Abstract
Objectives
To evaluate the diagnostic performance of shear-wave elastography (SWE) for breast cancer and to determine whether the integration of SWE into BI-RADS with subcategories of category 4 improves the diagnostic performance.
Methods
A total of 389 breast masses (malignant 120, benign 269) in 324 women who underwent SWE before ultrasound-guided core biopsy or surgery were included. The qualitative SWE feature was assessed using a four-colour overlay pattern. Quantitative elasticity values including the lesion-to-fat elasticity ratio (Eratio) were measured. Diagnostic performance of B-mode ultrasound, SWE, or their combined studies was compared using the area under the ROC curve (AUC).
Results
AUC of Eratio (0.952) was the highest among elasticity values (mean, maximum, and minimum elasticity, 0.949, 0.939, and 0.928; P = 0.04) and AUC of colour pattern was 0.947. AUC of combined studies was significantly higher than for a single study (P < 0.0001). When adding SWE to category 4 lesions, lesions were dichotomised according to % of malignancy: 2.1 % vs. 43.2 % (category 4a) and 0 % vs. 100 % (category 4b) for Eratio and 2.4 % vs. 25.8 % (category 4a) for colour pattern (P < 0.05).
Conclusions
Shear-wave elastography showed a good diagnostic performance. Adding SWE features to BI-RADS improved the diagnostic performance and may be helpful to stratify category 4 lesions.
Key points
• Quantitative and qualitative shear-wave elastography provides further diagnostic information during breast ultrasound.
• The elasticity ratio (E ratio ) showed the best diagnostic performance in SWE.
• E ratio and four-colour overlay pattern significantly differed between benign and malignant lesions.
• SWE features allowed further stratification of BI-RADS category 4 lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Breast elastography as a method of imaging tissue stiffness has been used to improve diagnostic confidence and increase specificity of the ultrasound interpretation. The recently developed shear-wave elastography (SWE; Supersonic Imagine, Aix-en-Provence, France) uses the acoustic radiation force induced by the ultrasound beam itself. This force induces mechanical waves, including shear waves, which propagate transversely in the tissue. Because the speed of shear waves is measured, SWE is able to provide quantitative elastic information expressed as the Young’s modulus or displayed as a colour overlay of the lesion and surrounding tissue in real time [1, 2].
Several studies in which SWE was used have demonstrated that using quantitative Young’s modulus of elasticity (kPa), and qualitative colour shear-wave elastographic features were useful differentiating benign from malignant breast lesions [2–7]. Moreover, the addition of SWE to the Breast Imaging Reporting and Data System (BI-RADS) classification [8] improved the diagnostic performance for breast cancer compared to the BI-RADS alone [2, 4–7]. Although the ultrasound BI-RADS lexicon has been proved to be an efficient and consistent system [9–12], BI-RADS category 4 lesions recommended for biopsy have a broad range for the likelihood of malignancy of 2 % – 95 % by definition. Therefore, they were subdivided into categories 4a, 4b, and 4c, which were useful in stratifying the likelihood of malignancy among the large heterogeneous group of category 4 lesions and communicating the level of suspicion to referring physicians and patients [10]. In most previous SWE studies, however, the subcategories of category 4 were not considered. Although Berg et al. reported that the addition of SWE features could reduce unnecessary biopsies of BI-RADS category 4a lesions, the study was performed with the prototypic ultrasound system equipped with SWE [6].
The purpose of this study was to evaluate the diagnostic performance of commercially available SWE for breast cancer and to determine whether the integration of SWE into BI-RADS classification with subcategories of category 4 improves the diagnostic performance for breast lesions.
Patients and methods
This retrospective study was conducted with institutional review board approval and a waiver of patient informed consent.
Patients and lesions
From May 2011 to October 2011, 332 consecutive patients underwent SWE before ultrasound-guided core needle biopsy (CNB) or surgical excision for breast lesions visible on ultrasound. Among these patients, 324 women aged 22–87 years (mean, 46.0 ± 11.4 years) with a total of 389 breast lesions were enrolled in this study. The remaining eight women who underwent neoadjuvant chemotherapy at the time of SWE were excluded from this study. One hundred five patients (27.6 %) had the following symptoms: palpable mass (n = 101) and nipple discharge (n = 4). The remaining patients were asymptomatic.
At our institution, ultrasound-guided 14-gauge CNB is initially performed for breast masses visible on ultrasound that have been prospectively assigned to the BI-RADS category 4 or 5 and, at the request of patients or referring physicians, BI-RADS category 3 masses. For imaging-pathology correlation after CNB, follow-up ultrasound was recommended in patients with concordant benign lesions and surgical excision in the others. At the request of the patient or referring physician, repeat biopsies were carried out for some concordant benign lesions by surgical excision or ultrasound-guided vacuum-assisted biopsy depending on the preferences of the physician and patient.
Ultrasound examinations
The breast ultrasound examinations were performed with the Aixplorer ultrasound system (SuperSonic Imagine, Aix-en-Provence, France) equipped with a 4–15-MHz linear-array transducer, by one of four radiologists with 5–10 years of experience in breast ultrasound. The investigator knew the results of clinical examination and mammography at the time of the ultrasound examination. For the lesions that were scheduled to be biopsied or excised surgically, the radiologists who performed the breast ultrasound recorded the lesion diameter (measured as the maximal diameter of the lesion), distance from the nipple (measured as the distance from the nipple to the closest margin of the lesion), lesion depth (measured as the vertical diameter from the skin to the centre of the lesion), and breast thickness (measured as the vertical diameter from the skin to the pectoralis muscle) where the lesion was located. Measurements were performed with light pressure by using a probe with the same method as that used for elastography [13]. After B-mode ultrasound, SWE images were obtained for the breast lesions that were scheduled to be biopsied or excised surgically. The built-in region of interest (ROI) (Q-box; SuperSonic Imagine) of the system was set to include the lesion and the surrounding normal tissue, which was demonstrated on a semitransparent colour map of tissue stiffness overlaid on the B-mode image with a range from dark blue, indicating the lowest stiffness, to red, indicating the highest stiffness (0–180 kPa). Areas of black on the SWE images represented tissue in which no shear wave was detected. Fixed 2 × 2-mm ROIs were placed by an investigator over the stiffest part of the lesion, including the immediate adjacent stiff tissue or halo. A second ROI of the same size was placed in the breast fatty tissue. This allowed calculation of the ratio between the mean elasticity values in the lesion and in the fat, called the elasticity ratio (Eratio). The system calculated the minimum (Emin), maximum (Emax), and mean elasticity values (Emean) in kPa as well as Eratio for the mass.
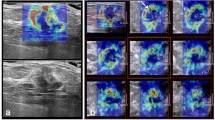
Image evaluation
Each ultrasound image was reviewed independently by a single breast radiologist with 10 years of experience in breast ultrasound. During the review session, the radiologist was blinded to clinical, mammographic, and pathological findings. A two-step sequential reading was performed by using the two data sets consisting of B-mode ultrasound and SWE with a 4-week interval between each reading session. The order of cases within each reading session was randomised to reduce bias. Regarding B-mode ultrasound, representative transverse and longitudinal images for each lesion were reviewed and ultrasound BI-RADS final assessment categories were assigned, including categories 3, 4a, 4b, 4c, or 5 [8]. Regarding the SWE, a representative opaque SWE colour overlay image with the underlying B-mode image was shown. In all SWE images for review, no quantitative information (elasticity value) was included. SWE colour overlay patterns were assessed using the four-colour overlay pattern proposed by Tozaki et al. [4]. When no difference from the colour around the lesion was observed at the margin of the lesion or in its interior (coded blue homogeneously), the image was classified as ‘no findings’ (pattern 1) (Fig. 1). When a colour that differed from the colour around the lesion was observed at the margin or in the interior of the lesion, but it extended beyond the lesion and continued vertically in cords on the cutaneous side or the thoracic wall side, it was concluded to be an artefact unique to SWE and classified as a negative finding (pattern 2) (Fig. 2). On the other hand, when a localised coloured area was present at the margin of the lesion, it was classified as a positive finding (pattern 3) (Fig. 3). When coloured areas were present in the interior of the lesion heterogeneously, it was classified as a positive finding (pattern 4) (Fig. 4).
Shear-wave elastography and B-mode images on split-screen mode in a 41-year-old woman. Left: B-mode image shows a 7-mm, oval, ill-defined mass (arrows) considered to be BI-RADS category 4a. Right: Elastogram shows the lesion and the surrounding tissue coded blue homogeneously considered to be pattern 1, with Eratio of 3.24. On the basis of the benign appearance on the shear-wave elastographic image, this mass could have been considered BI-RADS category 3. Biopsy showed fibroadenoma
Shear-wave elastography and B-mode images on split-screen mode in a 23-year-old woman. Left: B-mode image shows an 11-mm, irregular, ill-defined mass (arrows) considered to be BI-RADS category 4c. Right: Elastogram shows light green vertically striped pattern (arrows) considered to be pattern 2, with Eratio of 1.13. The diagnosis after surgical excision was fibrocystic change
Shear-wave elastography and B-mode images on split-screen mode in a 63-year-old woman. Left: B-mode image shows a 5-mm, round, microlobulated mass (arrows) considered to be BI-RADS category 4a. Right: Elastogram shows localised coloured area (arrow) at the margin of the lesion considered to be pattern 3, with Eratio of 11.04. The diagnosis after surgical excision was ductal carcinoma in situ
Shear-wave elastography and B-mode images on split-screen mode in a 53-year-old woman. Left: B-mode image shows a 7-mm, oval, hypoechoic mass with angular margin (arrows) considered to be BI-RADS category 4a. Right: Elastogram shows coloured areas present in the interior of the lesion heterogeneously considered to be pattern 4, with Eratio of 10.1. Biopsy showed invasive ductal carcinoma
Data and statistical analysis
After review of medical records, clinical and radiological variables for each examination were coded using the Excel spreadsheet (Microsoft Excel 2010, Washington, USA). The collected clinical variables were patient age and associated symptom of palpable mass. For radiological variables, breast density on mammography based on BI-RADS category was noted. For B-mode ultrasound, the following variables were determined: the lesion diameter (measured as the maximal diameter of the lesion), distance from the nipple (measured as the distance from the nipple to the closest margin of the lesion), lesion depth (measured as the vertical diameter from the skin to the centre of the lesion), and breast thickness (measured as the vertical diameter from the skin to the pectoralis muscle) where the lesion was located. For SWE, quantitative values of Emin, Emax, Emean, and Eratio for the mass on SWE were collected.
Clinical, radiological, B-mode, and SWE features were compared statistically between benign and malignant lesions by using the χ2 test for categorical variables and the Mann–Whitney U test for continuous variables. To determine the best-performing SWE features and to compare the diagnostic performance of B-mode ultrasound and SWE, we calculated and compared the area under the receiver operating characteristic (ROC) curve (AUC) and generated a confidence interval (CI) by using the DeLong method [14]. Logistic regression analysis with odds ratio estimates and 95 % CI was used to determine whether the elasticity value or colour overlay pattern at SWE was independently associated with malignant breast lesions considering clinical, radiological, and ultrasound features and to perform ROC curve analysis by calculating the probability of malignancy of lesions in combined B-mode ultrasound and SWE. Statistical analysis was performed with a statistical software programme (SAS, version 9.1.3, SAS Institute Inc., Cary, NC, USA). Differences were considered to be statistically significant at P < 0.05.
Results
Of the 389 lesions, 120 (30.8 %; 28 for CNB and 92 for surgery) were malignant and 269 (69.2 %; 229 for CNB and 40 for surgery) were benign. The pathology of lesions was confirmed after ultrasound-guided CNB (14-gauge gun biopsy in 252 or 8-or 11-gauge vacuum-assisted biopsy in 5) (n = 257) or surgical excision (n = 132). The details of pathology are summarised in Table 1.
Clinicoradiological features
The patient age, associated symptoms of the palpable mass, and breast density on mammography were significantly different between benign and malignant lesions (Table 2). Patients with malignant lesions were likely to be older and associated with a palpable mass. On B-mode ultrasound, malignant lesions were likely to be larger, located in thicker and deeper areas, and farther from the nipple (Table 2). A significant difference in the percentage of malignant lesions was found in accordance with the ultrasound BI-RADS category (Table 2).
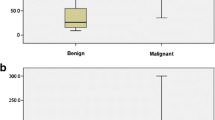
Quantitative analysis: elasticity values
Regarding elasticity values calculated at SWE, all values showed significant differences between benign and malignant breast lesions (Table 2). In ROC curve analysis, the AUC was 0.949 (95 % CI: 0.924, 0.974) for Emean, 0.939 (95 % CI; 0.912, 0.966) for Emax, 0.928 (95 % CI: 0.897, 0.959) for Emin, and 0.952 (95 % CI: 0.930, 0.975) for Eratio, among which the AUC of Eratio was the highest with the optimal cutoff value of 5.14 (sensitivity, 88.0 %; specificity, 90.6 %; P = 0.036).
At logistic regression analysis, Eratio showed a significant difference between benign and malignant breast lesions, irrespective of clinicoradiological features (patient age, associated symptom of palpable mass, and breast density on mammography) and ultrasound features (lesion diameter, distance from the nipple, lesion depth, breast thickness, and BI-RADS final assessment category) (Table 3).
Qualitative analysis: colour overlay pattern
On SWE, the four-colour overlay pattern showed a significant difference in the percentage of malignant lesions (P < 0.0001) (Table 2). In ROC curve analysis, the AUC was 0.947 (95 % CI: 0.923, 0.971), and with the cutoff of pattern 3, the AUC was 0.859 (sensitivity, 94.2 %; specificity, 77.7 %; P < 0.0001). At logistic regression analysis, the four-colour overlay pattern with the cutoff of pattern 3 showed significant difference between benign and malignant breast lesions, irrespective of clinicoradiological features (patient age, associated symptom of palpable mass, and breast density on mammography) and ultrasound features (lesion diameter, distance from the nipple, lesion depth, breast thickness, and BI-RADS final assessment category) (Table 4).
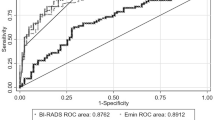
Comparison of diagnostic performance: B-mode ultrasound, SWE, and combined B-mode ultrasound and SWE
Regarding B-mode ultrasound, the AUC for BI-RADS final assessment category was 0.925 (95 % CI: 0.896, 0.955) and with the cutoff of category 4b, 0.891 (95 % CI: 0.855, 0.927) (sensitivity, 83.3 %; specificity, 94.8 %). Regarding SWE, the difference in the AUC was not significant between the quantitative Eratio (AUC, 0.952) and qualitative colour overlay pattern (AUC, 0.947) (P = 0.699).
In comparison of the AUC between B-mode ultrasound (0.891, with the cutoff of category 4b) and SWE (0.893, with the cutoff of 5.14 for Eratio; 0.859, with the cutoff of pattern 3 for colour overlay pattern), there was no significant difference (B-mode ultrasound vs. Eratio, P = 0.911; B-mode ultrasound vs. colour overlay pattern, P = 0.159) (Fig. 5). Regarding combined B-mode ultrasound and SWE, the AUC for combined studies was significantly higher than that for B-mode ultrasound or SWE (P < 0.0001) (Fig. 5). When adding SWE features to B-mode ultrasound for BI-RADS final assessment category 4 lesions, category 4a and 4b lesions were further stratified according to the percentage of malignancy. Adding colour overlay pattern to category 4a lesions showed 2.4 % of malignancy rate in pattern 1 and 2 lesions and 25.8 % of malignancy rate in pattern 3 and 4 lesions (P < 0.0001). Adding Eratio to category 4 lesions with the cutoff value of 5.14 showed the percentages of malignancy as follows: 2.1 % vs. 43.2 % for category 4a (P < 0.0001) and 0 % vs. 100 % for category 4b (P = 0.0009) (Table 5) (Figs. 1–4).
Discussion
Among quantitative values of the lesion stiffness measured at SWE, Eratio showed the highest AUC in diagnosing breast cancer with statistical significance (AUC, 0.952; P = 0.036). In the initial studies, mean elasticity values (Emean) were used empirically to differentiate breast lesions [2, 5]. However, elasticity values (e.g. Emax, Emin, Eratio, or standard deviation of elasticity) other than Emean have also shown a significant difference between benign and malignant breast lesions [3, 6]. In the clinical setting, variations in the SWE probe pressure might induce significant variations in the ROI calculation [15]. Barr et al. [16] reported that precompression–the amount of pressure applied to the tissue when performing ultrasound–changed the elastic properties of the tissue, making the tissue stiffer. Under substantial precompression of > 25 %, a benign lesion may have a velocity suggestive of a malignant lesion. However, fat tissue was similar in the rate of change in velocity to breast lesions and the elasticity ratio (Eratio) of the target tissue to the reference adjacent fat tissue can be expected to reduce the effect of precompression on the elastic properties of the tissue. In this context, Eratio was thought to show the best diagnostic performance in our study. Comparing with the previous study [6], the median of Eratio for benign (2.0; interquartile range, 4.4–10.7) and malignant lesions (7.8; interquartile range, 5.1–12.4) (P < 0.001) and the AUC of combined B-mode ultrasound and Eratio (0.960) were similar to those in our study.
Regarding qualitative analysis in SWE, Tozaki et al. proposed a four-colour overlay pattern classification for which lesions were assessed on the basis of colour stiffness and heterogeneity of the breast lesion at a time [4]. Pattern 3 or 4 in Tozaki’s classification reflected well a distinctive colour-map feature noted in many malignancies: a rim of surrounding relative stiffness but softer centre (Fig. 3) [3, 6]. During SWE, unexpected and unintentional artefactual vertical bands of stiffness were present, particularly with superficial masses (Fig. 2) [4, 6]. To avoid erroneous interpretation by this artefact, the vertical stripe pattern of artefacts (pattern 2) was introduced. In our study, 30.3 % (118 of 389) of cases were assessed as pattern 2 at SWE and 6 of them (5.1 %) were malignant. In the study by Tozaki et al. [4], 14 % (14 of 100) of patients were assessed as pattern 2 and the percentage of malignancy in pattern 2 was 14.3 %. Considering the difference in the proportion of malignant lesions (70 % vs. 30 %), our result would be consistent with that of Tozaki and the introduction of pattern 2 might be useful to reduce possible false positives.
In contrast with static elastography, SWE is known to measure local tissue elasticity almost independently from adjacent tissues and it is theoretically insensitive to target size [15]. However, the tumor size was reported to affect elasticity values. According to Evans et al. [3], invasive cancers with an ultrasound size of < 15 mm had an average mean elasticity of 109 kPa compared with an average of 167 kPa for lesions ≥ 15 mm. However, even small cancers, which are not as stiff as larger cancers, showed higher stiffness values than benign lesions did. Another study reported that the average mean elasticity values were higher in the larger masses for both benign and malignant lesions [5]. But, for each lesion size category, the elasticity value was still significantly higher for malignant lesions than for benign lesions (P < 0.001). Likewise, our result showed that lesion diameter did not affect the discriminating ability of SWE in malignancy (Tables 3 and 4). Basically, the shear wave is detected by the ultrasonic echo signal. For extremely hypoechoic areas in a B-mode image, due to too low echo signal for successful detection, these areas where the propagation of shear wave may be limited are not colour coded on SWE as well [17]. Therefore, extrinsic factors such as the location of lesion or breast thickness can influence the elasticity value on SWE [5, 6]. In our study, however, the discriminating ability of SWE in malignancy was not influenced by these extrinsic factors (Tables 3 and 4). Meanwhile, Berg et al. reported that Eratio was significantly greater in palpable masses than in nonpalpable masses [6]. However, the differences in the percentage of malignancy between palpable (43.1 %) and nonpalpable masses (22.6 %) were also statistically significant and whether palpability was independently associated with Eratio or not was not proved. Our study showed that the performance of quantitative and qualitative SWE values in differentiating benign and malignant lesions was independent of lesion palpability (Tables 3 and 4).
Regarding the diagnostic performance of B-mode ultrasound, SWE, and combined B-mode ultrasound and SWE, previous studies [3, 5, 7] reported that the performance result was not significantly different between B-mode ultrasound and SWE, which was consistent with our result. When SWE features were considered in addition to standard BI-RADS features, the diagnostic performance was improved in our study, as reported previously [2, 4–7]. However, all but the study by Berg et al. [6] did not consider the subcategories of BI-RADS category 4. In the study by Berg et al. [6], they considered using SWE features to influence treatment of BI-RADS category 3 or 4a masses because the SWE feature would not change the treatment of clearly benign (BI-RADS category 2) or moderate-to-high suspicion (BI-RADS category 4c or 5) masses. Similarly, no category 3 lesions and all category 5 lesions were malignant in our study, and we considered using SWE features to influence the management of BI-RADS category 4a, 4b, and 4c lesions. For BI-RADS category 4a showing 8.9 % of the percentage of malignancy, adding Eratio with the cutoff value of 5.14 and a qualitative colour overlay pattern with the cutoff of pattern 3 would have further stratified BI-RADS category 4a lesions (P < 0.0001) (Table 5). When Eratio < 5.14 was used as a feature to indicate benignity, the percentage of malignancy decreased to 2.1 %. Likewise, when patterns 1 and 2 were used as features that would be benign, the percentage of malignancy for these lesions decreased to 2.4 %. For BI-RADS category 4b showing 28.6 % of the percentage of malignancy, adding Eratio with the cutoff value of 5.14 would have further stratified lesions with 0 % and 100 % of the percentage of malignancy for benign and malignant favouring lesions, respectively (P = 0.0009) (Table 5). However, it remains questionable whether these criteria can be used to downgrade category 4a or 4b lesions to follow-up. In adding SWE to category 4a lesions, four cancers would be missed by averting biopsy (Table 5). For category 4b lesions, the small number of case would limit the application of SWE criteria for a downgrade or upgrade of BI-RADS category. But the SWE information could offer reassurance on diagnosis or imaging-pathologic correlation after biopsy for category 4a or 4b lesions, and further investigation might be necessary.
There are some limitations to our study. Owing to its retrospective nature, there might have been selection bias because patients included in this study were scheduled for biopsy of known breast lesions, which may have had an effect on the BI-RADS final assessment for some performers at the time of ultrasound examination. Long-term follow-up data were not available in concordant benign lesions after CNB. The percentage of missed cancer in concordant benign CNB results was reported to be from 0 to 0.8 % (mean, 0.3 %) [18]. Considering the number of included cases and the performance of a combined B-mode ultrasound and SWE, however, it is expected that there is little change in the number of missed cancers. SWE was performed by one of four radiologists and the interobserver variability could be a limitation. Considering the prior results [4, 5, 19] showing that SWE was highly reproducible for assessing the elastographic features of breast lesions, interobserver variability was expected to have little influence on our result. In addition, the ultrasound images were reviewed by a single radiologist. Further evaluation might be necessary to validate the reproducibility of our results. For the combined diagnostic performance of B-mode ultrasound and SWE, the result was obtained not from the combined reading by a radiologist but from statistical analysis based on the results of B-mode ultrasound and SWE. Therefore, a specific guideline for the combination of BI-RADS category at B-mode ultrasound and SWE features was not provided.
In conclusion, the elasticity ratio (Eratio), the best-performing elasticity value, and the four-colour overlay pattern in SWE both showed good diagnostic performance in differentiating benign and malignant breast lesions; this finding was independent of patient age, mammographic breast density, lesion palpability, lesion diameter, lesion depth, distance from the nipple, breast thickness, and BI-RADS final assessment category. When adding Eratio or the four-colour overlay pattern to the BI-RADS category, the diagnostic performance was improved and SWE features may be helpful to stratify BI-RADS category 4a or 4b lesions.
References
Bercoff J, Tanter M, Fink M (2004) Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control 51:396–409
Athanasiou A, Tardivon A, Tanter M, Sigal-Zafrani B, Bercoff J, Deffieux T, Gennisson JL, Fink M, Neuenschwander S (2010) Breast lesions: quantitative elastography with supersonic shear imaging–preliminary results. Radiology 256:297–303
Evans A, Whelehan P, Thomson K, McLean D, Brauer K, Purdie C, Jordan L, Baker L, Thompson A (2010) Quantitative shear wave ultrasound elastography: initial experience in solid breast masses. Breast Cancer Res 12:R104
Tozaki M, Fukuma E (2011) Pattern classification of ShearWave Elastography images for differential diagnosis between benign and malignant solid breast masses. Acta Radiol 52:1069–1075
Chang JM, Moon WK, Cho N, Yi A, Koo HR, Han W, Noh DY, Moon HG, Kim SJ (2011) Clinical application of shear wave elastography (SWE) in the diagnosis of benign and malignant breast diseases. Breast Cancer Res Treat 129:89–97
Berg WA, Cosgrove DO, Dore CJ, Schafer FK, Svensson WE, Hooley RJ, Ohlinger R, Mendelson EB, Balu-Maestro C, Locatelli M, Tourasse C, Cavanaugh BC, Juhan V, Stavros AT, Tardivon A, Gay J, Henry JP, Cohen-Bacrie C, Investigators BE (2012) Shear-wave elastography improves the specificity of breast US: the BE1 multinational study of 939 masses. Radiology 262:435–449
Evans A, Whelehan P, Thomson K, Brauer K, Jordan L, Purdie C, McLean D, Baker L, Vinnicombe S, Thompson A (2012) Differentiating benign from malignant solid breast masses: value of shear wave elastography according to lesion stiffness combined with greyscale ultrasound according to BI-RADS classification. Br J Cancer 107:224–229
American College of Radiology (2003) Breast imaging reporting and data system (BI-RADS), 4th edn. American College of Radiology, Reston
Hong AS, Rosen EL, Soo MS, Baker JA (2005) BI-RADS for sonography: positive and negative predictive values of sonographic features. AJR Am J Roentgenol 184:1260–1265
Lazarus E, Mainiero MB, Schepps B, Koelliker SL, Livingston LS (2006) BI-RADS lexicon for US and mammography: interobserver variability and positive predictive value. Radiology 239:385–391
Kim EK, Ko KH, Oh KK, Kwak JY, You JK, Kim MJ, Park BW (2008) Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. AJR Am J Roentgenol 190:1209–1215
Raza S, Chikarmane SA, Neilsen SS, Zorn LM, Birdwell RL (2008) BI-RADS 3, 4, and 5 lesions: value of US in management—follow-up and outcome. Radiology 248:773–781
Chang JM, Moon WK, Cho N, Kim SJ (2011) Breast mass evaluation: factors influencing the quality of US elastography. Radiology 259:59–64
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Marcy PY, Thariat J, Lacout A (2012) Should we catch the train of shear-wave elastography? AJR Am J Roentgenol 198:W624–W625
Barr RG, Zhang Z (2012) Effects of precompression on elasticity imaging of the breast: development of a clinically useful semiquantitative method of precompression assessment. J Ultrasound Med 31:895–902
Barr RG (2012) Sonographic breast elastography: a primer. J Ultrasound Med 31:773–783
Youk JH, Jung I, Kim EK, Kim MJ, Son EJ, Moon HJ, Kwak JY (2012) US follow-up protocol in concordant benign result after US-guided 14-gauge core needle breast biopsy. Breast Cancer Res Treat 132:1089–1097
Cosgrove DO, Berg WA, Dore CJ, Skyba DM, Henry JP, Gay J, Cohen-Bacrie C (2012) Shear wave elastography for breast masses is highly reproducible. Eur Radiol 22:1023–1032
Acknowledgements
This research was supported by the Basic Science Research Programme through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011–0007602).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Youk, J.H., Gweon, H.M., Son, E.J. et al. Diagnostic value of commercially available shear-wave elastography for breast cancers: integration into BI-RADS classification with subcategories of category 4. Eur Radiol 23, 2695–2704 (2013). https://doi.org/10.1007/s00330-013-2873-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-2873-3