Abstract
Objectives
To evaluate the accuracy of low-dose coronary CTA with iterative reconstruction (IR) in the diagnosis of coronary artery disease (CAD) in patients with suspected CAD.
Methods
Ninety-six patients with suspected CAD underwent low-dose prospective electrocardiogram-gated coronary CTA, with images reconstructed using IR. Image quality (IQ) of coronary segments were graded on a 4-point scale (4, excellent; 1, non-diagnostic). With invasive coronary angiography (ICA) considered the “gold standard”, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of coronary CTA were calculated on segment-, vessel- and patient-based levels. The patient data were divided into two groups (Agatston scores of ≥ 400 and <400). The differences in diagnostic performance between the two groups were tested.
Results
Diagnostic image quality was found in 98.1 % (1,232/1,256) of segments. The sensitivity, specificity, PPV, NPV and accuracy were 90.8 %, 95.3 %, 81.8 %, 97.8 % and 94.3 % (segment-based) and 97.2 %, 83.3 %, 94.6 %, 90.9 % and 93.8 % (patient-based). Significant differences between the two groups were seen in specificity, PPV and accuracy (92.1 % vs. 97.9 %, 76.0 % vs. 86.7 %, 91.7 % vs. 96.6 %, P < 0.05; segment-based). The average effective dose was 1.30 ± 0.15 mSv.
Conclusion
Low-dose prospective coronary CTA with IR can acquire satisfactory image quality and show high diagnostic accuracy in patients with suspected CAD; however, blooming continues to pose a challenge in severely calcified segments.
Key Points
• Coronary artery disease (CAD) is increasingly investigated using coronary CTA.
• The iterative reconstruction (IR) algorithm is promising in decreasing radiation doses.
• Low-dose prospective coronary CTA with IR can acquire satisfactory image quality.
• Low-dose prospective coronary CTA with IR can show high diagnostic accuracy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary computed tomography angiography (coronary CTA) is known to be one of the most sensitive non-invasive methods of detecting coronary artery stenosis [1–5]. However, the high radiation dose limits its wide application. Recent approaches such as prospective electrocardiogram (ECG) gating and high-pitch helical mode on newer multi-detector CT (MDCT) devices can reduce the radiation dose to less than 4 mSv [5–9]. The application of an iterative reconstruction (IR) algorithm helps to further decrease the radiation dose. Evidence suggests that at equal radiation doses, the images reconstructed with IR algorithms have lower noise and an improved contrast-to-noise ratio (CNR) and signal-to-noise ratio (SNR) compared with those reconstructed with the filtered back projection (FBP) algorithm [10–12].
Experiments involving phantoms and subjects have shown that IR algorithms can generate images with image quality equivalent to FBP reconstructions while at the same time facilitating radiation dose reductions in the range of 30–76 % [12–16]. The combination of prospectively ECG-triggered scans and the IR algorithm can decrease the radiation dose of coronary CTA to 1–2 mSv, well below the average background radiation levels [17]. However, there has been very limited work investigating the diagnostic accuracy of using the IR algorithm in low-dose coronary CTA. A recent study by Moscariello et al. [18] compared the diagnostic capability of the IR algorithm with FBP with the IR algorithm used on ‘low-dose’ acquisitions simulated from routine dose acquisitions (used for FBP reconstructions) by discarding half of the projection data with promising results. However, because both acquisition techniques (traditional retrospective helical and prospective axial) were used, no sub-group analysis was performed to independently evaluate the performance of IR on the prospective axial group. To the best of our knowledge, the diagnostic accuracy of prospectively ECG-triggered 256-slice low-dose coronary CTA images reconstructed by the IR algorithm has not been reported. Therefore, we aim to investigate the diagnostic performance of IR algorithms in prospectively ECG-triggered 256-slice coronary CTA acquisitions in patients with suspected coronary artery disease (CAD) who were referred to invasive coronary angiography.
Materials and methods
Patients
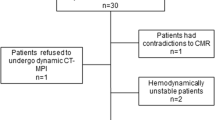
One hundred consecutive patients (74 male, 26 female) with a pre-test probability of CAD of 50–60 % who were scheduled for invasive coronary angiography (ICA) between September 2011 and July 2012 for evaluation of CAD were prospectively enrolled to undergo coronary CTA. Of these, four patients had prior coronary artery stents or coronary artery bypass grafts (CABG) and were excluded from the study. Thus, 96 patients (70 male, 26 female) were included in the study. This study was approved by our institutional review board. All ICA examinations were performed within 2 weeks of coronary CTA. All patients gave written informed consent before CT examination. Patients with nephropathy or known allergy to iodinated contrast media, severe renal inadequacy (creatinine clearance rate ≤120 μmol/l), severe arrhythmia, cardiac function or TIMI flow < grade III after coronary artery stenting or coronary artery bypass grafting (CABG) were excluded.
For study evaluation, patients were subdivided into two groups according to the calcium scores: group A included patients with Agatston calcium scores <400 and group B included patients with Agatston scores ≥ 400.
CT Examination
All CT examinations were performed with prospective ECG-gating using 256-slice multi-detector CT (Brilliance iCT, Philips Healthcare, Cleveland, OH, USA). The imaging procedure included a low-dose scout image followed by an unenhanced prospectively ECG-triggered coronary artery calcium scoring acquisition. The imaging parameters were as follows: tube potential = 120 kVp; effective tube current-time product = 50 mAs; detector configuration = 32 × 0.625 mm; rotation time = 330 ms; field of view = 250 mm; reconstructed slice thickness = 2.5 mm; increment = 2.5 mm. The imaging trigger was centred around a physiological cardiac phase of ventricular diastasis corresponding to 75 % of the R-R interval.
The images from the calcium scoring study were used to determine calcium scores and also to optimise the imaging length for the diagnostic coronary CTA. Automatic bolus tracking (Bolus Pro, Philips Healthcare, Cleveland, OH, USA) was used with a region of interest in the ascending aorta at the level of the pulmonary artery. CT data acquisition was initiated under full inspiration 6 s after a pre-determined signal attenuation threshold of 180 Hounsfield units (HU) had been attained; 60–70 ml of contrast media (Iohexol 350; GE Healthcare, Shanghai, China) followed by 20 ml of saline was intravenously injected at a flow rate of 5–6 ml/s into the antecubital vein using a dual-tube high pressure syringe (Ulrich REF XD 2051; Ulrich Medical GmbH, Ulm, Germany) equipped with an 18-gauge catheter. The coronary CTA parameters were as follows: tube potential = 120 kVp; effective tube current-time product = 105 mAs; no AEC was used; detector configuration = 128 × 0.625, 112 × 0.625 or 96 × 0.625 mm adjusted to imaging length; rotation time = 270 ms; field of view = 250 mm; slice thickness = 0.9 mm; increment = 0.45 mm. The imaging trigger was centred around a physiological cardiac phase of ventricular diastasis corresponding to 75 % of the R-R interval, with a ±5 % buffer used when the fluctuation of heart rate (HR) was >5 beats/min (bpm). The standard temporal resolution of 256-slice CCTA using prospective ECG-gated axial CT is 135 ms. Before the CT examination, patients with HR > 70 bpm were administered oral ß-receptor blockers (12.5–25 mg metoprolol succinate sustained-release tablets, AstraZeneca, Sweden) to decrease and stabilise the HR. The entire volume of the cardiac anatomy was scanned in a single breath hold of 3–5 s.
CT data reconstruction and image analysis
A fourth generation IR algorithm (iDose4, Philips Healthcare, Cleveland OH, USA) was used to reconstruct the images from the low-dose acquisitions. The technical details and the algorithm’s applicability in coronary CTA have been explained in previous work [12, 19]. IR levels of L4 were used to compensate for the noise increase that would result from dose reductions of 50 % [12, 17]. All reconstructions were targeted to provide spatial resolution of the sharp reconstruction kernel (XCC). The matrix size of the reconstructed images was 512 × 512.
The 256-slice CT data analysis
Coronary segments were defined according to a reporting system of the American Heart Association (AHA) [18]. The right coronary artery (RCA) was defined to include segments 1–4, the left main artery to consist of segment 5, the left anterior descending (LAD) artery to include segments 6–10, and the left circumflex artery (LCX) to include segments 11–15. If present, the intermediate artery (ramus intermedius) was designated as segment 16 and considered to belong to the LAD. All diameter measurements were performed with an electronic calliper tool provided with the workstation (Extended Brilliance Workspace Version 4.01, Philips Healthcare, Cleveland, OH, USA).
Coronary CTA data analysis was performed by two blinded and independent observers with 10 and 12 years’ experience in coronary CTA. Both were unaware of the clinical history. The image quality of each coronary segment was rated on a four-point scale as follows: 4: excellent (no artefacts, unrestricted evaluation); 3: good (minor artefacts, good diagnostic quality); 2: fair (moderate artefacts, still acceptable and diagnostic) and 1: non-diagnostic (severe artefacts impairing accurate evaluation) (Fig. 1). Then, both observers assessed all coronary artery segments for the presence of significant stenosis (defined as luminal diameter narrowing exceeding 50 %). For any disagreement in data analysis, a consensus agreement was reached.
Invasive coronary angiography
Invasive coronary angiography (ICA) was performed according to standard techniques and at least two views in different planes were obtained for each coronary artery. One experienced observer who was aware of the patients’ clinical history but blinded to the results from coronary CTA evaluated all angiograms with regard to the presence (diameter reduction > 50 %) or absence of significant stenoses. Coronary artery segments were defined according to the AHA reporting system described above [20]], similar to coronary CTA.
Estimation of radiation dose
For the estimation of CT radiation dose, the CT volume dose index (CTDIvol) and the dose-length product (DLP) were recorded and used for estimations. The effective dose (ED) of coronary CTA was derived from the product of the DLP and a conversion coefficient (k = 0.014 mSv•mGy−1•cm−1) [21].
Statistical analysis
All statistical analyses were performed using commercially available software (SPSS, Release 17.0, SPSS, USA). Quantitative variables were expressed as mean ± standard deviation and categorical variables as frequencies and percentages. Kappa statistics were calculated for interobserver agreements for image quality read-out and assessment of significant coronary artery stenosis with coronary CTA.
With ICA considered the “gold standard”, the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of coronary CTA were calculated on segment-, vessel- and patient-based levels. The patients were divided into two groups according to Agatston scores of ≥ 400 (group A) and <400 (group B). All vessels and patients were included in vessel- and patient-based analyses. Non-evaluable segments (caused by coronary motion, etc.) were considered as positive and segments that had a minimal diameter of <1.5 mm at their origin were excluded from per-segment analysis. Because our goal was to evaluate the accuracy of coronary CTA with IRT in the presence of severe calcifications, all calcified segments were included in our analysis. Per-segment, per-vessel or per-patient statistics for the diagnostic accuracy of coronary CTA were performed (i.e. lesions of the left main coronary artery or diagonal branches were included in the LAD, lesions of obtuse marginal branches were included in the LCX, lesions of posterior descending or postero-lateral branches were included in the RCA). A vessel and a patient were considered to be diseased if significant stenosis was found in at least one coronary segment. Differences regarding the baseline data and diagnostic accuracy between the two groups were tested for significance using the chi-squared or the Fisher’s exact test, if appropriate. A P value of <0.05 was considered statistically significant.
Results
Low-dose prospectively ECG-triggered coronary CTA with the IR algorithm was successfully performed in all 96 patients without adverse effects. The prevalence of disease was 75 %. The clinical characteristics of the patients enrolled are summarised in Table 1.
Image quality of prospectively ECG-triggered coronary CTA with IR algorithms
Interobserver agreement for image quality rating was good (kappa = 0.76). A total of 1,256 coronary artery segments were evaluated with CT; 184 segments were missing because of anatomical variants (n = 73), a minimal diameter of ≤1.5 mm at their origin (n = 66), the presence of stents (n = 18) or were distal to an occluded segment (n = 27).
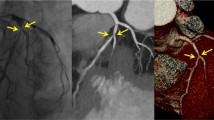
Diagnostic image quality was found in 98.1 % of segments (1,232/1,256). Excellent IQ (score 4) was present in 89.5 % of the coronary segments (1,124/1,256; Fig. 2), good IQ (score 3) in 7.5 % (94/1,256), fair IQ (score 2) in 1.1 % (14/1,256) and a non-diagnostic IQ (score 1) in 24 segments (1.9 %) in 6 patients. Reasons for non-diagnostic image quality were motion artefacts in 13 segments in three patients (54.2 %) whose HR increased to > 75 bpm immediately after the contrast medium injection, stair-step artefacts in 6 (25.0 %) segments in 2 patients, and low contrast opacification in 5 segments in 2 patients (20.8 %). All images reconstructed with the IR algorithm displayed a natural look and feel.
Prospectively gated transaxial (PGT) 256-slice coronary CT angiography (CTA) with iterative reconstruction (IR) of a 55-year-old woman [BMI: 25 kg/m2 and mean heart rate (HR): 62 ± 1.0 bpm]. (a-c) Curved multiplanar reformation (CMPR) of the left anterior descending artery (LAD), the circumflex artery (LCX) and right coronary artery (RCA), and (d) volume-rendered depiction showing normal coronary artery system. All segments were ranked 4 (excellent). Effective dose: 1.3 mSv
Diagnostic accuracy of prospectively ECG-triggered coronary CTA with the IR algorithm
The interobserver kappa value for the evaluation of stenosis was 0.82 for segment-based analysis, which indicates a good interobserver agreement. Using CCA as the reference standard, low-dose prospective coronary CTA examination with IR showed good sensitivity, specificity, positive predictive value, negative predictive value and accuracy on segment-, vessel- and patient-based analyses (Table 2).
In the segment-based analysis, coronary CTA correctly recognised 1,256 segments, which was consistent with the results of the ICA (Fig. 3); 22 segments failed to show the presence of significant stenosis (false negative) and 48 segments were incorrectly diagnosed as having significant narrowing (false positive). The causes of incorrect diagnosis were dense calcification in 58 segments (40 false positive, 18 false negative; Fig. 4) and motion artefacts in 10 segments (6 false positive, 4 false negative). Additionally, two segments in the middle part of the LCX were misdiagnosed as stenosis (false positive) because of compression caused by the crossing-over of the cardiac vein and low luminal density in that region. Per-segment, per-vessel and per-patient analyses with regard to the diagnostic accuracy of low-dose prospective coronary CTA in group A (Agatston score ≥ 400) and group B (Agatston score < 400) are shown in Table 3.
PGT 256-slice coronary CTA with IR (effective radiation dose 1.02 mSv) in a 56-year-old man (BMI: 23.5 kg/m2 and mean HR: 61 ± 1.5 bpm) with chest pain. CMPR of the RCA (a) shows non-calcified plaque in the mid and distal segment with severe stenoses. Catheter angiography of the RCA confirmed this (b)
PGT 256-slice coronary CTA with IR (effective radiation dose 1.28 mSv) in a 52-year-old man (BMI: 24.2 kg/m2 and mean HR: 64 ± 1.0 bpm) with chest pain. (a) Curved multiplanar reformation of the LAD shows significant stenosis in the proximal segment caused by calcified plaque, but it was false positive compared with catheter angiography (b)
The differences in diagnostic performance on a per-segment basis between groups A and B were significantly different except for sensitivity and negative predictive value (sensitivity, x 2 = 0.067, P = 0.796; specificity, x 2 = 18.845, P < 0.0001; positive predictive value, x 2 = 5.091, P = 0.024; negative predictive value, x 2 = 1.149, P = 0.284 and accuracy, x 2 = 13.882, P < 0.001).
In the vessel-based analysis, no significant differences in performance were observed except for specificity (sensitivity, x 2 = 2.378, P = 0.123; specificity, x 2 = 14.227, P < 0.0001; positive predictive value, x 2 = 0.002, P = 0.967; negative predictive value, x 2 = 1.29, P = 0.256; accuracy, x 2 = 1.91, P = 0.167).
Lastly, the differences in diagnostic performance on a per-patient basis between groups A and B were not significantly different (sensitivity: x 2 = 0.014, P = 0.905; specificity: x 2 = 0.137, P = 0.711; positive predictive value: x 2 = 0.028, P = 0.867; negative predictive value: x 2 = 0.075, P = 0.784; accuracy, x 2 = 0.07, P = 0.791).
Radiation dose of low-dose prospectively ECG-triggered coronary CTA with the IR algorithm
The average CTDI and DLP of the coronary CTA acquisitions were 8.20 ± 0.39 mGy (7.9–8.6 mGy) and 100.06 ± 10.68 mGy · cm (range, 78.29–120.10 mGy · cm). The effective dose (ED) was 1.30 ± 0.15 mSv (range, 1.02–1.68 mSv). In 78.1 % of patients (75/96), in whom the acquisitions were triggered at 75 % of the R-R interval without a ±5 % buffer, CTDIs were 8.03 ± 0.08 mGy (7.9–8.2 mGy) and ED was 1.14 ± 0.08 mSv (1.02–1.28 mSv). In the rest of the patients (21) in whom a ±5 % buffer was used, the CTDI was 8.46 ± 0.09 (8.3–8.6 mGy) and ED was 1.45 ± 0.12 mSv (1.27–1.68 mSv).
Discussion
Our results showed that low-dose prospectively ECG-triggered CTA with the IR algorithm can provide satisfactory image quality and has high sensitivity, specificity and accuracy (97.2 %, 83.3 %, 93.8 %) in patients with suspected CAD who were referred to ICA; however, as in other previously published studies, the presence of dense calcification continues to have an impact on the performance.
Good image quality is the basis for accurate evaluation of coronary artery disease. Several prospectively ECG-triggered CTA studies have confirmed that the percentage of coronary artery segments that can be diagnosed under a very low heart rate was 95–98.6 % [22–24]; 256-slice coronary CTA can be used under a wider range of heart rates than 64-slice CTA because it has a high standard temporal resolution [7]; in addition, its wide coverage can significantly reduce the acquisition time, thereby reducing the heart rate variations (and in turn making the images less sensitive to the fluctuations). The mean heart rate obtained in this study was 65 ± 3.5 bpm (range, 53–78), and under this range of heart rates, 98.1 % (1,232/1,256) of segments were diagnosed, consistent with previous reports [7, 24].
One of the causes of non-assessability of segments is motion artefacts arising from high HR. Even in patients who are on β-blockers to reduce and stabilise HR, the process of breath hold at the beginning of the acquisition could cause a sudden elevation of the HR before it settles down. This could cause a mismatch of the actual trigger phase and pre-designated (optimal) trigger phase, resulting in motion artefacts. This accounted for 54.2 % of the non-evaluable segments (13/24) in our study.
We used a hybrid IR algorithm (iDose4) in our study, which, by utilising a noise model in both projection and image domains, facilitated reduction in noise while at the same time preserving the tissue structure and the edges. This enables the use of various ‘levels’ of the algorithm, each of which provides a targeted reduction in noise to compensate for any noise increase that accompanies a given reduction in the tube output [16, 19], without resulting in any unnatural appearance of the image (“plastic appearance”) as encountered in earlier work [25]. Based on our previous experience, we determined that an IR level of L4 provided a good balance in image quality (i.e. maintained coronary luminal sharpness) for a given tube output [17].
In this study, low-dose prospectively ECG-triggered coronary CTA with the IR algorithm showed high sensitivity (89.7 %), specificity (95.3 %), positive predictive value (80.0 %) and negative predictive value (97.8 %) in a segment-based evaluation at a radiation dose of 1.30 ± 0.15 mSv. These results are similar to previous findings obtained from prospectively-gated coronary CTA and reconstructed with the FBP algorithm [5, 26, 27], but with further reductions in radiation dose. Hu et al. [5] performed high-pitch coronary CTA on a dual-source CT and obtained similar segment-based results at comparable effective radiation dose levels. Park et al. [27] performed a retrospective review of 64-slice coronary CTA performance in 110 patients with heavily calcified plaques (with Agatston score > 400) with comparable results.
Results from this study showed that the specificity, PPV and accuracy of coronary CTA for the detection of coronary stenosis were affected to a greater extent in group A (Agatston score ≥ 400) than in group B (Agatston score < 400). As the patients in the study were referred to ICA for suspected CAD, the prevalence of disease was high (75 %, with a mean calcium score of 483). The presence of dense calcium was the primary cause of false positives (40 of the 48 false-positive segments, 83 %), followed by coronary motion in six segments (13 %). This suggests that under the condition of a low radiation dose (i.e. reduced flux), the presence of calcium could impair the visualisation of the lumen and cause an overestimation of luminal stenosis even with the use of IR algorithms, indicating that we are at the limits of the resolution [27, 28].
Our result is consistent with the findings from an ex vivo human heart study by Scheffel et al. [29], wherein the authors reported improvements in overall IQ and CNR using a model-based IR technique compared with FBP, with the IQ getting uniformly worse in the presence of calcifications and no improvements achieved in the reduction of calcium blooming with the use of IR. On the other hand, Renker et al. [30] showed improvements in the diagnostic value of coronary CTA with IR versus FBP algorithms for severely calcified vessels, demonstrating improved accuracy with reduced blooming (significantly lower volumes of calcified plaques). This could be explained by the fact that their work focused more on the performance of an IR algorithm along with dedicated higher order reconstruction kernels in heavily calcified regions at routine tube output (effective radiation dose of 6.6 mSv), whereas our investigation focused more on the diagnostic performance of the IR algorithm with a conventional kernel (XCC), in coronary CTA performed at low tube outputs (i.e. effective radiation dose of 1.3 mSv).
Our study had 22 false-negative segments, again with calcium being the primary reason (18 segments, 82 %). We tried to take into account the presence of the calcium blooming while assessing the lesions and downgrading the degree of stenosis in these areas. The remaining false-negative segments (4) were caused by moderate motion artefacts; these segments were given a ranking of 2 (fair) on the 4-point scale.
The limitations of this study are as follows: (1) This was a single-centre study with a relatively small sample size. As the enrolled patients had already been referred to undergo ICA, this probably led to a selection bias of patients with a medium to high prevalence of disease (75 %)—this patient population is not typical of what was reported in the earlier coronary CTA literature. (2) We did not individually adapt the imaging protocol and reconstruction parameters based on the information from the calcium scoring images; for example we did not focus on image quality improvements (at the expense of a higher radiation dose) and investigate the potential benefits of using sharper reconstruction kernels in the reduction of blooming in the calcified areas. (3) We did not use a lower tube voltage (e.g. 100 kVp) in appropriate patients because we consider that the use of low tube voltage could also result in a larger proportion of the dose being absorbed by the body, potentially causing a higher degree of beam-hardening effects. Since reducing the tube current instead of the voltage only changes the effective flux and affects the x-ray penetration to a lesser extent, we used a conventional tube voltage (120 kVp) but with lower tube currents in this study.
In conclusion, the combination of low-dose prospectively ECG-triggered CTA with the IR technique can acquire satisfactory image quality and show high sensitivity, specificity and diagnostic accuracy in patients with suspected coronary heart disease; however with a high prevalence of disease in the study cohort, blooming continues to pose a challenge in the regions of severely calcified segments, re-emphasizing the importance of appropriate patient selection. Further investigations involving higher order reconstruction kernels need to be performed to optimise the image quality, especially in the presence of calcium.
References
Alkadhi H, Stolzmann P, Desbiolles L et al (2010) 128-slice, dual-source CT coronary angiography: accuracy and radiation dose of the high-pitch and the step-and-shoot mode. Heart 96:933–938
Carrascosa P, Capunay C, Deviggiano A et al (2010) Accuracy of low-dose prospectively gated axial coronary CT angiography for the assessment of coronary artery stenosis in patients with stable heart rate. J Cardiovasc Comput Tomogr 4:197–205
Kerl JM, Schoepf UJ, Zwerner PL et al (2011) Accuracy of coronary artery stenosis detection with CT versus conventional coronary angiography compared with composite findings from both tests as an enhanced reference standard. Eur Radiol 21:1895–1903
Sun ML, Lu B, Wu RZ et al (2011) Diagnostic accuracy of dual-source CT coronary angiography with prospective ECG-triggering on different heart rate patients. Eur Radiol 21:1635–1642
Hu XH, Zheng WL, Wang D, Xie SS, Wu R, Zhang SZ (2012) Accuracy of high-pitch prospectively ECG-triggering CT coronary angiography for assessment of stenosis in 103 patients: comparison with invasive coronary angiography. Clin Radiol 67:1083–1088
Zhang C, Zhang Z, Yan Z, Xu L, Yu W, Wang R (2011) 320-row CT coronary angiography: effect of 100-kV tube voltages on image quality, contrast volume, and radiation dose. Int J Cardiovasc Imaging 27:1059–1068
Hou Y, Yue Y, Guo W et al (2012) Prospectively versus retrospectively ECG-gated 256-slice coronary CT angiography: image quality and radiation dose over expanded heart rates. Int J Cardiovasc Imaging 28:153–162
Zhao L, Zhang Z, Fan Z, Yang L, Du J (2011) Prospective versus retrospective ECG gating for dual source CT of the coronary stent: comparison of image quality, accuracy, and radiation dose. Eur J Radiol 77:436–442
Dewey M, Zimmermann E, Deissenrieder F et al (2009) Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 120:867–875
Leipsic J, Labounty TM, Heilbron B et al (2010) Adaptive statistical iterative reconstruction: assessment of image noise and image quality in coronary CT angiography. AJR Am J Roentgenol 195:649–654
Bittencourt MS, Schmidt B, Seltmann M et al (2011) Iterative reconstruction in image space (IRIS) in cardiac computed tomography: initial experience. Int J Cardiovasc Imaging 27:1081–1087
Hou Y, Liu X, Xv S, Guo WL, Guo QY (2012) Comparisons of image quality and radiation dose between iterative reconstruction and filtered back projection reconstruction algorithms in 256-slice MDCT coronary angiography. AJR Am J Roentgenol 199:1–7
Leipsic J, Labounty TM, Heilbron B et al (2010) Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol 195:655–660
Park EA, Lee W, Kim KW et al (2012) Iterative reconstruction of dual-source coronary CT angiography: assessment of image quality and radiation dose. Int J Cardiovasc Imaging 28:1775–1786
Wang R, Schoepf UJ, Wu R et al (2012) Image quality and radiation dose of low dose coronary CT angiography in obese patients: Sinogram affirmed iterative reconstruction versus filtered back projection. Eur J Radiol 81:3141–3145
Funama Y, Taguchi K, Utsunomiya D et al (2011) Combination of a low-tube-voltage technique with hybrid iterative reconstruction (iDose) algorithm at coronary computed tomographic angiography. J Comput Assist Tomogr 35:480–485
Hou Y, Xv S, Guo WL, Vembar M, Guo QY (2012) The optimal dose reduction level using iterative reconstruction with prospective ECG-triggered coronary CTA using 256-slice MDCT. Eur J Radiol 81:3905–3911
Moscariello A, Takx RA, Schoepf UJ et al (2011) Coronary CT angiography: image quality, diagnostic accuracy, and potential for radiation dose reduction using a novel iterative image reconstruction technique-comparison with traditional filtered back projection. Eur Radiol 21:2130–2138
Noël PB, Fingerle AA, Renger B et al (2011) Initial performance characterization of a clinical noise-suppressing reconstruction algorithm for MDCT. AJR Am J Roentgenol 197:1404–1409
Austen WG, Edwards JE, Frye RL et al (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc committee for grading of coronary artery disease, council on cardiovascular surgery, American Heart Association. Circulation 51:5–40
McCollough C, Cody D, Edyvean S et al (2008) The measurement, reporting, and management of radiation dose in CT. Tech. Rep. 96 2008. American Association of Physicists in Medicine, College Park MD, USA
Earls JP, Berman EL, Urban BA et al (2008) Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology 246:742–753
Husmann L, Valenta I, Gaemperli O et al (2008) Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J 29:191–197
Klass O, Walker M, Siebach A et al (2010) Prospectively gated axial CT coronary angiography: comparison of image quality and effective radiation dose between 64- and 256-slice CT. Eur Radiol 20:1124–1131
Hara AK, Paden RG, Silva AC, Kujak JL, Lawder HJ, Pavlicek W (2009) Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study. AJR Am J Roentgenol 193:764–771
Sun Z, Ng KH (2012) Prospective versus retrospective ECG-gated multislice CT coronary angiography: a systematic review of radiation dose and diagnostic accuracy. Eur J Radiol 81:e94–e100
Park MJ, Jung JI, Choi YS et al (2011) Coronary CT angiography in patients with high calcium score: evaluation of plaque characteristics and diagnostic accuracy. Int J Cardiovasc Imaging 27:43–51
Meng L, Cui L, Cheng Y et al (2009) Effect of heart rate and coronary calcification on the diagnostic accuracy of the dual-source CT coronary angiography in patients with suspected coronary artery disease. Korean J Radiol 10:347–354
Scheffel H, Stolzmann P, Schlett CL et al (2012) Coronary artery plaques: cardiac CT with model-based and adaptive-statistical iterative reconstruction technique. Eur J Radiol 81:e363–e369
Renker M, Nance JW Jr, Schoepf UJ et al (2011) Evaluation of heavily calcified vessels with coronary CT angiography: comparison of iterative and filtered back projection image reconstruction. Radiology 260:390–399
Acknowledgements
The work presented was supported by government funding through the Shenyang Science and Technology Research Program (F12-193-9-35).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hou, Y., Ma, Y., Fan, W. et al. Diagnostic accuracy of low-dose 256-slice multi-detector coronary CT angiography using iterative reconstruction in patients with suspected coronary artery disease. Eur Radiol 24, 3–11 (2014). https://doi.org/10.1007/s00330-013-2969-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2969-9