Abstract
Objective
To evaluate the diagnostic accuracy of dual-source CT (DSCT) prospective ECG-triggering coronary angiography in patients with different heart rate (HR).
Methods
103 patients with suspected coronary artery disease underwent DSCT prospective ECG-triggered coronary angiography and invasive coronary angiography (ICA). The patients were grouped by HR during CT scans: low HR (≤60 bpm, n = 34); medium HR (60 < HR ≤ 70 bpm, n = 36) and high HR (>70 bpm, n = 33). The sensitivity and specificity of DSCT in detecting ≥50% stenosis were compared among subgroups where ICA was the gold standard. Image quality was scored using a 4-point scale.
Results
A total of 1,580 (95.9%) coronary artery segments were evaluable. Sensitivity and specificity were 82.8% and 98.4%, 88.3% and 98.7%, and 80.3% and 98.6% for different subgroups (all p > 0.05). The overall area under the curve of the receiver-operating characteristic analysis was 0.94. The image quality scores were 3.1 ± 0.3, 3.1 ± 0.3 and 3.0 ± 0.4 for subgroups (p > 0.05). The overall average effective radiation dose was 3.60 ± 1.60 mSv.
Conclusion
DSCT coronary angiography with prospective ECG-triggering could be just as accurate in patients with medium to high HR compared to those with low HR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) is one of the most common causes of death in the western world [1] and China [2]. Computed tomographic coronary angiography (CTCA) has become a widely-used diagnostic tool for CAD as a non-invasive examination with high accuracy and negative predictive value [3]. However, the radiation exposure associated with CTCA is still a concern in the community [4, 5]. To reduce the radiation burden, many dose-saving techniques have been developed [5, 6]. Among these techniques prospective ECG-triggering CTCA is considered a good method of significantly reducing patient dose from 10.7 to 18.9 mSv using retrospective ECG-gated to 2.8–3.8 mSv on 64 multi-detector row spiral CT (64-MDCT) [7–9]. On the dual-source CT (DSCT), prospective ECG-triggering sequential CTCA can accurately diagnose stenosis with a dose level at 2.5–2.9 mSv [4, 8], a dose saving of more than 65% compared with the 8.5–9.8 mSv using standard retrospective DSCT protocols [10, 11].
Recent studies using prospective ECG-triggering controlled patients’ HR to 70 bpm or lower in order to guarantee image quality and low dose [10, 12–14]. It has been shown that DSCT with two sets of image acquisition systems has doubled the temporal resolution to 83 ms, which allows CTCA examinations without requiring low HR [10, 15]. To date, however, fewer data are available to show the diagnostic accuracy of DSCT prospective triggering CTCA in high HR patients.
The purpose of this study was to assess the diagnostic accuracy and image quality of DSCT coronary angiography with prospective ECG-triggering in patients with low to high HR using invasive coronary angiography (ICA) as the reference.
Materials and methods
Patient population
From January 1st, 2009 to August 31st, 2009, a total of 155 consecutive patients who had undergone both DSCT coronary angiography and invasive coronary angiography (ICA) were enrolled in this study. Patients were referred for CTCA examinations to rule out coronary heart disease (CHD). The interval between DSCT coronary angiography and ICA was less than 30 days. The exclusion criteria of this study were as follows: CTCA were performed using retrospective ECG-gated scans (n = 37); the presence of coronary stents or implants (n = 12), coronary artery bypass grafts (n = 3). After the exclusion, 103 patients who underwent both DSCT prospective ECG-triggering coronary angiography and ICA were included for further analysis. The study protocol was approved by the Institutional Ethics Committee of the hospital. The written informed consent forms were signed by all patients for both CTCA and ICA examinations.
The patients were divided into three subgroups based on HR recorded during the CT scans; low HR, ≤60 bpm; medium HR, 60 < HR ≤ 70 bpm and high HR, >70 bpm. The patient demographics and the statistical comparison of three HR subgroups were given in Table 1.
DSCT data acquisition and post-processing
All imaging was performed with DSCT (SOMATOM Definition, Siemens Healthcare, Forchheim, Germany) using a commercial prospective ECG-triggering sequential protocol, and using the following parameters: collimation 2 × 32 × 0.6 mm; slice collimation 2 × 64 × 0.6 mm by using z-flying focal spot; gantry rotation 0.33 s; tube voltage 100 kV or 120 kV, and tube current 420–500 mAs adjusted by body mass index (BMI). The start phase of the CT data acquisition was 70% of the R-R interval when baseline HR was ≤70 bpm or 40% of the R-R interval when baseline HR was >70 bpm [16]. The acquisition window was 380 ms using flex padding which allows approximately ±8% R-R interval flexibility for image reconstruction. The image was reconstructed with slice thickness of 0.6 mm, slice increment of 0.3 mm and convolution kernel of B26. The cardiac phase in which least or no motion was seen was manually selected by reviewing the reconstructions at different cardiac phases (possible by using the padding acquisition window). All images were transferred to a commercial workstation (Multi-Modality Workplace, Siemens Healthcare, Forchheim, Germany) for further image processing and evaluation.
Oral beta-blockers were given to patients whose heart rate was higher than 90 bpm to achieve a HR ≤ 90 bpm and beat-to-beat HR change <10 bpm before CT scan. For patients whose HR could not be achieved ≤90 bpm or beat-to-beat HR change <10 bpm, the retrospective ECG-gated scan protocol was used. Nitroglycerine was not administered for CT angiography to align with the protocol of CT angiography used in our center.
Contrast agent (Omnipaque 350 mgI/ml, GE Healthcare, USA or Ultravist 370 mgI/ml, Bayers-Schering Pharma, Germany) was injected through a 20G catheter into the antecubital vein using a power injector (Stellant, Medrad, Indianola, PA, USA).
A tri-phase injection protocol was used; 50 ml of contrast agent (phase I) followed by 30 ml of diluted contrast (phase II; 30% contrast agent and 70% saline), and 40 ml of saline chaser (phase III). The injection rate was 4–5.5 ml per second adjusted according to the duration of the CT data acquisition which was automatically triggered to begin 6 s after the CT value reached 100 Hounsfield Units (HU) at the root of the ascending aorta.
The effective dose of the CTCA was calculated by multiplying the dose length product (DLP) by the conversion coefficient (k = 0.014 mSv/mGy∙cm) for the chest as previously suggested [11, 12]. The DLP and HR were taken from the patient protocol provided by the CT system.
DSCT data analysis
The 16-segment coronary artery schema suggested by American Heart Association (AHA) was used [10]. Segments with a visual diameter of <1.5 mm at the origin were not included. Two experienced readers (with more than 10 years of experience in cardiac radiology) assessed the CTCA images independently without knowledge of the patient clinical history and ICA results. In the event of a discrepancy between the two reviewers, a joint reading session was used to reach a consensus. All images were analysed in the axial view, multiplanar reformation (MPR) and maximum intensity projection (MIP) on a per-segment, per-vessel basis. A segment was classified as stenotic when lumen narrowing exceeded 50%.
Image quality of a vessel was scored on a 4-point scale; 1, non-discriminable vessel structure or poor image quality with severe artefact; 2, moderate artefact but assessable on the axial images; 3, good image quality with minor artefact; 4, excellent image quality [7]. The score of one was considered to be non-diagnostic. The scheme of vessels was left main (LM), left anterior descending (LAD), left circumflex (LCX) and right coronary artery (RCA). The overall score of a vessel was given by assigning the lowest segment score of that vessel.
Invasive coronary angiography
The ICA was performed using standard angiographic techniques. ICA data were reviewed by two experienced observers (>10 years’ experience), who were blinded to the result of DSCT and patient clinical history. At least two orthogonal projections were used to determine the degree of stenosis. Additional projections were used if necessary. Coronary luminal stenosis in diameter was analysed and recorded visually by two reviewers. In the event of a discrepancy between the two reviewers, the same procedure was followed as described for DSCT above. As for the CTCA data analysis, the coronary arteries were named according to the AHA model and segments with diameter of <1.5 mm at the origin were excluded from the analysis.
Statistical analysis
Statistical analyses were performed using a commercial software package (SPSS 17.0 for windows, SPSS, Chicago, IL, USA). The analysis of variance (ANOVA) and Kruskal-Wallis analysis were used for continuous interval data with normal distribution and ordinal data with non-normal distribution, respectively. A binomial-based proportion analysis was used for patient characteristic data. The sensitivity, specificity and accuracy of CTCA were calculated and the differences were compared by using the χ 2 test of contingency on a per-segment and per-vessel basis. ICA was taken as the gold standard. Interobserver agreement of CTCA assessment was performed using kappa analysis (<0.4, poor agreement; 0.4–0.75, fair to good agreement; >0.75, excellent agreement). We performed a receiver-operating characteristic (ROC) analysis to compare the diagnostic power of CTCA to the CHD patients in different HR subgroups. The area under the curve (AUC) between 0.5 and 0.70 suggests the limited diagnostic power, AUC 0.70–0.90 means moderate diagnostic power and AUC >0.90 means strong diagnostic power. A p value of <0.05 was considered to be statistically significant.
Results
One hundred and three patients (65 men, 38 women, mean age and standard deviation were 58.5 ± 10.6 years, range 32–83 years) successfully underwent both DSCT prospective ECG-triggering coronary angiography and ICA examinations. In the low HR group (n = 34), the mean HR was 54.2 ± 3.9 (range 44–59, median, 54.5) bpm; in the medium HR group (n = 36), the mean HR was 64.4 ± 2.5 (range 60–69, median, 64.5) bpm and in the high HR group (n = 33), the mean HR was 79.1 ± 7.2 (range 71–96, median, 79.0) bpm. The mean calcium scores in the low, medium and high HR subgroups were 139.5 (range 0–837.1), 263.5 (range 0–1,187) and 143.6 (range 0–1000.5), respectively. As shown in Table 1, the HR variability, calcium score, days between CTA and ICA, and other patient characteristics were not significantly different among three HR subgroups.
Invasive coronary angiography
Overall, invasive coronary angiography (ICA) demonstrated that 10 out of 103 patients (9.7%) had no coronary heart disease (CHD), 38 (36.9%) patients with one-vessel CHD, 23 (22.3%) patients with two-vessel CHD and 32 (31.0%) patients with three-vessel CHD. The distribution of CHD patients and statistical analyses among subgroups are shown in Table 2.
DSCT prospective ECG-triggering coronary angiography
On a per-patient-based analysis in this group, prospective ECG-triggered coronary sequential DSCT provided analysable image quality of the coronary vessels in 102 (99%) of the 103 patients. There was one non-analysable case in the medium HR group in which the patient had a severe artefact caused by abrupt HR change during CT data acquisition. In a total of 1,648 segments, image quality was analysable in 1,580 segments (95.9%). Sixty-eight segments were not assessed for the following reasons: 26 segments were <1.5 mm at the origin; 25 segments were not sufficiently opacified because of proximal stenosis or occlusion; 13 segments were affected by diffusive calcium blooming artefact; three segments had motion artefact; and one segment was affected by severe stair-step artefact. In 13 patients of low HR (one case, 2.9%), medium HR (four cases, 11.1%) and high HR (eight cases, 24.2%), additional reconstructions were made within the range allowed by the flex padding to improve image quality.
An inter-reader reliability analysis using the Kappa statistic was performed to determine consistency among readers. The inter-reader Kappa values of the low, medium and high HR subgroups were 0.853 (95% CI = 0.790–0.916), 0.864 (95% CI = 0.807–0.921) and 0.830 (95% CI = 0.754–0.906), respectively.
In overall subjects of this study, the diagnostic sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV) on a segmental basis were 84.3%, 98.6%, 96.1%, 92.2% and 96.9%, respectively; whereas positive and negative test likelihood ratios were 60.2 and 0.16, respectively. No significant differences were found among low, medium and high HR subgroups in a comparison of diagnostic values (Table 3, Figs. 1 and 2).
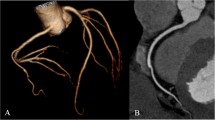
A 71-year-old male patient (body mass index of 27.2 kg/m2, baseline heart rate of 93 bpm) underwent DSCT using prospective ECG-triggering coronary angiographic protocols. Stenoses on the right coronary artery (Arrows) were demonstrated on images of curved multiplanar reformation (A) and volume rendering techniques (B). The same lesion was visualised on the reference standard of invasive coronary angiography (C). The effective radiation dose for this patient was 6.0 mSv
A 49-year-old female patient (body mass index of 22.9 kg/m2, baseline heart rate of 77 bpm) underwent DSCT using prospective ECG-triggering coronary angiographic protocols. Stenoses on the left anterior descending (Arrows) were demonstrated on images of maximum intensity projection (A) and volume rendering techniques (B). The same lesion was visualised on the reference standard of invasive coronary angiography (C). The effective radiation dose for this patient was 3.6 mSv
On receiver-operating characteristic (ROC) analysis, the area under the curve (AUC) for this study was 0.94 (95% CI = 0.92–0.96). For the low, medium and high HR groups, the AUCs were 0.97 (95% CI = 0.94–0.99), 0.94 (95% CI = 0.90–0.97) and 0.92 (95% CI = 0.87–0.97), respectively. There were no significant differences among HR subgroups with regard to AUC (p < 0.001) (Fig. 3).
Receiver-operating characteristic curves for overall group (A), low, medium, and high HR groups (B). These data demonstrated that similar diagnostic performances of DSCT coronary angiography with prospective ECG-triggering were found in different heart rate patients for detection of >50% coronary stenosis
The image quality scores on a per-vessel basis were shown in Table 4. The mean and standard deviation (SD) for different vessels were compared in subgroups. The differences were not significant (all p > 0.05) among the subgroups. The lowest score occurred for the LCX in each HR subgroup.
The mean effective doses were 3.40 ± 1.50 mSv (range: 0.95–6.06 mSv), 3.59 ± 1.12 mSv (range: 1.85–6.15 mSv) and 3.84 ± 2.15 mSv (range: 1.02–8.92 mSv) in these three HR subgroups, respectively. No significant differences were found among low, medium and high HR subgroups (F = 0.383, p = 0.684). The mean effective dose for overall subjects in this group was 3.60 ± 1.60 mSv (range: 0.95–8.92 mSv).
Discussion
Prospective ECG-triggering imaging markedly decreases CTCA radiation dose compared with retrospective ECG-gated imaging. Reported effective doses of patients with low heart rates for prospective CTCA were 2.1–4.3 mSv on 64-slice CT [14, 17, 18], and 2.1–2.5 mSv on DSCT in the step-and-shoot mode [13]. However, the favourable heart rates of prospective CTCA in the above-mentioned studies were limited to 70 bpm or 65 bpm. To benefit higher HR patients with low-dose prospective CTCA, we investigated the diagnostic performance of DSCT prospective ECG-triggering coronary angiography in patients with low to high HR using ICA as a reference.
Retrospective ECG-gated DSCT coronary angiography has been shown to provide high image quality without heart rate modulation by oral or intravenous administration of β-blockers before CT imaging procedure [19–22]. Our previous study indicated that at the end of systole or at the start of isovolumetric relaxation (before the rapid-filling phase), coronary motion changes direction and its velocity is theoretically zero, and that coronary artery motion varied significantly throughout the cardiac cycle and from patient to patient, due to different heart rates [23]. Isovolumetric relaxation duration of low HR patients is relatively longer than that of higher HR patients. For that reason, previous prospective DSCT coronary angiography (step-and-shoot mode) needs HR ≤ 70 bpm to achieve stable higher image quality [10–13, 24].
Our data indicated that sequential DSCT with a novel developed prospective ECG-triggering (flex padding technique) provided diagnosable coronary image quality in 99% patients, and there were no significant differences among low, medium and high HR groups (the mean HR was 79.1 bpm, range 71–96 bpm). In addition, the present study showed that the main reasons for severely affected image quality were less engorgement of the distal artery after the obstructed lesion, diffuse calcification, thin and small vessels, motion artefacts or misregistration artefacts. Among the four main coronary artery branches, the ordination order of image quality scores from high to low was that LM>RCA>LAD>LCX. It was comparable to the result reported by the literature [18].
Retrospective ECG-gated CTCA had shown diagnostic sensitivity of 90–97.8% and specificity of 86.8–99.2% [21, 22, 25], but these caused additional radiation exposure for the patient. Previous studies with prospective ECG-triggering (step-and-shoot mode) had shown sensitivity of 100% and specificity of 83.3%–93% in patients with HR ≤ 70 bpm or 65 bpm [13, 14].
The heart rates of patients enrolled in our study ranged from 44 bpm to 96 bpm. We found that prospective ECG-triggering DSCT coronary angiography provided similar diagnostic accuracy and efficacy in detecting ≥50% stenosis in patients with different heart rates. Diagnostic sensitivity, specificity, accuracy and image quality were not significantly different from the low to high heart rate groups. Overall, the prospective imaging yielded diagnosable image quality in 95.9% coronary segments with a sensitivity of 84.3%, specificity of 98.6% and accuracy of 96.1% for detecting significant coronary luminal stenosis. The areas under the curve of ROC analyses also showed no significant difference from the low to the high heart rate group, confirming that the prospective ECG-triggering imaging protocol of DSCT could be used in patients with a relatively high heart rate without sacrificing diagnostic efficacy.
Reported effective dose for prospective CTCA were 2.1–4.3 mSv on 64-slice CT [14, 17, 18], and 2.1–2.5 mSv on DSCT [13]. In this study the mean effective dose was 3.60 mSv (range 0.95–8.92 mSv), which remains a slightly high dose compared with that using the step-and-shoot mode, because flex padding technique (acquisition of additional phases) was used in this study, which would lead to increased radiation dose compared with single-phase acquisition to achieve a similar high proportion of vessels with diagnostic image quality. On the other hand, the wider acquisition window (flex padding technique) allowed data reconstruction from a wider R-R phase, improving the chance of good image quality for the coronary arteries in patients with a fast heart rate. The dosage in our study was sharply decreased compared with retrospective ECG-gated CTCA on DSCT [10], or invasive coronary angiography [26].
Clinically, there were a number of patients with irregular heart rates or heart rate >90 bpm. In this study, the reason that we gave oral beta-blockers to patients with baseline heart rate higher than 90 bpm was that prospective ECG-triggering could not be performed in such patients because of the potential failure or unpredictable image quality. The latest generation of DSCT system could further reduce radiation dose and improve image quality by using a high-pitch prospective ECG-triggering technique. Improved temporal resolution (75 ms) was a promising solution for the diagnostic accuracy of coronary CTA in patients with an irregular or high heart rate.
Our study had limitations. Patient enrolled in this study had high prevalence of diseased coronary artery, which may lead to under-estimation of sensitivity and negative prediction value. This was caused by most of our patients with negative findings on CTCA were not involved in the invasive catheter procedure. Patients with irregular heart rates were excluded, especially on atrial fibrillation or premature ventricular contraction.
In conclusion, DSCT coronary angiography with prospective ECG-triggering could be performed and provided accurate diagnosis for detecting ≥50% stenosis in patients with low, medium and high heart rates, while the average radiation dose was relatively low.
References
Donald LJ, Robert JA, Todd MB et al (2010) Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation 121:948–954
Gaziano TA (2007) Reducing the growing burden of cardiovascular disease in the developing world. Health Aff 26:13–24
Bastarrika G, Lee YS, Huda W et al (2009) CT of coronary artery disease. Radiology 253:317–338
Einstein AJ, Henzlova MJ, Rajagopalan S (2007) Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 298:317–323
Ketelsen D, Thomas C, Werner M et al (2010) Dual-source computed tomography: estimation of radiation exposure of ECG-gated and ECG-triggered coronary angiography. Eur J Radiol 73:274–279
Schoenhagen P (2008) Back to the future: coronary CT angiography using prospective ECG triggering. Eur Heart J 29:153–154
Ko SM, Kim NR, Kim DH et al (2010) Assessment of image quality and radiation dose in prospective ECG-triggered coronary CT angiography compared with retrospective ECG-gated coronary CT angiography. Int J Cardiovasc Imaging 26:93–101
Klass O, Jeltsch M, Feuerlein S et al (2009) Prospectively gated axial CT coronary angiography: preliminary experiences with a novel low-dose technique. Eur Radiol 19:829–836
Earls JP, Berman E, Urban BA et al (2008) Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology 246:742–753
Alkadhi H, Stolzmann P, Scheffel H et al (2008) Radiation dose of cardiac dual-source CT: the effect of tailoring the protocol to patient-specific parameters. Eur J Radiol 68:385–391
Pflederer T, Jakstat J, Marwan M et al (2010) Radiation exposure and image quality in staged low-dose protocols for coronary dual-source CT angiography: a randomized comparison. Eur Radiol 20:1197–1206
Hein F, Meyer T, Hadamitzky M et al (2009) Prospective ECG-triggered sequential scan protocol for coronary dual-source CT angiography: initial experience. Int J Cardiovasc Imaging 25:231–239
Scheffel H, Alkadhi H, Leschka S et al (2008) Low-dose CT coronary angiography in the step-and-shoot mode: diagnostic performance. Heart 94:1132–1137
Herzog BA, Husmann L, Burkhard N et al (2008) Accuracy of low-dose computed tomography coronary angiography using prospective electrocardiogram-triggering: first clinical experience. Eur Heart J 29:3037–3042
Achenbach S, Anders K, Kalender WA (2008) Dual-source cardiac computed tomography: image quality and dose considerations. Eur Radiol 18:1188–1198
Srichai MB, Hecht EM, Kim D et al (2009) Dual-Source computed tomography angiography image quality in patients with fast heart rates. J Cardiovasc Comput Tomogr 3:300–309
Maruyama T, Takada M, Hasuike T et al (2008) Radiation dose reduction and coronary assessability of prospective electrocardiogram-gated computed tomography coronary angiography: comparison with retrospective electrocardiogram-gated helical scan. J Am Coll Cardiol 52:1450–1455
Husmann L, Valenta I, Gaemperli O et al (2008) Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J 29:191–197
Alkadhi H, Scheffel H, Desbiolles L et al (2008) Dual-source computed tomography coronary angiography: influence of obesity, calcium load, and heart rate on diagnostic accuracy. Eur Heart J 29:766–776
Rixe J, Rolf A, Conradi G et al (2008) Image quality on dual-source computed-tomographic coronary angiography. Eur Radiol 18:1857–1862
Rixe J, Rolf A, Conradi G et al (2009) Detection of relevant coronary artery disease using dual-source computed tomography in a high probability patient series: comparison with invasive angiography. Circ J 73:316–322
Ropers U, Ropers D, Pflederer T et al (2007) Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J Am Coll Cardiol 50:2393–2398
Lu B, Mao SS, Zhuang N et al (2001) Coronary artery motion during the cardiac cycle and optimal ECG triggering for coronary artery imaging. Invest Radiol 36:250–256
Lell M, Marwan M, Schepis T et al (2009) Prospectively ECG-triggered high-pitch spiral acquisition for coronary CT angiography using dual source CT: technique and initial experience. Eur Radiol 19:2576–2583
Xu Y, Tang LJ, Zhu XM et al (2010) Comparison of dual-source CT coronary angiography and conventional coronary angiography for detecting coronary artery disease. Int J Cardiovasc Imaging 26:75–81
Herzog BA, Wyss CA, Husmann L et al (2009) First head-to-head comparison of effective radiation dose from low-dose 64-slice CT with prospective ECG-triggering versus invasive coronary angiography. Heart 95:1656–1661
Acknowledgement
This study was granted by the Ministry of Science and Technology of China, Grant NO. 2007BAI05B02.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, Ml., Lu, B., Wu, Rz. et al. Diagnostic accuracy of dual-source CT coronary angiography with prospective ECG-triggering on different heart rate patients. Eur Radiol 21, 1635–1642 (2011). https://doi.org/10.1007/s00330-011-2107-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2107-5