation and were evaluated by immunohistochemistry. Of these, 6 had positive markers in different degree and 1/6 has follicular cancer at histology, while the other 14 were benign after surgery. Overall, this approach by thin core needle biopsy identified benignancy in 14/40 (35 %) IN avoiding surgery. As a conclusion, thin core biopsy should help to discern the nature of thyroid lesions cytologically classified as indeterminate, and it should be used as a complementary test in thyroid nodule assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fine-needle aspiration cytology (FNAC) represents the main diagnostic tool in evaluating both palpable and non palpable thyroid nodules because of its high accuracy, reproducibility, and cost effectiveness [1]. However, while FNAC is very reliable in detecting papillary (PTC) and anaplastic thyroid cancer, indeterminate neoplasms (IN), defined as a monotonous cellular population with scant or absent colloid, represent the gray zone of cytology [2]. In fact, in these lesions cytologic evaluation cannot discriminate malignant (i.e., follicular carcinoma and follicular variant of PTC) from benign (i.e., follicular adenoma and nodular adenomatous goiter) tumors [3]. As a consequence, in the presence of cytologic report of IN, thyroidectomy is required. Nevertheless, since about 80 % of these nodules are benign at histology, surgery in itself is unnecessary in a large number of these cases. Thus, the identification of parameters in predicting malignancy is strongly required.
Thyroid core needle biopsy, first described in 1990’s [4, 5], allows to obtain histologic sample by large gauge (i.e., 16–18) needle, with consequent discomfort and possible complications for patients. Previous studies have noted a low increased incidence of bleeding associated with core biopsy [5]. To date, this approach was rarely analyzed in thyroid nodules, and the data are still sparse [6–13]. Then, because of the above reasons, core needle biopsy is not recommended by current International thyroid nodule guidelines. In this regard, the approach by thin (22–20 gauge) core needle biopsy (TCB) has been proposed [9]. These needles should allow to adequately sample both large and small thyroid nodules, avoiding patient’s discomfort. The core devices are semi automated, allowing careful positioning of the needle tip and sampling of the target, on ultrasound (US) guide.
Here we reported a new TCB approach in forty patients with IN at cytology. The critical point of this technique was the sampling scheme: the needle cuts thyroid tissue starting within the nodule and across its border. This approach has not been described in thyroid to date. The resulting sample includes a rim of nodular and extranodular tissue, and nodule’s fibrous capsule, when present.
Materials and methods
Patients
In the period from December 2011 to May 2012 364 thyroid nodules underwent FNA at Ospedale Israelitico. Of these, 23 (6.3 %) were classified as malignant (Tir 5, see below), 16 (4.4 %) as suspicious for malignant (Tir 4), 40 (11 %) as indeterminate (Tir 3), 250 (68.7 %) as benign (Tir 2), and 35 (9.6 %) as inadequate (Tir 1). The 40 consecutive patients (37 females and 3 males, mean age 43 ± 13.8 years) with indeterminate cytology were enrolled in the study. Nodules size ranged from 6 to 20 mm. All cytologic examinations have been made by an expert cytopathologist (LG) at Ospedale Israelitico of Rome. Cytologic samples were classified according to SIAPEC-IAP consensus [14]: Tir 1 (inadequate), Tir 2 (benign), Tir 3 (indeterminate), Tir 4 (suspicious for malignancy), and Tir 5 (malignant). Biopsy was performed at least 3 months after FNAC. Informed consensus was obtained in all patients.
Biopsy technique
Patient was instructed not to take aspirin or any other anticoagulants in the 5 days prior to biopsy. Thyroid gland was evaluated by ultrasound system using a 13 MHz linear probe before biopsy. Patient was asked to assume supine position with hyperextend neck. After skin disinfection, local anesthesia by 2 cc of mepavacain 1 % was administered. Biopsy was performed using a modified 21-G Menghini cutting needle having length of 10 cm and diameter of 0.514 mm (Biomol, Hospital Service, Rome, Italy). The needle was inserted into the nodule under US guide in freehand fashion. When the tip was inside of the nodule, mandrel was removed and needle was advanced within the nodule to obtain a tissue core. Needle was moved ahead across the nodule’s margin reaching extranodular tissue. Then, the needle was removed. The obtained core sample was fixed by buffered formalin 10 %. Figure 1 shows a schematic illustration of the above procedure. After biopsy, mild compression on the site of biopsy was applied. Patient was kept under surveillance for about 60 min and underwent US re-evaluation. The procedure was performed in outpatients surgery of Ospedale Israelitico of Rome by the same experienced surgeon (NN).
Schematic illustration of the herein used sampling technique: the 21-G Menghini cutting needle is inserted into the nodule (a); mandrel is removed (b); needle is advanced within the nodule and moved ahead across the nodule’s margin reaching extranodular tissue (c); needle is removed, and the obtained core sample consists of nodular tissue, extranodular parenchyma, and nodule’s capsule when present (d)
Histologic examination
The formalin-fixed cores of tissue were automatically processed and embedded in paraffin. Serial four micron sections were picked up on polarized slide: the first was stained with hematoxylin–eosin; the others were treated with immunohistochemistry for galectin-3, cytokeratin-19, and HBME-1 (Thermo Fisher Scientific, CA, USA) and revealed by peroxidase using biotin-free method. All cases were observed by two experienced pathologists (AC, ST).
In all core samples, following criteria were evaluated: (a) the presence of a collagen parallel row at a core edge, consistent with fibrous capsule; (b) architectural pattern of grow (size of follicles, trabecule, solid areas); (c) cytologic features (nuclear size and morphology, cytoplasm stain, cell polarity); (d) the presence and characteristics of colloid; (e) the presence of calcific debris; and (f) galectin-3, cytokeratin-19, and HBME-1 immunophenotype of follicular cells.
Statistical analysis
Comparison of frequency was made by χ 2 test, using Graph Pad Prism (Graph Pad Software Inc., USA).
Results
Out of the 40 biopsies, 39 provided adequate material for diagnosis. One was entirely constituted by fibrin clots and inadequate for examination.
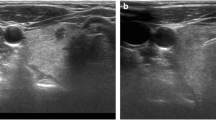
Five cases were characterized by nuclear features of PTC and reported as follicular variant of PTC. These cases were previously classified as indeterminate due to the microfollicular prevalent structure and the absence of nuclear clearing and pseudoinclusion, which were appreciable after TCB as reported for formalin-fixed paraffin-embedded material [15]; this, combined with the evaluation of histologic architecture, allowed the diagnosis (Fig. 2). After thyroidectomy, diagnosis was confirmed at histologic evaluation in all these 5 nodules. The initial cytologic samples of these five cases were reviewed and indeterminate report was confirmed in all cases. Hürthle cell proliferation combined with lymphocytic infiltrate, consistent with Hürthle cell hyperplasia in Hashimoto thyroiditis was found in 6 cases. Eight cases resulted lacking of fibrous capsule with microfollicular proliferation in closed relationship with surrounding normal parenchyma so they were assessed as microfollicular adenomatous hyperplasia. These 14 cases had triple negative immunohistochemistry. Finally, 20 cases were set as follicular neoplasms because of encapsulation (Fig. 3) and the risk of malignancy was stratified by immunohistochemistry (galectin-3, cytokeratin-19, and HBME-1). Of these, 14 had triple negative, while 6 had positive immunohistochemical markers in various degree (1 showed triple positive, 4 were focally positive for cytokeratin-19, and 1 was focally positive for galectin-3 and cytokeratin-19). These 20 patients were addressed to surgical management. At histology, benign neoplasm was found in all cases but one. The latter had triple positive staining at immunohistochemistry and harbored a follicular cancer. Figure 4 illustrates the main results of the study.
Core biopsy from a non-encapsulated nodule. A diagnosis of follicular variant of papillary carcinoma was made based on nuclear morphology (HE stain). The arrow indicates the absence of nodule’s fibrous capsule (a). Same case tested with immunohistochemistry. The three markers of the panel resulted positive (galectin-3 immunohistochemistry) (b)
Overall, TCB identified 19/40 (47.5 %) IN as benign (n = 14) or malignant (n = 5) which were not demonstrable by conventional FNA; then, the rate of lesions classified as diagnostic by initial FNA (79.4 %) increased to 84.9 % of combined FNA–TCB. The indeterminate nodules were reduced from 40 (11 % out of 364 FNA) to 20 (5.5 %) (P < 0.05).
No complications, such as pain or swelling, after the biopsy were recorded. The US re-evaluation reported neither perithyroid hemorrhage or parenchyma edema.
Discussion
Cytologically indeterminate thyroid nodules represent a main dilemma for thyroidologists. In fact, these follicular patterned lesions amount to about 15 % of thyroid cytologies, and they should harbor malignant and benign tumors. At histology, while adenomatous nodules lack well-defined fibrous capsule, follicular neoplasms manifest as encapsulated lesions [16]. This major difference is not evaluable by cytology, and, as a consequence, in these cases surgery is mandatory. Since benignancy rate is highly prevalent (80 %) at histologic evaluation, a large number of patients undergo unnecessary surgery. To date, several studies analyzing clinical, cytologic, or molecular parameters in predicting IN outcome have been reported, with discrepant findings [17–22]. More recently, core needle biopsy has been described as a diagnostic tool in this context [6, 13].
Aim of the present study was to test the diagnostic accuracy of a new technical approach by thin (21-G) core biopsy in forty consecutive IN. The results showed that five of these were PTC and were submitted for surgery. Twenty encapsulated follicular neoplasms underwent surgery too. Of the remaining nodules, six Hürthle cell hyperplasia in thyroiditis and eight adenomatous hyperplasia were addressed to follow-up. One was inadequate and needed to repeat biopsy. Target of our technique was to sample nodule’s border starting from the lesion inside. By this approach, a sample including core and periphery of the lesion was obtained, avoiding damage to the delicate extranodular tissue. The examination of this sample allowed to discriminate encapsulated from non-encapsulated nodules, distinguishing between adenomatous hyperplasia and truly encapsulated follicular neoplasms. This did not identify the malignant follicular cancer which requires the histologic evaluation of the whole nodule’s capsule after surgery. However, the absence of the capsule, combined with negative immunohistochemistry, identified the benign hyperplastic lesions which avoided the surgery. The presence of nodular capsule was confirmed in all excised nodules, thus underlining the utility of TCB to recognize encapsulated neoplasms. Also, morphologic evaluation of follicular cells identified follicular variant of PTC based on nuclear clearing and fine chromatin distribution, well discernible on paraffin-embedded samples (Fig. 2a). Cores from follicular encapsulated neoplasms, lacking reliable morphologic criteria of malignancy at biopsy, were evaluated using immunohistochemical markers. Risk stratification of malignancy was set by galectin-3, cytokeratin-19, and HBME-1 (Fig. 2b), previously reported as the more appropriate panel in IN [16, 23]. The positivity of the three immunohistochemical markers well identified the malignant lesion. In this context, it has to be mentioned the low specificity of a single immunohistochemical marker, while high accuracy is obtained with a triple positive staining predictive of malignancy and triple negative staining are supporting non malignant nature [24]. The herein reported new sampling and technical approach has not been described to date in thyroid. It allowed to identify 14 benign nodules (35 % of the IN series) thus permitting conservative approach.
To date, a few papers evaluated core biopsy in assessing IN, with interesting findings [6–13]. Park et al. [6] reviewed a series of IN aiming to compare the accuracy of a second FNAC, core biopsy, and surgery. Based on biopsy using 18-G needles, 42/54 (77.8 %) nodules had benign outcome, 11 (20.3 %) were assessed as PTC, and 1 (1.8 %) was indeterminate. More recently, Na et al. [12] compared a second FNAC with 18-G needle biopsy in nodules reading of nondiagnostic (n = 64) or atypia of indeterminate significance (n = 161) as assessed by Bethesda System [25, 26]. Core biopsy had reduced rate in both classes with respect to repeat FNAC. Furthermore, final diagnosis was obtained in 104 IN, and core biopsy correctly assessed 26/39 (66.7 %) benign and 44/65 (67.7 %) malignant tumors. The remaining cases were not diagnostic (3/65 cancer) or indeterminate (12/39 benignancy and 11/65 malignancy). Some complications were reported in 6 % patients. Another study [11] compared core biopsy and FNAC in 555 thyroid nodules which underwent both procedures. Core biopsy possessed lower IN rate than FNAC, and had improved accuracy when combined with FNAC. Similar results were found by Renshaw and Pinnar [27] on 337 nodules. Core biopsy, by 18- or 20- or 21-G needles, was less sensitive in diagnosing PTC, and had higher accuracy when associated with conventional cytology. A 20–22 gauge needle TCB has been reported by Zhang et al. [9] in a large series of nodules with inadequate or suboptimal cytologic outcome. Subjects underwent FNAC or both FNAC and TCB. Tissue fragments by TCB were larger than FNAC, and inadequacy was recorded in 8.7 % of FNAC and 3.4 % of combined FNAC/TCB. Also, minor complications were similar between FNAC and FNAC/TCB patients, and no major complications were observed. Whether to repeat FNA in nodules with previously not diagnostic report is a matter to debate [28]. In this regard an interesting paper has been recently reported. There, Samir et al. [13] showed that the combination of FNA and 25-G TCB can classify as diagnostic 87 % of thyroid lesions with prior inadequate FNA. Here, TCB detected 5 follicular variant papillary cancers and 14 benign lesions, indeterminate cytologies were significantly reduced, and the combined TCB-FNA diagnosis achieved 85 %. According to Zhang et al. [9], 1/40 TCB of the present series was inadequate, and no complications were recorded. Moreover, small needle caliber of TCB furnished adequate tissue sample. Our technique of sampling, by positioning the needle inside of nodule and advancing it to nodule’s border, allowed to evaluate nodular parenchyma, extranodular tissue, and nodule’s capsule when present. This kind of sampling avoids tissue compression or nodule escape that may represent a problem when the needle approaches the nodule from normal parenchyma to the lesion, especially when a thick fibrous or calcified capsule is present. The relevance of a high-quality evaluation of nodule border subsists in the possibility to distinguish among follicular lesions the adenomatous non-encapsulated nodules from truly neoplastic encapsulated lesion. The examination of nuclear morphology, histologic architecture, and associated pathology (i.e., lymphocytic infiltration) completes the diagnostic skill offered by the core. By this approach 35 % indeterminate neoplasms were assessed as benign. Based on the present data and considering the stringent match of core diagnosis with definitive histology, TCB sample should accurately assess nuclear change, general alterations in follicular structure, and relations with adjacent tissues. Furthermore, core biopsy was fixed in formalin immediately after it was collected, thus avoiding technical artifacts due to delayed fixation or inadequate smearing. The latter should represent a crucial interpretative limit in thyroid cytology. In this context, it has to be mentioned that core tissue is reported as suitable for various molecular investigation (i.e., FISH for chromosomal rearrangement or mutational analysis) improving diagnostic and prognostic assessment [29, 30]. This represents our future aim.
Because of the original sampling technique used, these data should contribute to define the role of thin core biopsy in indeterminate thyroid nodule assessment. The critical point of this technique was the sampling scheme: the needle cuts thyroid tissue starting within the nodule and across its border. The resulting sample is a tissue cylinder that includes a rim of nodular and extranodular tissue, and nodule’s fibrous capsule when present. This approach has not been described in thyroid nodules to date. Thin core needle biopsy identified benignancy in about 1/3 of indeterminate nodules thus avoiding surgery. Moreover, based on triple negative immunohistochemical panel and according to clinical setting, it should be possible to consider conservative approach in some encapsulated follicular lesions.
In conclusion, the herein reported new operative method for thin core biopsy should help to discern the nature of thyroid nodules classified as indeterminate at cytology. The procedure, performed with a passage starting from inside of the nodule by expert surgeons or radiologists, allows to obtain an adequate sample of nodular and extranodular tissue, and to exam the nodule’s border. To date, a few data on TCB in thyroid nodule exist, and this approach should be used as a complementary test in nodules with cytologic outcome of indeterminate.
References
H. Gharib, J.R. Goellner, Fine-needle aspiration biopsy of thyroid: an appraisal. Ann. Intern. Med. 118, 282–289 (1993)
Z.W. Baloch, S. Fleisher, V.A. LiVolsi, P.K. Gupta, Diagnosis of “follicular neoplasm”: a gray zone in thyroid fine-needle aspiration cytology. Diagn. Cytopathol. 26, 41–44 (2002)
Z.W. Baloch, M.J. Sack, G.H. Yu, V.A. Livolsi, P.K. Gupta, Fine-needle aspiration of thyroid: an institutional experience. Thyroid 8, 565–569 (1998)
A. Carpi, A. Sagripanti, A. Nicolini, S. Santini, E. Ferrari, R. Romani, G. Di Coscio, Large needle aspiration biopsy for reducing the rate of inadequate cytology on fine needle aspiration specimens from palpable thyroid nodules. Biomed. Pharmacother. 52, 303–307 (1998)
Q. Liu, M. Castelli, P. Gattuso, R.A. Prinz, Simultaneous fine-needle aspiration and core-needle biopsy of thyroid nodules. Am. Surg. 61, 628–632 (1995)
K.T. Park, S.H. Ahn, J.H. Mo, Y.J. Park, J. Park, S.I. Choi, S.Y. Park, Role of core needle biopsy and ultrasonographic finding in management of indeterminate thyroid nodules. Head Neck 33, 160–165 (2011)
J.D. Oppenheimer, D. Kasuganti, R. Nayar, H.B. Chrisman, R.J. Lewandowski, A.A. Nemcek Jr, R.K. Ryu, How to interpret thyroid biopsy results: a three-year retrospective interventional radiology experience. Cardiovasc. Intervent. Radiol. 33, 800–805 (2010)
J.N. Harvey, D. Parker, P. De, R.K. Shrimali, M. Otter, Sonographically guided core biopsy in the assessment of thyroid nodules. J. Clin. Ultrasound 33, 57–62 (2005)
S. Zhang, M. Ivanovic, A.A. Nemcek Jr., D.V. Defrias, E. Lucas, R. Nayar, Thin core needle biopsy crush preparations in conjunction with fine-needle aspiration for the evaluation of thyroid nodules: a complementary approach. Cancer (Cancer Cytopathol.) 114, 512–518 (2008)
N.J. Screaton, L.H. Berman, J.W. Grant, US-guided core-needle biopsy of the thyroid gland. Radiology 226, 827–832 (2003)
J.Y. Sung, D.G. Na, K.S. Kim, H. Yoo, H. Lee, J.H. Kim, J.H. Baek, Diagnostic accuracy of fine-needle aspiration versus core-needle biopsy for the diagnosis of thyroid malignancy in a clinical cohort. Eur. Radiol. 22, 1564–1572 (2012)
D.G. Na, J.H. Kim, J.Y. Sung, J.H. Baek, K.C. Jung, H. Lee, H. Yoo, Core-needle biopsy is more useful than repeat fine-needle aspiration in thyroid nodules read as nondiagnostic or atypia of undetermined significance by the Bethesda system for reporting thyroid cytopathology. Thyroid 22, 468–475 (2012)
A.E. Samir, A. Vij, M.K. Seale, G. Desai, E. Halpern, W.C. Faquin, S. Parangi, P.F. Hahn, G.H. Daniels, Ultrasound-guided percutaneous thyroid nodule core biopsy: clinical utility in patients with prior nondiagnostic fine-needle aspirate. Thyroid 22, 461–467 (2012)
G. Fadda, F. Basolo, A. Bondi, G. Bussolati, A. Crescenzi, O. Nappi, F. Nardi, M. Papotti, G. Taddei, L. Palombini, SIAPEC-IAP Italian Consensus Working Group: Cytological classification of thyroid nodules. Proposal of the SIAPEC-IAP Italian Consensus Working Group. Pathologica 102, 108–405 (2010)
J. Rosai, L.C. Carcangiu, Papillary carcinoma. In: Atlas of tumor pathology: tumors of thyroid gland. Series 3 (AFIP, Whashington D.C., 1992)
S.R. Kini, Thyroid cytopathology: an atlas and text (Lipincott Williams & Wilkins, Philadelphia, 2008)
A. Bartolazzi, F. Orlandi, E. Saggiorato, M. Volante, F. Arecco, R. Rossetto, N. Palestini, E. Ghigo, M. Papotti, G. Bussolati, M.P. Martegani, F. Pantellini, A. Carpi, M.R. Giovagnoli, S. Monti, V. Toscano, S. Sciacchitano, G.M. Pennelli, C. Mian, M.R. Pelizzo, M. Rugge, G. Troncone, L. Palombini, G. Chiappetta, G. Botti, A. Vecchione, R. Bellocco, Italian Thyroid Cancer Study Group (ITCSG). Galectin-3-expression analysis in the surgical selection of follicular thyroid nodules with indeterminate fine-needle aspiration cytology: a prospective multicentre study. Lancet Oncol. 9, 543–549 (2008)
T. Rago, G. Di Coscio, F. Basolo, M. Scutari, R. Elisei, P. Berti, P. Miccoli, R. Romani, P. Faviana, A. Pinchera, P. Vitti, Combined clinical, thyroid ultrasound and cytological features help to predict thyroid malignancy in follicular and Hürthle cell thyroid lesions: results from a series of 505 consecutive patients. Clin. Endocrinol. (Oxf.) 66, 13–20 (2007)
P. Trimboli, E. Condorelli, A. Catania, S. Sorrenti, Clinical and ultrasound parameters in the approach to thyroid nodules cytologically classified as indeterminate neoplasm. Diagn. Cytopathol. 37, 783–785 (2009)
B. Cakir, C. Aydin, B. Korukluoğlu, D. Ozdemir, I.C. Sisman, D. Tüzün, A. Oguz, G. Güler, G. Güney, A. Kuşdemir, S.Y. Sanisoglu, R. Ersoy, Diagnostic value of elastosonographically determined strain index in the differential diagnosis of benign and malignant thyroid nodules. Endocrine 39, 89–98 (2011)
L. García-Pascual, M.J. Barahona, M. Balsells, C. del Pozo, J. Anglada-Barceló, J. Casalots-Casado, E. Veloso, J. Torres, Complex thyroid nodules with nondiagnostic fine needle aspiration cytology: histopathologic outcomes and comparison of the cytologic variants (cystic vs. acellular). Endocrine 39, 33–40 (2011)
K. Gul, R. Ersoy, A. Dirikoc, B. Korukluoglu, P.E. Ersoy, R. Aydin, S.N. Ugras, O.K. Belenli, B. Cakir, Ultrasonographic evaluation of thyroid nodules: comparison of ultrasonographic, cytological, and histopathological findings. Endocrine 36, 464–472 (2009)
S. Rezk, K. Ashraf, Role of immunohistochemistry in the diagnosis and progression of follicular epithelium derived thyroid carcinoma. Appl. Immunohistochem. Mol. Morphol. 13, 256–264 (2005)
E. Saggiorato, R. De Pompa, M. Volante, S. Cappia, F. Arecco, A.P. Dei Tos, F. Orlandi, M. Papotti, Characterization of thyroid ‘follicular neoplasms’ in fine-needle aspiration cytological specimens using a panel of immunohistochemical markers: a proposal for clinical application. Endocr. Relat. Cancer 12, 305–317 (2005)
Z.W. Baloch, E.S. Cibas, D.P. Clark, L.J. Layfield, B.M. Ljung, M.B. Pitman, A. Abati, The National Cancer Institute Thyroid fine needle aspiration state of the science conference: a summation. Cytojournal 7, 5–6 (2008)
E.S. Cibas, S.Z. Ali, The Bethesda system for reporting thyroid cytopathology. Thyroid 19, 1159–1165 (2009)
A.A. Renshaw, N. Pinnar, Comparison of thyroid fine-needle aspiration and core needle biopsy. Am. J. Clin. Pathol. 128, 370–374 (2007)
F.F. Maia, P.S. Matos, E.J. Pavin, J. Vassallo, D.E. Zantut-Wittmann, Value of repeat ultrasound-guided fine-needle aspiration in thyroid nodule with a first benign cytologic result: impact of ultrasound to predict malignancy. Endocrine 40, 290–296 (2011)
J.M. Sáez, Treatment directed to signaling molecules in patients with advanced differentiated thyroid cancer. Anticancer Agents Med. Chem. (2012)
K. Buxey, J. Serpell, Importance of core biopsy in the diagnosis of thyroid lymphoma. ANZ J. Surg. 82, 90 (2012)
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nasrollah, N., Trimboli, P., Guidobaldi, L. et al. Thin core biopsy should help to discriminate thyroid nodules cytologically classified as indeterminate. A new sampling technique. Endocrine 43, 659–665 (2013). https://doi.org/10.1007/s12020-012-9811-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-012-9811-z