Abstract
Objective
To compare dose and image quality of 64-slice, first and second generation dual-energy CT (DECT) for CT pulmonary angiography (CTPA).
Methods
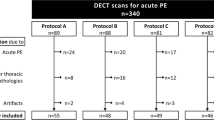
Totally 120 patients, 30 in each group, underwent CTPA on a first generation (group 1: single-energy, 120 kV/145 mAs; group 2: DE, 140/80 kV, 70/350 mAs) or second generation dual-source DECT device (group 3: DE, 100/Sn140 kV, 120/102 mAs; group 4: DE, 80/Sn140 kV, 202/86 mAs). CTDIvol, DLP, background noise (BN), thorax diameter and attenuation in the pulmonary trunk were compared.
Results
Thorax diameter and attenuation in the pulmonary trunk did not differ significantly (p > 0.4 and >0.19) between the groups. Mean CTDIvol and DLP were significantly lower (p < 0.003) in group 4 (6.2 ± 1.6 mGy/170 ± 41 mGycm) compared to group 1 (8.5 ± 2.6 mGy/235 ± 117 mGycm), group 2 (9.2 ± 3.3 mGy/224 ± 122 mGycm) and group 3 (8.7 ± 2.8 mGy/246 ± 86 mGycm). BN was significantly lower (p < 0.0001) in group 4 (12 ± 3 HU) and group 1 (13 ± 6 HU) compared to group 3 and 2 (16 ± 6 HU and 23 ± 9).
Conclusion
The use of second generation DECT in 80/Sn140 kV configuration allows for significant dose reduction with image quality similar to 120 kV CTPA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary embolism (PE) represents a frequent and relevant condition in daily clinical routine associated with high mortality [1, 2]. Morbidity and mortality resulting from PE can be reduced significantly by early initiation of appropriate treatment [3–5]. Therefore, accurate and timely diagnosis is imperative and heavily relies on thin-section multi-detector row computed tomography (MDCT) pulmonary CT angiography (CTPA) rather than invasive pulmonary angiography and ventilation/perfusion scintigraphy [6–8]. With the introduction of dual-source CT systems and their capability of dual-energy imaging evaluation of PE has entered a new age: This new CT generation combines thin-section collimation with the opportunity of spectral imaging [9]. Beyond emboli visualization, dual-energy CTPA contributes functional aspects: Making use of the unique x-ray absorption characteristics of iodinated contrast material at high and low photon energies (given by tube potential settings) [10, 11], DECT allows to create iodine distribution maps of the lung parenchyma and to display perfusion defects caused by obstructive PE or other lung abnormalities [12–20].
However, there is only little data available regarding dose and image quality at CTPA with this new technique. Although CT examinations account only for a minority of radiological procedures, they are jointly accountable for the predominant percentage of iatrogenic diagnostic radiation exposure of the population [21–23]. In recent years, many approaches to reduce patient dose at CTPA have been investigated including routine use of automatic exposure control software, reduction of tube current and tube potential. Since the introduction of DECT with the dual-source approach there have been concerns about exposing the patient to excessive dose as the same volume is simultaneously irradiated by two x-ray tubes. First data from a phantom study could rebut this concern [24]. However, transferring results from a phantom to patients is generally difficult, as dose and image quality is largely dependent on patient parameters that cannot be simulated by a static phantom. The present study reflects our experience with dual-energy CTPA in clinical routine with two generations of dual-source dual-energy CT in unselected consecutive patients who were referred to our department to rule out pulmonary embolism. The purpose of this study was to investigate dose levels and image quality parameters for both generations of dual-source dual-energy CT and compare them to a standard single-source single-energy CTPA protocol of a 64-slice device.
Methods and materials
Patient population
The data analysed retrospectively in this study was acquired in a time frame of 34 months (August 2007 until June 2010). During that time, our installed CT devices as well as CT protocols underwent some changes. Until December 2009, every patient referred to CTPA for suspected PE was examined on a dual-source CT device of the first generation (Somatom Definition, Siemens Healthcare, Forchheim, Germany). Between August and December 2007, patients were examined with the single-source protocol introduced below (group 1). Between January 2008 and December 2009, patients were examined in dual-energy mode (140 kV/80 kV). Patients of group 2, however, were selected from the time span between July 2009 and December 2009, when we had implemented our dedicated dual-energy contrast injection protocol introduced below. In mid December 2009, the CT machine was replaced by a dual-source CT device of the second generation (Somatom Definition Flash, Siemens Healthcare). From December 2009 to March 2010 patients underwent dual-energy CTPA with a 100 kV/140 kV + tin filter protocol (group 3). From there on patients (group 4) were examined with an 80 kV/140 kV + tin filter protocol. From every group, 30 randomly selected patients were included for this analysis. There were no exclusion criteria. The ethics committee of our hospital did not see any ethical problems and waived the need for informed patient consent.
CT protocols
Details on CT protocols are given in Table 1. While in the first generation of DECT, collimation for CTPA was restricted to 1.2 mm for optimized cross-scattered radiation correction, the second CT generation features improved software-base cross-scattered radiation correction and therefore allows to use a 0.6 mm collimation also in dual-energy mode. Further, the spectrum of the 140 kV tube is additionally hardened by a tin filter (Sn) for better separation of the mean spectra emitted by the low and high kV tube and for better tissue penetration. CT protocol settings followed the manufacturer’s recommendations.
Due to the restricted detector collimation of 14 × 1.2 mm in group 2, images were reconstructed at a slice thickness of 1.5 mm with a position increment of 1.0 mm with a medium-soft convolution kernel (B30f). In group 1, 3 and 4, images were reconstructed at 1.0 mm slice thickness with 0.5 mm increment using the same kernel (B30f). By default, three images series are reconstructed for dual-energy examinations: One series each for the high and low kV, and one mixed series merging information of both the high and low kV data set to create an image impression of a virtual 120 kV examination. For that purpose, 70% of the 140 kV and 30% of the 80 kV data were blended (so called M_03 series) in group 2. In group 3, 60% of the 100 kV data and 40% of the hardened 140 kV spectrum data were blended (M_0.6 series). In group 4, a mixing ratio of 40% of the 80 kV data and 60% of the hardened 140 kV spectrum was used (M_0.4 series). Blending ratios followed the manufacturer’s recommendations.
CT examinations were contrast-enhanced using iodinated contrast material (CM) with 400 mgI/ml (Imeron 400, Bracco, Konstanz, Germany), injected into an antecubital vein with a flow of 4 ml/s. In group 1, 75 ml of CM was followed by a 40 ml NaCl chaser bolus. As DECT iodine mapping is very sensitive for dense contrast material in the subclavian vein and superior vena cava, the use of a compact CM bolus with a good wash out of the venous system is essential to avoid artifacts. Therefore, we used a 50 ml bolus of pure CM, followed by 30 ml of a mixed phase with 30% of CM and 70% of NaCl, followed by a 50 ml chaser bolus of pure NaCl in groups 2–4. This protocol has shown satisfying results with vascular enhancement and low artefact burden on lung perfusion analysis in our daily routine use. In all patients, bolus tracking was used for automated start of the examination with a start trigger of 140 HU within the pulmonary trunk and a start delay of 7 s. Images were acquired in caudocranial direction between the apices and costophrenic recesses with the lungs held in normal expiration (“Breathe in, breathe out, don’t breathe”).
Dose estimates and image quality analysis
For the estimation of radiation doses, we recorded the volume CT dose index (CTDIvol in mGy), and dose length product (DLP in mGycm) from the patient protocol, which is automatically generated after the end of an examination and stored in the PACS of our department.
The biggest thoracic diameter from skin surface to skin surface was measured in axial slices in each patient to compare the groups in terms of body habitus. As measures of image quality several region-of-interest (ROI) measurements were performed on a RIS/PACS workstation (Centricity 4.1, General Electric Healthcare, Dornstadt, Germany) using a circle tool. Mean attenuation values and standard deviation were recorded and displayed in Hounsfield Units (HU). Background noise (BN) was determined as the standard deviation of air measured presternally in front of the patient. The attenuation in the pulmonary trunk (APT), the apical segmental artery (AS1) and posterior basal segmental artery (AS10) was measured. ROI were drawn as large as possible to include as much of the contrast filled lumen of the pulmonary arteries. On segmental level, ROI were placed as distally as possible but in a vessel part with a diameter of at least 4 mm. If an embolus was present in the respective segmental pulmonary artery, the contralateral vessel was measured. All measurements were performed by a radiologist with 6 month of experience in chest CT. Based on these measurements, signal-to-noise ratio (SNR) was determined according to the following equation:
A frequency distribution analysis was performed for density values in the pulmonary arteries in both groups using a cut-off value of 200 HU, a value that has been previously described as attenuation margin for diagnostic CT angiography [25–27]. Image quality was further rated subjectively and independently by two blinded radiologists with more than 5 years of experience in chest CT according to a five-point scale (1 = excellent to the very peripheral branches, 2 = good, exclusion of PE to the subsegmental level surely possible, 3 = moderate, exclusion of PE sure to segmental level, uncertainties beyond, 4 = still diagnostic to lobar level but with significantly reduced confidence beyond, 5 = non-diagnostic, needed to be repeated). In groups 2–4, all measurements and ratings were performed on the mixed, virtual 120 kV series (i.e. M_03, M_0.6, M_0.4).
Statistical analysis
Analyses were performed computer-based with dedicated software (BiAS 9.02, Epsilon Verlag, Frankfurt, Germany). Patient age, thorax diameters, attenuation values, SNR, subjective image quality score, DLP and CTDIvol, are expressed as mean values ± standard deviations. We tested continuous variables for normal distribution using the Kolmogoroff-Smirnoff-Lilliefors test, corrected according to Dallal-Wilkinson as appropriate. Since data was distributed non-normally, we applied the U test according to Wilcoxon-Mann-Whitney. We considered a p-value of less than 5% to be statistically significant and used two-sided tests. We applied Fisher’s exact test to compare the incidence of PE and the frequency distribution of patients with respect to gender and an attenuation margin of 200 HU in their pulmonary arteries. Inter-observer agreement of subjective image quality ratings was assessed with Cohan’s weighted kappa analysis.
Results
Patient characteristics
Patient characteristics are summarized in Table 2. Patients in group 2 were significantly (p < 0.033) younger (50.7 ± 19.0 years) compared to patients in group 3 and 4. Beyond that, no significant differences were found regarding gender distribution or incidence of pulmonary embolism (7/30 vs. 8/30 vs. 7/30 vs. 9/30 cases for group 1 vs. 2 vs. 3 vs. 4). Mean thorax diameter did also not differ significantly between the groups. Therefore, further analysis and comparison of radiation exposure and image quality was considered feasible and valid.
Radiation dose
Mean CTDIvol and DLP were significantly lower (p < 0.013) in group 4 (6.2 ± 1.6 mGy/170 ± 41 mGycm) compared to group 1 (8.5 ± 2.6 mGy/235 ± 117 mGycm), group 2 (9.2 ± 3.3 mGy/224 ± 122 mGycm) and group 3 (8.7 ± 2.8 mGy/246 ± 86 mGycm). Differences between groups 1–3 were insignificant. Similar results were observed when looking at CTDIvol separately for male and female patients in the four different groups. While DLP of male patients showed the same distribution, the mean DLP of female patients of group 2 (186 ± 71 mGycm) was the second lowest after group 4 (175 ± 43 mGycm) and therefore significantly lower than in group 3 (252 ± 102 mGycm). As a consequence, the difference between group 2 and 4 did not reach statistical significance. Data is summarized in Table 3.
Image quality
BN was significantly lower (p < 0.0001) in group 4 (12 ± 3 HU) and group 1 (13 ± 6 HU) compared to group 3 and 2 (16 ± 6 HU and 23 ± 9). Differences between group 1 and 4 were insignificant. The attenuation within the pulmonary trunk was a little higher in group 4 (341 ± 102 HU), compared to group 2 (324 ± 104 HU), group 1 (317 ± 96 HU) and group 3 (302 ± 116 HU), but without statistical significance between the groups. Regarding segmental arteries, significantly higher attenuation was found for segment 1 artery (389 ± 120 HU) in group 1 compared to all other groups. Corresponding SNR for the pulmonary trunk and the segmental arteries S1 and S10 were significantly higher for group 1 and 4 compared to group 2 and 3 (Fig. 1). Data is summarized in Table 4.
Comparison of image quality. a–d give an example for image impression achieved with 120 kV 64-slice CT (a), first generation dual-energy CT (b) and second generation dual-energy CT with 100 kV/Sn140 kV configuration (c) and 80 kV/Sn140 kV configuration (d). Section thickness is 1.0 mm for image a, c and d and 1.5 mm for image b. Image noise was measured with a region-of-interest tool presternally as standard deviation of air. Typical noise values are noted with 8.8 HU (a) and 8.9 HU (d) for 120 kV 64-slice and second generation DECT with 80/Sn140 kV. Image noise was slightly higher with the 100/Sn140 kV configuration (e.g. 15.8 HU in image c) and clearly higher for first generation DECT (in this case 28.3 HU in image b). The corresponding signal-to-noise-ratio was 41.8 (a), 18.9 (b), 20.1 (c) and 58.8 (d), respectively
Comparing group 1, 2, 3 and 4, a vascular attenuation of >200 HU was achieved for the pulmonary trunk in 28 (93.3%), 26 (86.7%), 25 (83.3%) and 30 (100%) patients, for the S1 artery in 28 (93.3%), 27 (90%), 25 (83.3%) and 26 (86.7%) patients, and for the S10 artery in 30 (100%), 25 (83.3%), 28 (93.3%) and 28 (93.3%) patients, respectively. Differences between the groups were insignificant (p for all >0.05).
Mean subjective image quality was rated best for group 4 by both observers (1.53 ± 0.63 and 1.77 ± 0.68; κ = 0.74 with p = 0.0015) followed by group 1 (1.70 ± 0.75 and 1.80 ± 0.81; κ = 0.80 with p = 0.0078) with no significant difference between both groups. Subjective image quality was rated lower in group 2 (2.00 ± 0.74 and 2.13 ± 0.78; κ = 0.82 with p = 0.0001) and group 3 (1.96 ± 1.00 and 2.00 ± 1.05; κ = 0.95 with p < 0.0001) by both observers compared to group 1 and 4. However, only between group 2 and 4, there was a significant difference in image quality score with observer 1 in favour for group 4. No examination needed to be repeated due to unsatisfying image quality (i.e. “5”). Data is summarized in Table 4.
Discussion
In a first phantom study, Schenzle et al. [24] were able to show that with the same dual-source CT systems as in the underlying study there is no increase in dose with constant noise levels in comparison to a 120 kV standard protocol. However, transferring results from a phantom trial to clinical routine use in patients is generally difficult, as dose and image quality is largely dependent on patient parameters that cannot be simulated by a static phantom. Further, the 80 kV/Sn140 kV configuration of the second generation DECT was not investigated in that study. In terms of dose exposure, our clinical results support Schenzle’s findings for the 140 kV/80 kV and 100 kV/Sn140 kV configuration in comparison to our standard clinical 120 kV single-energy protocol. When looking at separate gender-based analysis of our data, we even found lower DLP in female patients of group 2 examined on first generation DECT. On the other hand, CTDIvol did not show any statistically significant differences compared to group 1 and 3, hence this finding is most likely based on shorter z-axis coverage in female patients of group 2. When it comes to image quality parameters, contrary to Schenzle’s observations, the 140 kV/80 kV configuration of the first generation DECT showed almost double the noise values than the 120 kV single-energy protocol although images were reconstructed at 1.5 mm compared to 1.0 mm and a 14 × 1.2 mm collimation was used for optimized cross-scatter correction. Taking this into account, image noise could be expected to be even higher, if a 0.6 mm collimation with 1.0 mm reconstructed images had been used. To what degree that would have affected subjective image quality, however, cannot be appreciated with the data of this work.
As a relevant finding we were able to show that with the 80 kV/Sn140 kV configuration of the second generation DECT a noise level equal to that of 120 kV single-energy CT examinations with a significant reduction of patient dose is achievable in clinical routine. Although a “soft” 80 kV spectrum on tube A was used in group 4, no adverse effects on image quality were observed, but a relevant impact on dose parameters was achieved. A possible explanation for this finding may be that the 140 kV spectrum, which is additionally hardened by a tin filter, contributes data for high spatial resolution with little noise, while the 80 kV spectrum contributes excellent iodine contrast. Hence, to create a virtual 120 kV image impression, only 40% of the 80 kV data needs to be blended with 60% of the Sn140 kV data. This allows to keep the influence of higher image noise with the softer spectrum low on the one hand, but to benefit from the inherent lower dose profile of the 80 kV spectrum on the other hand. A tube potential of 100 kV will show a more disadvantageous dose profile with lower iodine contrast. To achieve a similar contrast impression with the 100 kV/Sn140 kV configuration, 60% of the 100 kV data needs to be blended with 40% of the Sn140 kV data, hence resulting in a slightly but significantly increased image noise in group 3 with dose parameters equal to group 1 and 2, but significantly higher than in group 4 (i.e. 80 kV/Sn140 kV). Beyond this, tube current settings for the Sn140 kV tube were lower in group 4 than in group 3 due to technical requirements given by the manufacturer, which represents another factor for lower dose parameters in group 4.
Especially in front of the increasing debate about radiation dose in CT this is an important observation as dual-energy CT sees itself in a tough competition from so called low-dose CT protocols for CTPA with single-energy devices. These low-dose protocols mostly base on the fact that it has been understood that lowering the tube potential from 140 kV or 120 kV to 100 kV or 80 kV with constant or slightly adjusted tube current time product will result in a 40–50% decrease of patient dose [28–32]. The second benefit is that lowering the tube potential will move the mean energy of the produced x-ray spectrum more towards the k-edge of iodine and thus increase CT numbers and therefore vascular opacification [11]. Lowering tube potential with constant tube current settings will result in increased image noise. The increase of vascular attenuation on the other hand side is supposed to compensate for this and hence all available studies report on a constantly high SNR or CNR when comparing high and low kV CTPA protocols [28, 30, 32]. However, using a tube potential of 80 kV will emit an x-ray spectrum that is considered to be “soft” and hence less penetrable in body tissue. A standard use of 80 kV without tube current correction in unselected patients may be discussed controversially, as a clear dependency of image quality parameters on patient size is regularly seen [31, 33, 34], even with negative effect on diagnostic confidence [35]. Diagnostic confidence is essential for maintaining the accuracy and especially the high negative predictive value of CTPA and giving the strength of this test [6, 8, 36, 37]. Due to tube power and therefore maximum photon output restrictions, the use of 100 kV instead of 80 kV protocols seems to be the more practical way in clinical routine with the current generation of widely installed 16- and 64-slice CT bases [28, 30, 32]. Dose parameters (CTDIvol: 5 mGy [32], 6.1 mGy [30], 17.6 mGy [28]) and noise levels (14.8 HU [30], 16.9 HU [28], 34 HU [32]) reported for these 100 kV protocols tended to be low, but were within a wide range, although protocol parameters were very similar or identical in the utilized 16-slice CT devices. In front of this data, the results achieved in the underlying study with the 80 kV/Sn140 kV configuration with the second generation of DECT with a mean CTDIvol of 6.2 mGy and a mean background noise of 12 HU appear competitive.
On the other hand side, our data suggest that at least, if image noise is within a certain range as in the present study, the impact on subjective image quality as perceivable by the radiologist seems to be of minor importance. Although image noise was 92% higher in group 2 compared to group 4, only observer 1 scored image quality significantly better in the latter group, whereas both observers did not rate subjective image quality significantly differently in all other cases. Considering this important finding, a potential for further dose reduction with second generation DECT with the 80 kV/Sn140 kV configuration by lowering mAs values seems to be given. The adoption of recently introduced iterative raw data reconstruction algorithms may contribute additional benefits in this context.
Some limitations of our study need to be addressed. First, by its retrospective nature, some patient-based factors that may confound our results may not have been recognized. Second, since 15 ml more contrast material were injected in group 1 compared to the other groups, this had an impact on opacification of the segmental arteries of the upper lobe with influence on SNR. However, a small compact contrast bolus for DE CTPA with good washout of the upper venous system is essential to avoid artefacts of the pulmonary iodine distribution maps demanding sophisticated injection protocols. Overall image quality on the other side was not compromised in the dual-energy groups in our study.
In conclusion, CTPA is feasible without additional dose exposure or loss of perceivable image quality with both first (140 kV/80 kV) and second (100 kV/Sn140 kV) generation dual-energy CT compared to a standard 120 kV 64-slice protocol in a clinical routine setting. With the use of the 80 kV/Sn140 kV configuration of second generation DECT dose exposure can even be significantly lowered without loss of image quality and should therefore be preferably applied. An actually better noise profile with this configuration may leave room for a further reduction in dose by reducing tube current settings.
References
Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ (1998) Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 158:585–593
Tapson VF (2008) Acute pulmonary embolism. N Engl J Med 358:1037–1052
Dalen JE (2002) Pulmonary embolism: what have we learned since Virchow? Natural history, pathophysiology, and diagnosis. Chest 122:1440–1456
Dauphine C, Omari B (2005) Pulmonary embolectomy for acute massive pulmonary embolism. Ann Thorac Surg 79:1240–1244
Ota M, Nakamura M, Yamada N, Yazu T, Ishikura K, Hiraoka N, Tanaka H, Fujioka H, Isaka N, Nakano T (2002) Prognostic significance of early diagnosis in acute pulmonary thromboembolism with circulatory failure. Heart Vessels 17:7–11
Remy-Jardin M, Pistolesi M, Goodman LR, Gefter WB, Gottschalk A, Mayo JR, Sostman HD (2007) Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology 245:315–329
Schaefer-Prokop C, Prokop M (2005) MDCT for the diagnosis of acute pulmonary embolism. Eur Radiol 15(Suppl 4):D37–D41
Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galie N, Pruszczyk P, Bengel F, Brady AJ, Ferreira D, Janssens U, Klepetko W, Mayer E, Remy-Jardin M, Bassand JP, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Zamorano JL, Andreotti F, Ascherman M, Athanassopoulos G, De Sutter J, Fitzmaurice D, Forster T, Heras M, Jondeau G, Kjeldsen K, Knuuti J, Lang I, Lenzen M, Lopez-Sendon J, Nihoyannopoulos P, Perez Isla L, Schwehr U, Torraca L, Vachiery JL (2008) Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J 29:2276–2315
Petersilka M, Bruder H, Krauss B, Stierstorfer K, Flohr TG (2008) Technical principles of dual source CT. Eur J Radiol 68:362–368
Johnson TR, Krauss B, Sedlmair M, Grasruck M, Bruder H, Morhard D, Fink C, Weckbach S, Lenhard M, Schmidt B, Flohr T, Reiser MF, Becker CR (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17:1510–1517
Zatz LM (1976) The effect of the kVp level on EMI values. Selective imaging of various materials with different kVp settings. Radiology 119:683–688
Bauer RW, Kerl JM, Weber E, Weisser P, Korkusuz H, Lehnert T, Jacobi V, Vogl TJ (2010) Lung perfusion analysis with dual energy CT in patients with suspected pulmonary embolism—influence of window settings on the diagnosis of underlying pathologies of perfusion defects. Eur J Radiol. doi:10.1016/j.ejrad.2010.09.009
Fink C, Johnson TR, Michaely HJ, Morhard D, Becker C, Reiser MF, Nikolaou K (2008) Dual-energy CT angiography of the lung in patients with suspected pulmonary embolism: initial results. Rofo 180:879–883
Pontana F, Faivre JB, Remy-Jardin M, Flohr T, Schmidt B, Tacelli N, Pansini V, Remy J (2008) Lung perfusion with dual-energy multidetector-row CT (MDCT): feasibility for the evaluation of acute pulmonary embolism in 117 consecutive patients. Acad Radiol 15:1494–1504
Thieme SF, Becker CR, Hacker M, Nikolaou K, Reiser MF, Johnson TR (2008) Dual energy CT for the assessment of lung perfusion—correlation to scintigraphy. Eur J Radiol 68:369–374
Thieme SF, Johnson TR, Lee C, McWilliams J, Becker CR, Reiser MF, Nikolaou K (2009) Dual-energy CT for the assessment of contrast material distribution in the pulmonary parenchyma. Am J Roentgenol 193:144–149
Zhang LJ, Chai X, Wu SY, Zhao YE, Hu XB, Hu YX, Xue YB, Yang GF, Zhu H, Lu GM (2009) Detection of pulmonary embolism by dual energy CT: correlation with perfusion scintigraphy and histopathological findings in rabbits. Eur Radiol 19:2844–2854
Ferda J, Ferdova E, Mirka H, Baxa J, Bednarova A, Flohr T, Schmidt B, Matejovic M, Kreuzberg B (2009) Pulmonary imaging using dual-energy CT, a role of the assessment of iodine and air distribution. Eur J Radiol. doi:10.1016/j.ejrad.2009.08.005
Pansini V, Remy-Jardin M, Faivre JB, Schmidt B, Dejardin-Bothelo A, Perez T, Delannoy V, Duhamel A, Remy J (2009) Assessment of lobar perfusion in smokers according to the presence and severity of emphysema: preliminary experience with dual-energy CT angiography. Eur Radiol. doi:10.1007/s00330-009-1475-6
Pontana F, Remy-Jardin M, Duhamel A, Faivre JB, Wallaert B, Remy J (2010) Lung perfusion with dual-energy multi-detector row CT: can it help recognize ground glass opacities of vascular origin? Acad Radiol 17:587–594
Brenner DJ, Hall EJ (2007) Computed tomography—an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Mettler FA Jr, Wiest PW, Locken JA, Kelsey CA (2000) CT scanning: patterns of use and dose. J Radiol Prot 20:353–359
Wiest PW, Locken JA, Heintz PH, Mettler FA (2002) CT scanning: a major source of radiation exposure. Semin Ultrasound CT MR 23:402–410
Schenzle JC, Sommer WH, Neumaier K, Michalski G, Lechel U, Nikolaou K, Becker CR, Reiser MF, Johnson TR (2010) Dual energy CT of the chest: how about the dose? Invest Radiol 45:347–353
Dodd JD, Kalva S, Pena A, Bamberg F, Shapiro MD, Abbara S, Cury RC, Brady TJ, Hoffmann U (2008) Emergency cardiac CT for suspected acute coronary syndrome: qualitative and quantitative assessment of coronary, pulmonary, and aortic image quality. Am J Roentgenol 191:870–877
Halpern EJ (2009) Triple-rule-out CT angiography for evaluation of acute chest pain and possible acute coronary syndrome. Radiology 252:332–345
Wittram C (2007) How I do it: CT pulmonary angiography. Am J Roentgenol 188:1255–1261
Heyer CM, Mohr PS, Lemburg SP, Peters SA, Nicolas V (2007) Image quality and radiation exposure at pulmonary CT angiography with 100- or 120-kVp protocol: prospective randomized study. Radiology 245:577–583
Schueller-Weidekamm C, Schaefer-Prokop CM, Weber M, Herold CJ, Prokop M (2006) CT angiography of pulmonary arteries to detect pulmonary embolism: improvement of vascular enhancement with low kilovoltage settings. Radiology 241:899–907
Szucs-Farkas Z, Kurmann L, Strautz T, Patak MA, Vock P, Schindera ST (2008) Patient exposure and image quality of low-dose pulmonary computed tomography angiography: comparison of 100- and 80-kVp protocols. Invest Radiol 43:871–876
Szucs-Farkas Z, Verdun FR, von Allmen G, Mini RL, Vock P (2008) Effect of X-ray tube parameters, iodine concentration, and patient size on image quality in pulmonary computed tomography angiography: a chest-phantom-study. Invest Radiol 43:374–381
Bjorkdahl P, Nyman U (2010) Using 100- instead of 120-kVp computed tomography to diagnose pulmonary embolism almost halves the radiation dose with preserved diagnostic quality. Acta Radiol 51:260–270
Sigal-Cinqualbre AB, Hennequin R, Abada HT, Chen X, Paul JF (2004) Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology 231:169–174
Szucs-Farkas Z, Strautz T, Patak MA, Kurmann L, Vock P, Schindera ST (2009) Is body weight the most appropriate criterion to select patients eligible for low-dose pulmonary CT angiography? Analysis of objective and subjective image quality at 80 kVp in 100 patients. Eur Radiol 19:1914–1922
MacKenzie JD, Nazario-Larrieu J, Cai T, Ledbetter MS, Duran-Mendicuti MA, Judy PF, Rybicki FJ (2007) Reduced-dose CT: effect on reader evaluation in detection of pulmonary embolism. Am J Roentgenol 189:1371–1379
Quiroz R, Kucher N, Zou KH, Kipfmueller F, Costello P, Goldhaber SZ, Schoepf UJ (2005) Clinical validity of a negative computed tomography scan in patients with suspected pulmonary embolism: a systematic review. JAMA 293:2012–2017
Schoepf UJ, Costello P (2004) CT angiography for diagnosis of pulmonary embolism: state of the art. Radiology 230:329–337
Acknowledgements
Dr. Ralf Bauer and Dr. J. Kerl are research consultants and representatives of the Speaker’s Bureau of Siemens Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bauer, R.W., Kramer, S., Renker, M. et al. Dose and image quality at CT pulmonary angiography—comparison of first and second generation dual-energy CT and 64-slice CT. Eur Radiol 21, 2139–2147 (2011). https://doi.org/10.1007/s00330-011-2162-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2162-y