Abstract
Objectives
To evaluate the MR-based outcome predictors of lumbar transforaminal epidural steroid injection (ESI) for lumbar radiculopathy caused by herniated intervertebral disc (HIVD).
Methods
A total of 149 patients (male/female 75:74; mean age 51.5 years) with the very worst (87 patients) or the very best outcome (62 patients) after ESI were enrolled in this study. They were selected from 1,881 patients who underwent lumbar transforaminal ESI for lumbar radiculopathy caused by HIVD from January 2007 to December 2008. Two radiologists reviewed MR in consensus. Chi-square test and Fisher’s exact test were used to evaluate the difference between the two groups.
Results
HIVD in the foraminal–extraforaminal zone were significantly more common in the very best outcome group (16/24, 66.6 %) than HIVD in the central–subarticular zone (46/125, 36.8 %) (P = 0.012). Other factors such as HIVD zone, T2-high signal, relation to nerve root, corner change, Modic change, disc height loss, grade of disc degeneration, and osteophyte were not statistically significant.
Conclusion
HIVD in the foraminal or extraforaminal zone is the only good MR-based outcome predictor of lumbar transforamial ESI for lumbar radiculopathy.
Key Points
• Transforaminal epidural steroid injection is now widely used to relieve lumbar radiculopathy.
• Herniated disc material in the foraminal/extraforaminal region helps predict a good outcome.
• Other features of the disc were not significant predictors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal injection therapies have been widely used for many years [1–8]. Many papers have reported that beside other image-guided techniques, fluoroscopic guided lumbar transforaminal epidural steroid injection (ESI) is effective in relieving lumbar radiculopathy caused by herniated intervertebral disc (HIVD) [5, 9–12].
We have observed that ESI can be a good treatment option without pain recurrence for long periods in some patients; however, ESI failed to relieve the symptom in other patients. Many factors can influence the therapeutic effect of lumbar tranforaminal ESI on lumbar radiculopathy. Because they can include psychological, environmental, genetic and other factors, it is very difficult to gather all possible factors from the patients correctly and objectively. In addition, clinicians cannot obtain all possible outcome predictors from the patients in routine clinical practice. However, MR findings are relatively objective and are considered for most patients who are candidates for operation due to severe pain. Therefore, in this study, we focused on MR findings as possible outcome predictors for transforaminal ESI in managing lumbar radiculopathy.
We hypothesized that some MR findings of HIVD might be outcome predictors for lumbar transforaminal ESI to relieve radiculopathy. If MR-based outcome predictors are found, we can consider ESI or early operation according to the findings. If no MR-based outcome predictors are found, ESI can be considered for any patient irrespective of MR features before operation.
To our knowledge, few reports have analysed the MR features of HIVD influencing the effect of lumbar tranforaminal ESI [13, 14]. However, those studies analysed all patients who underwent injection. Guyer et al. [15] suggested that it was important to specify the definition of success/failure or of good/poor outcomes for investigating factors related to outcome in the study of outcome predictor analysis after lumbar spinal arthroplasty. They eliminated an intermediate group patients who they say fell into somewhat of a “grey zone”, i.e. those who might be classified as successes or failures with slight changes in the definition of success, and analysed the data from patients who had the very best outcomes and those with the very worst outcomes. The purpose of this study was to evaluate the MR-based outcome predictors of lumbar transforaminal ESI for lumbar radiculopathy caused by HIVD in the patients who had the very best outcome and those with the very worst outcome.
Methods
Patient selection
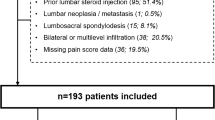
This study was approved by the institutional review board. Informed consent was waived. One radiologist screened 1,881 patients who underwent lumbar transforaminal ESI in our department from January 2007 to December 2008. The same one radiologist retrospectively reviewed the patients’ medical records and selected extreme response groups. MR review and telephone interview were additionally conducted for patients if there were unclear descriptions in their medical records. Exclusion criteria were (1) previous operation, (2) previous injection, (3) no follow-up after injection, (4) absence of lumbar spine MR, (5) lumbar radiculopathy caused by spinal stenosis. Inclusion criteria were (1) lumbar radiculopathy caused by HIVD, (2) either very best outcome or very worst outcome after lumbar transforaminal ESI, (3) availability of lumbar spine MR data obtained less than 2 months before or after lumbar transforaminal ESI. Response after ESI was measured by visual analogue scale (VAS) and five-point self-satisfaction scale (no pain, much improved, slightly improved, no change, aggravated). Very best outcome was defined by (1) initial response with much improvement or no pain and a reduction in the VAS score of more than 50 % on chart documentation 2 weeks after a series of ESI, and (2) more than 2 years’ symptom improvement after ESI without operation based on chart documentation and telephone interview. Very worst outcome was defined by (1) no improvement or aggravated state or a reduction in the VAS of less than 50 % on chart documentation after a series of ESI, or (2) temporary improvement after a series of ESI but symptom recurrence in less than 2 months, or (3) temporary improvement after series of ESI but symptom recurrence resulting in operation in less than 6 months. On the basis of the exclusion criteria, 917 patients were excluded. Among remaining 964 patients, 815 patients showed intermediate outcome. Finally, 149 patients (male/female 75:74; mean age 51.5 years; range 18–87 years) were enrolled in this study. Among them, the very worst outcome group comprised 87 patients, and the very best outcome group comprised 62 patients.
Injection technique and interval
Transforaminal ESI was performed using fluoroscopic guidance by one of three experienced musculoskeletal radiologists who had experience with more than 1,000 ESI procedures. The uniplanar (Intergris Allura Xper FD 20; Philips Medical Systems, Best, Netherlands) digital subtraction angiography unit was used for fluoroscopy. With patients in the prone position and under sterile preparation, a 22G spinal needle was advanced into the neural foramen with intermittent injection of the contrast agent (Omnipaque 300 [iohexol, 300 mg iodine per mL]; Amersham Health, Princeton, USA) until the contrast agent spread smoothly around the nerve root (Figs. 1 and 2). Then, a mixture of 40 mg (1 mL) triamcinolone acetonide suspension (Tamceton [40 mg/mL]; Hanall Pharmaceutical, Seoul, Korea) and 0.5 mL normal saline and a mixture of 1 mL bupivacaine hydrochloride (0.5 mL/0.5 %; Marcaine Spinal 0.5 % Heavy; AstraZeneca, Westborough, USA) and 0.5 mL normal saline were injected into the epidural space. A series of repeat ESI was considered after 2 weeks with one further repeat 2 weeks later (three treatments in total).
A 54-year-old woman with the very best outcome. On MR images (a–c), herniated intervertebral disc (HIVD) was noted at L5/S1 right foraminal zone with right L5 nerve root compression. After transforaminal epidural steroid injection (ESI) via L5/S1 right neural foramen (d), the patient expressed no pain in the leg, and did not show leg pain during 2 years of subsequent follow-up. There was no relapse on the last follow-up
A 35-year-old man with the very worst outcome. On MR images (a–c), HIVD was noted at L5/S1 right central zone with right S1 nerve root compression. Even after two transforaminal ESIs via right S1 neural foramen (d) and right L5/S1 neural foramen (e) with 2 weeks’ interval, the patient showed no improvement, and underwent subsequent surgery
MR analysis
One of the radiologists who screened patients recorded the symptomatic disc level and level of transforaminal injection in a separate database without any comment about clinical outcome. The other two radiologists, who were blinded to clinical outcome and were informed of the causing HIVD level and level of transforaminal injection, only reviewed MR images in consensus. The two radiologists reviewed MR for the following items: HIVD type, HIVD zone, HIVD volume, T2-high signal in the HIVD, relation of HIVD to nerve root, corner change, Modic change, disc height loss, grade of disc degeneration, and posterior osteophyte. HIVD type was classified as protrusion or exclusion; HIVD zone was classified as central, subarticular, foraminal or extraforaminal; and HIVD volume was classified as mild, moderate or severe—all according to American Society of Spine Radiology (ASSR)–American Society of Neuroradiology (ASNR)–North American Spine Society (NASS) recommendations [16]. Canal compromise of less than one third of the canal at the most severely compromised axial section is defined as “mild”, between one and two thirds as “moderate” and over two thirds as “severe”. The same grading can be applied for foraminal involvement [16]. Presence of high signal change in the herniated disc was also evaluated on T2-weighted images. The relation between HIVD and nerve root was classified as contact, displacement or compression [17]. Corner changes were classified as none, or as either or both erosion or Modic change in the posterior corner of the vertebral body. Subchondral bone marrow signal change was classified as type 1, 2 or 3 according to Modic’s suggestion (whence the term “Modic change”) [18]. Disc height loss was classified as none, less than half or more than half, compared with relatively intact intervertebral disc level. Disc degeneration was graded according to Pfirrmann’s suggestion [19]. Presence of posterior osteophyte with HIVD was evaluated.
Clinical variables
Age, sex, symptom duration and pattern of symptom attack (initial versus recurrent) were evaluated by one radiologist on the basis of the chart documentation. For statistical analysis, we also classified patients’ ages into six age groups: less than 29 years old, 30–39, 40–49, 50–59, 60–69 and greater than 70 [5]. Symptom duration before injection was classified as less than 2 weeks, 2 weeks to 1 month, 1–3 months, 3–6 months and more than 6 months.
Statistical analysis
Chi-square tests were used to evaluate the relation between the very best or the very worst outcome group and HIVD level (L1/2 to L5/S1), HIVD zone, HIVD volume, relation of HIVD to nerve root, corner change, Modic change, disc height loss, grade of disc degeneration, age groups and symptom duration. For the relation between HIVD volume with the very best or the very worst outcome group, statistical analysis was assessed separately for HIVD in the central–subarticular zone and for HIVD in the foraminal–extraforaminal zone because of different definitions of HIVD volume according to different HIVD zone. Age difference between the very best outcome group and the very worst outcome group was evaluated by Mann–Whitney U test. Fisher’s exact test was used to evaluate the relation between the very best or the very worst outcome group and HIVD type (protrusion versus extrusion), presence of T2-high signal in HIVD, presence of posterior osteophyte, gender and pattern of symptom attack (initial versus recurrent).
HIVD zone, corner change, Modic change, grade of disc degeneration, age group and symptom duration were further classified into two categories for dichotomous analyses, and Fisher’s exact tests were used to evaluate the relation between those factors and the very best or the very worst outcome group. HIVD zone was classified as central–subarticular versus foraminal–extraforaminal zone. Corner change was divided into two categories: absence versus presence. Modic change was also divided into two categories: absence versus presence. Grade of disc degeneration was divided into two categories: grades 1, 2 and 3 versus grades 4 and 5. Age groups were separated into two groups after initial statistical analysis of all six groups. Symptom duration was divided into two categories: less than 1 month versus more than 1 month.
PASW statistics 17.0 (SPSS, Chicago, Ill) was used for statistical calculation. A p value of less than 0.05 was considered to indicate a significant difference.
Results
Results are summarised in Tables 1 and 2. HIVD zone with dichotomous analysis (central–subarticular versus foraminal–extraforaminal zone) was statistically significant between the two groups (P = 0.012). HIVD in the foraminal–extraforaminal zone was more common in the very best outcome group than in the very worst outcome group (Fig. 1). HIVD in the central–subarticular zone was more common in the very worst outcome than in the very best outcome group (Fig. 2). Of the 24 patients with HIVD in the foraminal–extraforaminal zone, 16 (66.7 %) were in the very best outcome group and eight (33.3 %) were in the very worst outcome. In 125 patients with HIVD in the central–subarticular zone, only 46 patients (36.8 %) belonged to the very best outcome group and 79 patients (63.2 %) belonged to the very worst outcome group. In 35 patients with HIVD in the subarticular zone only, 21 patients (60.0 %) were in the very worst outcome group and 14 patients (40.0 %) were in the very best outcome group.
HIVD levels were common in L4/5 and L5/S1, which was not significantly different between the two groups. HIVD volume, T2-high signal in the HIVD, relation of HIVD to the nerve roots, corner change, Modic change, disc height loss, grade of disc degeneration and presence of posterior osteophyte were also not significantly different between the groups.
Age groups were significantly different between the outcome groups (P = 0.007). In the age group of 60–69 years, patients in the very best outcome group were more common than those in the very worst outcome group (20 patients versus eight patients). For dichotomous analysis of age groups, we separated those groups into two: greater than or equal to 60 years old versus less than 60 years old. Of the 52 patients greater than or equal to 60 years old, 27 patients (51.9 %) were in the very best outcome group, and 25 patients (48.1 %) were in the very worst outcome group. However, of the 97 patients less than 60 years old, only 35 patients (36.1 %) were in the very best outcome group, and 62 patients (63.9 %) were in the very worst outcome group (P = 0.045). Gender, symptom duration and pattern of symptom attack were not significantly different between the two groups.
Discussion
Our results suggest that HIVD in either or both the foraminal and extraforaminal zone was more common in the very best outcome group than HIVD in either or both the central and subarticular zone after lumbar transforaminal ESI. Other MR findings could not be regarded as outcome predictors after lumbar transforaminal ESI.
The precise definition of good and poor outcome is very important; there is a large intermediate group of patients who can be classified as either good or poor outcome with slight changes in the definition of success. In particular, determination of the outcome after ESI mainly depends on patients’ subjective expressions concerning pain relief. Therefore, in our study, we tried to select response groups from extreme ends of the spectrum—the very best and the very worst outcome groups—after eliminating the intermediate group.
In cases with HIVD in either or both the foraminal and extraforaminal zone, transforaminal ESI could inject the drugs into the compressed lesion more completely, which may be one of the causes of the excellent response. This result may suggest that in patients with HIVD in the foraminal or extraforaminal zone, more active nonoperative methods such as transforaminal ESI should be considered before operation. This result is similar to that of Choi et al.’s study [13] and Komori et al.’s case report [20].
In our study, the number of patients with HIVD in the foraminal and extraforaminal zone is much less than those with HIVD in the central and subarticular zone. The disproportionate number of patients with different HIVD zones is probably caused by the rarity of the HIVD in the foraminal and extraforaminal zone. Previous studies revealed that the proportion of HIVD in the foraminal and extraforaminal zone was 2.6–11.7 % of all lumbar HIVD [21–23].
According to our study, the volume of HIVD was not a factor related to the effect of ESI. If a large volume of disc is herniated into the epidural space, a more aggressive healing mechanism may be induced. In addition, severe disc herniations may have a greater chance of resolution of HIVD. Komori et al. [20] reported that disappearance of HIVD was seen frequently in cases of migrating disc herniation, and it was presumed that exposure to the vascular supply had a strong association with this phenomenon. Bush et al. [24] reported that a high proportion of patients with discogenic sciatica made a satisfactory recovery with aggressive conservative management, accompanied by resolution of HIVD. Therefore, if there is no motor weakness or neurologic deficit, a large volume of HIVD may not be an obstacle to conservative management, including ESI.
Contrary to previous studies [13, 14], the relation of nerve root to HIVD was not a significant risk factor in our study. Radiculopathy was known to be induced by inflammatory reaction rather than by mechanical compression only [25–27]; therefore, morphology of nerve root demonstrated on MR may not be a risk factor influencing effects after conservative management.
Interestingly, patients in the very best outcome group were older than those in the very worst outcome group. Because this study excluded patients having spinal stenosis, the patients in the older group often had HIVD as the sole cause of radiculopathy. Therefore, longstanding compression or structural change, which is usually present in the older age group, may not affect the result. The cause of that result may be due to the different contents of herniated disc depending on the patients’ age. In young patients, HIVD tends to have more components of nucleus pulposus, which is known to be a causative component of inflammatory reaction resulting in radiculopathy [25]. In older patients, HIVD tends to have more components of fragmented annulus fibrosus. Golish et al. [28] recently reported that an epidural lavage assay of structural matrix proteins and their degradation fragments, including fibronectin and aggrecan, associated with degenerative disc disease can predict good response to lumbar ESI for radiculopathy with HIVD. The main role of ESI is to reduce pain in a prompt manner and thereby improve quality of life. Because we measured the initial response 2 weeks after ESI, this study mainly assessed outcome predictors for ESI. However, other factors influence the possibility of recurrence over the next 2 years (e.g. normal healing potential) and several studies have suggested that the effect of ESI may only be temporary [29, 30].
Our study has some limitations. Firstly, it is a retrospective study. However, to select extreme results group, it is necessary to gather a large number of patients with longer follow-up periods. Therefore, prospective research is somewhat difficult for this kind of study. But, to gather further patient information (clinical outcome variables, follow-up responses, etc.) more rigorous prospective studies about outcome predictors after injection would be required. We hope our study promotes further prospective study about MR outcome variables after ESI. Second, we did not take into account potential confounders for causes of pain, such as environmental and psychological risk factors.
In conclusion, herniated disc material in the foraminal or extraforaminal region is the only good MR-based outcome predictor of lumbar transforamial epidural steroid injection for lumbar radiculopathy.
References
Manchikanti L, Boswell MV, Singh V et al (2009) Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician 12:699–802
Lee JW, Shin HI, Park SY, Lee GY, Kang HS (2010) Therapeutic trial of fluoroscopic interlaminar epidural steroid injection for axial low back pain: effectiveness and outcome predictors. AJNR Am J Neuroradiol 31:1817–1823
Lee JH, An JH, Lee SH (2009) Comparison of the effectiveness of interlaminar and bilateral transforaminal epidural steroid injections in treatment of patients with lumbosacral disc herniation and spinal stenosis. Clin J Pain 25:206–210
Kwon JW, Lee JW, Kim SH et al (2007) Cervical interlaminar epidural steroid injection for neck pain and cervical radiculopathy: effect and prognostic factors. Skeletal Radiol 36:431–436
Jeong HS, Lee JW, Kim SH, Myung JS, Kim JH, Kang HS (2007) Effectiveness of transforaminal epidural steroid injection by using a preganglionic approach: a prospective randomized controlled study. Radiology 245:584–590
Cooper G, Lutz GE, Boachie-Adjei O, Lin J (2004) Effectiveness of transforaminal epidural steroid injections in patients with degenerative lumbar scoliotic stenosis and radiculopathy. Pain Physician 7:311–317
Lee JW, Kim SH, Lee IS et al (2006) Therapeutic effect and outcome predictors of sciatica treated using transforaminal epidural steroid injection. AJR Am J Roentgenol 187:1427–1431
Lee JW, Myung JS, Park KW et al (2010) Fluoroscopically guided caudal epidural steroid injection for management of degenerative lumbar spinal stenosis: short-term and long-term results. Skeletal Radiol 39:691–699
Vad VB, Bhat AL, Lutz GE, Cammisa F (2002) Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976) 27:11–16
Ackerman WE 3rd, Ahmad M (2007) The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg 104:1217–1222
Schaufele MK, Hatch L, Jones W (2006) Interlaminar versus transforaminal epidural injections for the treatment of symptomatic lumbar intervertebral disc herniations. Pain Physician 9:361–366
Lee IS, Kim SH, Lee JW et al (2007) Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol 28:204–208
Choi SJ, Song JS, Kim C et al (2007) The use of magnetic resonance imaging to predict the clinical outcome of non-surgical treatment for lumbar intervertebral disc herniation. Korean J Radiol 8:156–163
Ghahreman A, Bogduk N (2011) Predictors of a favorable response to transforaminal injection of steroids in patients with lumbar radicular pain due to disc herniation. Pain Med 12:871–879
Guyer RD, Siddiqui S, Zigler JE et al (2008) Lumbar spinal arthroplasty: analysis of one center’s twenty best and twenty worst clinical outcomes. Spine (Phila Pa 1976) 33:2566–2569
Fardon DF, Milette PC (2001) Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 26:E93–E113
Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N (2004) MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology 230:583–588
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193–199
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Komori H, Shinomiya K, Nakai O, Yamaura I, Takeda S, Furuya K (1996) The natural history of herniated nucleus pulposus with radiculopathy. Spine (Phila Pa 1976) 21:225–229
Dickman CA, Mamourian A, Drayer BP, Sonntag VK, Spetzler RF (1990) MR imaging of lateral disc herniation. J Neurosurg 73:642–643
O'Hara LJ, Marshall RW (1997) Far lateral lumbar disc herniation. The key to the intertransverse approach. J Bone Joint Surg Br 79:943–947
Liu T, Zhou Y, Wang J et al (2012) Clinical efficacy of three different minimally invasive procedures for far lateral lumbar disc herniation. Chin Med J (Engl) 125:1082–1088
Bush K, Cowan N, Katz DE, Gishen P (1992) The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine (Phila Pa 1976) 17:1205–1212
McCarron RF, Wimpee MW, Hudkins PG, Laros GS (1987) The inflammatory effect of nucleus pulposus. A possible element in the pathogenesis of low-back pain. Spine (Phila Pa 1976) 12:760–764
Kang JD, Georgescu HI, McIntyre-Larkin L, Stefanovic-Racic M, Donaldson WF 3rd, Evans CH (1996) Herniated lumbar intervertebral discs spontaneously produce matrix metalloproteinases, nitric oxide, interleukin-6, and prostaglandin E2. Spine (Phila Pa 1976) 21:271–277
Matsui Y, Maeda M, Nakagami W, Iwata H (1998) The involvement of matrix metalloproteinases and inflammation in lumbar disc herniation. Spine (Phila Pa 1976) 23:863–868, discussion 868–869
Golish SR, Hanna LS, Bowser RP, Montesano PX, Carragee EJ, Scuderi GJ (2011) Outcome of lumbar epidural steroid injection is predicted by assay of a complex of fibronectin and aggrecan from epidural lavage. Spine (Phila Pa 1976) 36:1464–1469
Price C, Arden N, Coglan L, Rogers P (2005) Cost-effectiveness and safety of epidural steroids in the management of sciatica. Health Technol Assess 9:1–58
Karppinen J, Malmivaara A, Kurunlahti M et al (2001) Periradicular infiltration for sciatica: a randomized controlled trial. Spine (Phila Pa 1976) 26:1059–1067
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J.W., Choi, S.W., Park, S.H. et al. MR-based outcome predictors of lumbar transforaminal epidural steroid injection for lumbar radiculopathy caused by herniated intervertebral disc. Eur Radiol 23, 205–211 (2013). https://doi.org/10.1007/s00330-012-2566-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2566-3